Abstract
Background
Three-dimensional (3D) systems for laparoscopy provide surgeons with additional information on spatial depth not found in two-dimensional (2D) systems.
Methods
This study enrolled 156 spleen-preserving splenic hilar lymphadenectomy (LSPSHL) patients in a randomized controlled trial (ClinicalTrials.gov Identifier NCT02327481) at the department of gastric surgery at Fujian Medical University Union Hospital between January 2015 and April 2016. The short-term efficacies were compared between the treatment groups. The unedited videos of 80 LSPSHL (40 procedures each for 3D and 2D) were rated for technical performance using the Generic Error Rating Tool.
Results
The data for 156 LSPSHL patients indicate that the estimated blood loss (EBL) (3D vs 2D = 66.3 vs. 99.0, P = 0.046) was significantly less in the 3D group. The postoperative recovery and complication rates were similar (P > 0.05). And there were no deaths within 30 days of surgery. Two observers analyzed 80 videos of LSPSHL. The results showed that there were fewer grasping-errors made in the 3D group than in the 2D group when dissecting the inferior pole region of spleen (IPRS) (P = 0.016) and the superior pole region of spleen (SPRS) (P = 0.022). Additionally, the inter-rater reliability was high regarding grasping-errors in the IPRS (intraclass correlation coefficient (ICC) 0.92) and in the SPRS (ICC 0.83). The ICC for the total number of errors was 0.82. The mean of errors in the 3D group (3D vs. 2D = 20.7 vs. 23.5, P = 0.022) was less than the 2D group.
Conclusions
Compared with 2D LSPSHL, 3D technology reduces EBL and technical errors during splenic hilar dissection.


Similar content being viewed by others
References
Kitano S, Iso Y, Moriyama M et al (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4(2):146–148
Hyung WJ, Lim JS, Song J et al (2008) Laparoscopic spleen-preserving splenic hilar lymph node dissection during total gastrectomy for gastric cancer. J Am Coll Surg 207(2):e6–e11
Shah J, Buckley D, Frisby J et al (2003) Depth cue reliance in surgeons and medical students. Surg Endosc Other Interv Techniq 17(9):1472–1474
Mather G, Smith DR (2000) Depth cue integration: stereopsis and image blur. Vision Res 40(25):3501–3506
Voorhorst FA, Overbeeke KJ, Smets GJ (1996) Using movement parallax for 3D laparoscopy. Med Prog Technol 21(4):211
Storz P, Buess GF, Kunert W (2012) 3D HD versus 2D HD: surgical task efficiency in standardised phantom tasks. Surg Endosc 26(5):1454–1460
Aykan S, Singhal P, Nguyen DP et al (2014) Perioperative, pathologic, and early continence outcomes comparing three-dimensional and two-dimensional display systems for laparoscopic radical prostatectomy–a retrospective, single-surgeon study. J Endourol 28(5):539–543
Gaudissart Q, Cadière GB, Nyssen AS (2007) Comparison of learning curves and skill transfer between classical and robotic laparoscopy according to the viewing conditions: implications for training. Am J Surg 194(1):115–121
Chiu CJ, Prabhu KL, Tan-Tam CH et al (2015) Using three-dimensional laparoscopy as a novel training tool for novice trainees compared with two-dimensional laparoscopy. Am J Surg 209(5):824–827.e1
Alaraimi B, Bakbak WE, Sarker S et al (2014) A randomized prospective study comparing acquisition of laparoscopic skills in three-dimensional (3D) vs. two-dimensional (2D) laparoscopy. World J Surg 38(11):2746–2752
Smith R, Day A, Rockall T et al (2012) Advanced stereoscopic projection technology significantly improves novice performance of minimally invasive surgical skills. Surg Endosc 26(6):1522–1527
Usta TA, Ozkaynak A, Kovalak E et al (2015) An assessment of the new generation three-dimensional high definition laparoscopic vision system on surgical skills: a randomized prospective study. Surg Endosc 29(8):2305–2313
Zheng CH, Lu J, Zheng HL et al. Comparison of 3D laparoscopic gastrectomy with a 2D procedure for gastric cancer: A phase 3 randomized controlled trial. Surgery 2018; 163(2)
Japanese Gastric Cancer A (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14(2):113–123
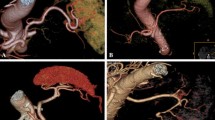
Huang CM, Chen QY, Lin JX et al (2014) Huang’s three-step maneuver for laparoscopic spleen-preserving No. 10 lymph node dissection for advanced proximal gastric cancer. Chin J Cancer Res 26(2):208–210
Huang CM, Huang ZN, Zheng CH et al (2017) Huang’s three-step maneuver shortens the learning curve of laparoscopic spleen-preserving splenic hilar lymphadenectomy. Surg Oncol 26(4):389
de Steur WO, Hartgrink HH, Dikken JL et al (2015) Quality control of lymph node dissection in the Dutch Gastric Cancer Trial. Br J Surg 102(11):1388–1393
Wente MN, Veit JA, Bassi C et al (2007) Postpancreatectomy hemorrhage (PPH)—an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25
