Abstract
Background
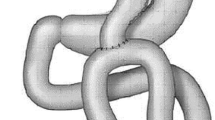
Mini gastric bypass (MGB) is a promising and attractive alternative bariatric procedure. In 2011, we introduced MGB in our high-volume bariatric unit. Subsequently, we evaluated short- and midterm results of this procedure.
Methods
A prospective cohort of patients who underwent MGB between 2012 and 2013 was retrospectively evaluated.
Results
From 2012 to 2013, primary MGB was performed in 287 patients with a mean BMI of 42 kg/m2 (range 32–76 kg/m2). The mean operation time was 50 min (range 25–120 min). The mortality rate was 0%. Serious complications, such as leakage, pulmonary embolism, or bleeding, occurred in 3.1% of patients; anastomotic leaks occurred in 1.4% of patients. Conversion to Roux-en-Y gastric bypass for biliary reflux or other indications occurred in six patients (2%). During our initial learning phase, biliary reflux rates were higher due to an overly short pouch. Surgical revision for malnutrition was performed in one patient. Percent excess weight loss and percent total body weight loss were 85 and 35%, respectively, after 1 year; 88 and 36.6%, respectively, after 2 years; and 83 and 34.3%, respectively, after 3 years. Follow-up rates after 1, 2, and 3 years were 96% (277/287), 72% (208/287), and 66% (190/287), respectively.
Conclusions
As a primary bariatric procedure, MGB is associated with good early and midterm results. MGB has the potential to become a significant alternative bariatric procedure. Correct technique is of extreme importance when performing MGB; therefore, the appointment of an experienced MGB surgeon as a guide when beginning to utilize this technique is advised.



Similar content being viewed by others
References
World Health Organization (2015) Media centre factsheet N311, obesity and overweight. World Health Organization, Geneva. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed Jan 2015
Buchwald H, Avidor Y, Braunwald E et al (2004) Bariatric surgery. A systematic review and meta-analysis. JAMA 292:1724–1737
Adams TD, Gress RE, Smith SC et al (2007) Long-term mortality after gastric bypass surgery. N Engl J Med 357:753–761
Sjostrom L, Narbro K, Sjostrom CD et al (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 357:741–752
Christou NV, Sampalis JS, Liberman M et al (2004) Surgery decreases long-term mortality, morbidity and health care use in morbidly obese patients. Ann Surg 240:416–424
Flum DR, Dellinger EP (2004) Impact of gastric bypass operation on survival. A population-based analysis. J Am Coll Surg 199:543–555
Pories WJ, Swanson MS, MacDonald KG et al (1995) Who would have thought of it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 222:339–352
Angrisani L et al (2015) Bariatric surgery worldwide 2013. Obes Surg 25(10):1822–1832. https://doi.org/10.1007/s11695-015-1657-z
Deitel M. Letter (2015) Bariatric surgery worldwide 2013 reveals a rise in mini gastric bypass. Obes Surg 25:2165
Rutledge R (2001) The mini-gastric bypass: experience with first 1,274 cases. Obes Surg 11:276–280
Fisher BL et al (2001) Mini gastric bypass controversy. Obes Surg 11(6):773–777
Mahawar KK, Carr WR, Balupuri S, Small PK (2014) Controversy surrounding ‘mini’ gastric bypass. Obes Surg 24(2):324–333. https://doi.org/10.1007/s11695-013-1090-0 (Review)
Musella M, Milone M (2014) Still “controversies” about the mini gastric bypass? Obes Surg 24:643–644
Mahawar KK, Carr WRJ, Jennings N, Balupuri S, Small PK (2014) Reply to “still controversies after mini gastric bypass”. Obes Surg 24:645–646
Garcia-Caballero M, Carbalo M (2004) One anastomosis gastric bypass: a simple, safe and efficient procedure for treating morbid obesity. Nutr Hosp 19:372–375
Carbajo M, Garcia-Caballero M, Toledano M, Osorio D, Garacia-Lanza C, Carmona JA (2005) One-anastomosis gastric bypass by laparoscopy: results of the first 209 patients. Obes Surg 15:398–404
