Abstract
Background
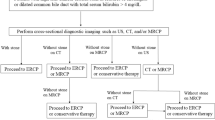
Numerous models have been developed to predict choledocholithiasis. Recent work has shown that these algorithms perform suboptimally. Identification of clinical predictors with high positive and negative predictive value would minimize adverse events associated with unnecessary diagnostic endoscopic retrograde cholangiopancreatography (ERCP) while limiting the use of expensive tests including magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS) for indeterminate cases.
Methods
Consecutive unique inpatients who received their first ERCP at Los Angeles County Medical Center between January 2010 and November 2016 for suspected bile duct stones were reviewed. The primary outcome was the proportion of patients with specific combinations of liver enzyme patterns, transabdominal ultrasound, and clinical features who had stones confirmed on ERCP. As a secondary outcome, we assessed the performance of the American Society for Gastrointestinal Endoscopy (ASGE) risk stratification algorithm in our population.
Results
Of the 604 included patients, bile duct stones were confirmed in 410 (67.9%). Detailed assessment of liver enzyme patterns alone and in combination with clinical features and imaging findings yielded no highly predictive algorithms. Additionally, the ASGE high-risk criterion had a positive predictive value of only 68% for stones. For the 236 patients for whom MRCP was performed, this imaging modality was shown to have highest predictive value for the presence of stones on ERCP.
Conclusion
Exhaustive exploration of various threshold values and dynamic patterns of liver enzymes combined with clinical features and basic imaging findings did not reveal an algorithm to accurately predict the presence of stones on ERCP. The ASGE risk stratification criteria were also insensitive in our population. Though desirable, there may be no “perfect” combination of clinical features that correlate with persistent bile duct stones. MRCP or EUS may be considered to avoid unnecessary ERCP and associated complications.

Similar content being viewed by others
References
Szary NM, Al-Kawas FH (2013) Complications of endoscopic retrograde cholangiopancreatography: how to avoid and manage them. Gastroenterol Hepatol 9:496–504
Loperfido S, Angelini G, Benedetti G et al (1998) Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 48:1–10
Masci E, Toti G, Mariani A et al (2001) Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol 96:417–423
Barkun AN, Barkun JS, Fried GM et al (1994) Useful predictors of bile duct stones in patients undergoing laparoscopic cholecystectomy. McGill Gallstone Treatment Group. Ann Surg 220:32–39
Arguedas MR, Dupont AW, Wilcox CM (2001) Where do ERCP, endoscopic ultrasound, magnetic resonance cholangiopancreatography, and intraoperative cholangiography fit in the management of acute biliary pancreatitis? A decision analysis model. Am J Gastroenterol 96:2892–2899
Maple JT, Ben-Menachem T, Anderson MA et al (2010) The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc 71:1–9
Suarez AL, LaBarre NT, Cotton PB, Payne KM, Cote GA, Elmunzer BJ (2016) An assessment of existing risk stratification guidelines for the evaluation of patients with suspected choledocholithiasis. Surg Endosc 30:4613–4618
Adams MA, Hosmer AE, Wamsteker EJ et al (2015) Predicting the likelihood of a persistent bile duct stone in patients with suspected choledocholithiasis: accuracy of existing guidelines and the impact of laboratory trends. Gastrointest Endosc 82:88–93
He H, Tan C, Wu J et al (2017) Accuracy of ASGE high-risk criteria in evaluation of patients with suspected common bile duct stones. Gastrointest Endosc 86:525–532
Canto MI, Chak A, Stellato T, Sivak MV Jr (1998) Endoscopic ultrasonography versus cholangiography for the diagnosis of choledocholithiasis. Gastrointest Endosc 47:439–448
Polkowski M, Regula J, Tilszer A, Butruk E (2007) Endoscopic ultrasound versus endoscopic retrograde cholangiography for patients with intermediate probability of bile duct stones: a randomized trial comparing two management strategies. Endoscopy 39:296–303