Bissolati M, Socci C, Orsenigo E et al (2012) Duodenal stump fistula after gastric surgery for malignancy. A retrospective analysis of risk factors in a single-center experience. Eur J Surg Oncol 38(10):987–987
Bonrath EM, Zevin B, Dedy NJ et al (2013) Error rating tool to identify and analyse technical errors and events in laparoscopic surgery. Br J Surg 100(8):1080–1088
Fecso AB, Bhatti JA, Stotland PK et al. Technical Performance as a Predictor of Clinical Outcomes in Laparoscopic Gastric Cancer Surgery. Ann Surg 2018:1
J R. Understanding adverse events: human factors. Qual Health Care Qhc 1995; 4(2):80
Buess G, Theiss R, Günther M et al (1985) Endoscopic surgery in the rectum. Endoscopy 17(01):31–35
Byrn JC, Schluender S, Divino CM et al (2007) Three-dimensional imaging improves surgical performance for both novice and experienced operators using the da Vinci Robot System. Am J Surg 193(4):519–522
Parker AJ (2007) Binocular depth perception and the cerebral cortex. Nat Rev Neurosci 8(5):379–391
Gómezgómez E, Carrascovaliente J, Valerorosa J et al (2015) Impact of 3D vision on mental workload and laparoscopic performance in inexperienced subjects. Actas Urol Esp 39(4):229–235
G M. From 2D to 3D: the future of surgery? Lancet 2011; 378(9800):1368–1368
Kong SH, Oh BM, Yoon H et al (2010) Comparison of two- and three-dimensional camera systems in laparoscopic performance: a novel 3D system with one camera. Surg Endosc 24(5):1132–1143
S N, L S, D M, et al. Augmented reality in laparoscopic surgical oncology. Surg Oncol 2011; 20(3):189–201
Osborn DA (1967) Errors in blood transfusion. BMJ 4(5578):550–551
HN B, PG P (1966) Iatrogenic factors in infectious disease. Ann Intern Med 65(4):641
org.cambridge.ebooks.online.book.Author@cfc. Human Error. 1990
Kohn LT, Corrigan J, Donaldson MS (2000) To err is human: building a safer health system. Annales Franaises Danesthèsie Et De Rèanimation 6(6):453–454 21(
Taffinder N, Smith SGT, Huber J et al (1999) The effect of a second-generation 3D endoscope on the laparoscopic precision of novices and experienced surgeons. Surg Endosc 13(11):1087–1092
Smith R, Schwab K, Day A et al (2015) Effect of passive polarizing three-dimensional displays on surgical performance for experienced laparoscopic surgeons. Br J Surg 101(11):1453–1459
Cicione A, Autorino R, Breda A et al (2013) Three-dimensional vs standard laparoscopy: comparative assessment using a validated program for laparoscopic urologic skills. Urology 82(6):1444–1450
dL MR, DJ JC (2000) W, et al. Human factors and cardiac surgery: a multicenter study. J Thor Cardiovasc Surg 119(4):661–672
Acknowledgements
This work was supported by Scientific and Technological Innovation Joint Capital Projects of Fujian Province, China (No. 2016Y9031), the Construction Project of Fujian Province Minimally Invasive Medical Center (No. [2017]171), the second batch of special support funds for Fujian Province Innovation and Entrepreneurship Talents (2016B013), the Youth Project of Fujian Provincial Health and Family Planning Commission (2016-1-41), the Nature Fund Health Joint Fund Project of Fujian Province (2015J01464), Fujian Province Medical Innovation Project (2015-CXB-16) and Chinese Physicians Association Young Physician Respiratory Research Fund.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Zhi-Yu Liu, Qi-Yue Chen, Qing Zhong, Ping Li, Jian-Wei Xie, Jia-Bin Wang, Jian-Xian Lin, Jun Lu, Long-Long Cao, Mi Lin, Ru-Hong Tu, Ze-Ning Huang, Ju-Li Lin, Hua-Long Zheng, Chang-Ming Huang, Chao-Hui Zheng have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
464_2018_6640_MOESM1_ESM.tif
(A) Overall survival of spleen hilar lymphadenectomy (n = 156). (B) Recurrence-free survival of spleen hilar lymphadenectomy (n = 156). (TIF 408 KB)
464_2018_6640_MOESM5_ESM.tif
No difference in the D2 lymphadenectomy noncompliance rate was demonstrated among these subgroups (A: Noncompliance rate of nodal dissection (pT), PpT1=0.380, PpT2 = 0.101, PpT3 = 1, PpT4 = 0.752, PTotal = 0.831). (B: Noncompliance rate of nodal dissection (pN), PN0 = 0.853, PN1 = 0.675, PN2 = 0.398, PN3 = 0.051, PTotal = 0.831). (C: Noncompliance rate of nodal dissection (pTNM stage), PI = 1, PII = 0.711, PIII = 0.348, PTotal = 0.831). (D: Noncompliance rate of nodal dissection (BMI), PBMI<18 =1, P18≤BMI<25 =0.713, PBMI≥25 =0.705, PTotal = 0.831). (TIF 4810 KB)
Rights and permissions
About this article
Cite this article
Liu, ZY., Chen, QY., Zhong, Q. et al. Is three-dimensional laparoscopic spleen preserving splenic hilar lymphadenectomy for gastric cancer better than that of two-dimensional? Analysis of a prospective clinical research study. Surg Endosc 33, 3425–3435 (2019). https://doi.org/10.1007/s00464-018-06640-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-06640-7