Lee WJ, Yu PJ, Wang W, Chen TC, Wei PL, Huang MT (2005) Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg 242:20–28
Lee WJ, Ser KH, Lee YC, Tsou JJ, Chen SC, Chen JC (2012) Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg 22:1827–1834
Musella M, Apers J, Rheinwalt K, Ribeiro R, Manno E, Greco F, Milone M, Di Stefano C, Guler S, Van Lessen IM, Guerra A, Maglio MN, Bonfanti R, Novotna R, Coretti G, Piazza L (2015) Efficacy of bariatric surgery in type 2 diabetes mellitus remission: the role of mini gastric bypass/one anastomosis gastric bypass and sleeve gastrectomy at 1 year of follow-up. A European survey. Obes Surg. https://doi.org/10.1007/s11695-015-1865-6
Rutledge R, Walsh W (2005) Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg 15:1304–1308
Peraglie C (2008) Laparoscopic minigastric bypass (LMGB) in the super-super obese: outcomes in 16 patients. Obes Surg 18:1126–1129
Peraglie C (2016) Laparoscopic mini-gastric bypass in patients age 60 and older. Surg Endosc 30:38–43
Lee WJ, Lee YC, Ser KH, Chen SC, Su YH (2011) Revisional surgery for laparoscopic minigastric bypass. Surg Obes Relat Dis 7:486–491
Weiner RA, Theodoridou S, Weiner S (2011) Failure of laparoscopic sleeve gastrectomy—further procedure?. Obes Facts 4(Suppl 1):42–46
Moszkowicz D, Rau C, Guennzi M, Zinzindohoue F, Berger A, Chevallier JM (2013) Laparoscopic omega-loop gastric bypass for the conversion of failed sleeve gastrectomy: early experience. J Vis Surg 150:373–378
Lönroth H (1998) Laparoscopic gastric bypass. Obes Surg 8(6):563–565
Lee WJ, Wang W, Lee YC, Huang MT, Ser KH, Chen JC (2008) Laparoscopic mini-gastric bypass: experience with tailored bypass limb according to body weight. Obes Surg 18:294–299
Bergland A, Gislason H, Raeder J (2008) Fast-track surgery for bariatric laparoscopic gastric bypass with focus on anaesthesia and peri-operative care. Experience with 500 cases. Acta Anaesthesiol Scand 52(10):1394–1399
Coblijn UK, Lagarde SM, de Castro SM, Kuiken SD, van Tets WF, van Wagensveld BA (2016) The influence of prophylactic proton pump inhibitor treatment on the development of symptomatic marginal ulceration in Roux-en-Y gastric bypass patients: a historic cohort study. Surg Obes Relat Dis 12(2):246–252. https://doi.org/10.1016/j.soard.2015.04.022
Kular KS, Manchanda N, Rutledge R (2014) A 6-year experience with 1,054 mini-gastric bypasses—first study from Indian subcontinent. Obes Surg 24:143
Chevallier JM, Arman GA, Guenzi M, Rau C, Bruzzi M, Beaupel N, Zinzindohoué F, Berger A (2015) One thousand single anastomosis (omega loop) gastric bypasses to treat morbid obesity in a 7-year period: outcomes show few complications and good efficacy. Obes Surg 25:951–958
American Diabetes Association (2012) Standards of medical care in diabetes 2012. Diabetes Care 35:S11–S63
Noun R, Skaff J, Riachi E, Daher R, Antoun NA, Nasr M (2012) One thousand consecutive mini-gastric bypass: short and long-term outcome. Obes Surg 22:697–703
Facchiano E, Leuratti L, Veltri M, Lucchese M (2016) Laparoscopic conversion of one anastomosis gastric bypass to Roux-en-Y gastric bypass for chronic bile reflux. Obes Surg. https://doi.org/10.1007/s11695-015-2017-8
Deitel M (2013) Mini-gastric (one-anastomosis) bypass becoming a mainstream operation. In: Bariatr News issue 18, p 13
Acknowledgements
We would like to thank Dr. M. Dunkelgrun for his contributions to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
J. Apers, R. Wijkmans, M. Emous, and E. Totte have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Apers, J., Wijkmans, R., Totte, E. et al. Implementation of mini gastric bypass in the Netherlands: early and midterm results from a high-volume unit. Surg Endosc 32, 3949–3955 (2018). https://doi.org/10.1007/s00464-018-6136-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6136-x