Kiriyama S, Takada T, Strasberg SM et al (2012) New diagnostic criteria and severity assessment of acute cholangitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci 19:548–556
Yang MH, Chen TH, Wang SE et al (2008) Biochemical predictors for absence of common bile duct stones in patients undergoing laparoscopic cholecystectomy. Surg Endosc 22:1620–1624
Robertson GS, Jagger C, Johnson PR et al (1996) Selection criteria for preoperative endoscopic retrograde cholangiopancreatography in the laparoscopic era. Arch Surg 131:89–94
Santucci L, Natalini G, Sarpi L, Fiorucci S, Solinas A, Morelli A (1996) Selective endoscopic retrograde cholangiography and preoperative bile duct stone removal in patients scheduled for laparoscopic cholecystectomy: a prospective study. Am J Gastroenterol 91:1326–1330
Narjes H, Nehmiz G (2000) Effect of hospitalisation on liver enzymes in healthy subjects. Eur J Clin Pharmacol 56:329–333
Tetangco EP, Shah N, Arshad HM, Raddawi H (2016) Markedly elevated liver enzymes in choledocholithiasis in the absence of hepatocellular disease: case series and literature review. J Investig Med High Impact Case Rep https://doi.org/10.1177/2324709616651092
Snape WJ Jr, Long WB, Trotman BW, Marin GA, Czaja AJ (1976) Marked alkaline phosphatase elevation with partial common bile duct obstruction due to calcific pancreatitis. Gastroenterology 70:70–73
Bachar GN, Cohen M, Belenky A, Atar E, Gideon S (2003) Effect of aging on the adult extrahepatic bile duct: a sonographic study. J Ultrasound Med 22:879–882 (quiz 83–85)
Krawczyk M, Wang DQ, Portincasa P, Lammert F (2011) Dissecting the genetic heterogeneity of gallbladder stone formation. Semin Liver Dis 31:157–172
Gross BH, Harter LP, Gore RM et al (1983) Ultrasonic evaluation of common bile duct stones: prospective comparison with endoscopic retrograde cholangiopancreatography. Radiology 146:471–474
Chang L, Lo S, Stabile BE, Lewis RJ, Toosie K, de Virgilio C (2000) Preoperative versus postoperative endoscopic retrograde cholangiopancreatography in mild to moderate gallstone pancreatitis: a prospective randomized trial. Ann Surg 231:82–87
Chang L, Lo SK, Stabile BE, Lewis RJ, de Virgilio C (1998) Gallstone pancreatitis: a prospective study on the incidence of cholangitis and clinical predictors of retained common bile duct stones. Am J Gastroenterol 93:527–531
Cohen ME, Slezak L, Wells CK, Andersen DK, Topazian M (2001) Prediction of bile duct stones and complications in gallstone pancreatitis using early laboratory trends. Am J Gastroenterol 96:3305–3311
Rubin MI, Thosani NC, Tanikella R, Wolf DS, Fallon MB, Lukens FJ (2013) Endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis: testing the current guidelines. Dig Liver Dis 45:744–749
Magalhaes J, Rosa B, Cotter J (2015) Endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis: from guidelines to clinical practice. World J Gastrointest Endosc 7:128–134
Badger WR, Borgert AJ, Kallies KJ, Kothari SN (2017) Utility of MRCP in clinical decision making of suspected choledocholithiasis: an institutional analysis and literature review. Am J Surg 214:251–255
Sharma R, Menachery J, Choudhary NS, Kumar M, Puri R, Sud R (2015) Routine endoscopic ultrasound in moderate and indeterminate risk patients of suspected choledocholithiasis to avoid unwarranted ERCP: a prospective randomized blinded study. Indian J Gastroenterol 34:300–304
Author information
Authors and Affiliations
Contributions
CYY, NR, JB: concept and design. CYY, NR, NJ, JB: acquisition of data. CYY, NR, JB: statistical analysis and interpretation of data. CYY, NR, NJ, JC, JVD, RS, JB: drafting and revision of manuscript.
Corresponding author
Ethics declarations
Disclosures
Drs. Chung Yao Yu, Nitzan Roth, Niraj Jani, Jaehoon Cho, Jacques Van Dam, Rick Selby, and James Buxbaum have no conflicts of interest or financial ties to disclose.
Appendix
Appendix
See Tables 5, 6, 7, 8, 9, and 10.
Rights and permissions
About this article
Cite this article
Yu, C.Y., Roth, N., Jani, N. et al. Dynamic liver test patterns do not predict bile duct stones. Surg Endosc 33, 3300–3313 (2019). https://doi.org/10.1007/s00464-018-06620-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-06620-x