Abstract
Background
The trend towards laparoscopic surgery seen in other specialties has not occurred at the same pace in oesophagectomy. This stems from concerns regarding compromised oncological clearance, and complications associated with gastric tube necrosis and anastomotic failure. We present our experience of minimally invasive oesophagectomy (MIO) compared to open and hybrid surgery. We aim to ascertain non-inferiority of MIO by evaluating impact on survival, oncological clearance by resection margin and lymph node harvest and post-operative complications.
Methods
Data were sourced retrospectively 2008–2015. Three approaches were studied. MIO (3-stage Mckeown), hybrid (2-stage Ivor Lewis, laparoscopy, thoracotomy) and open (2-stage Ivor Lewis).
Results
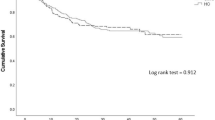
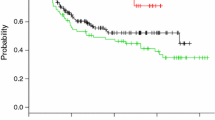
Five-year survival was 54.2%. Surgical approach had no significant impact on survival at any stage of disease (Stage 0/I p = 0.98; stage II p = 0.2; stage III p = 0.76). There was no statistically significant difference in oncological clearance by resection margins between procedures when compared by disease stage (p = 0.49). A higher number of nodes were harvested in hybrid [median 27.5 (6–65)] and open surgeries [median 26 (4–54)] than in MIO [median 20 (7–44)] (p > 0.01). Numbers of nodes resected did not impact risk of recurrence [recurrence, median 25 (6–54), no recurrence, 26 (4–65)] (p = 0.25). Anastomotic strictures (22.4%) and potential leaks (17.9%) were more common in MIO (strictures p > 0.01, leaks p = 0.08), although associated morbidity was lower. Respiratory complications were less common in MIO (2.9%) versus hybrid (13.3%) (p = 0.02). Wound infection and chyle leak were also lower (wound 1.5% MIO 3.5% open, p = 0.6; chyle leak 1.5% MIO, 6.7% hybrid, p = 0.2).
Conclusions
Our results show no negative impact of MIO on survival or oncological clearance. Respiratory and wound complications are lower in MIO, but rates of anastomotic strictures and potential anastomotic leaks are increased. This may be due to the longer length of conduit and subclinical ischaemia at the anastomosis and merits further evaluation.




Similar content being viewed by others
References
Allum WH, Blazeby JM, Griffin SM, On behalf of the Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland, the British Society of Gastroenterology and the British Association of Surgical Oncology et al (2011) Guidelines for the management of oesophageal and gastric cancer. Gut 60:1449e1472. doi:10.1136/gut.2010.228254
Chadwick G et al National Oesophago-gastric Cancer Audit (2010-2015) The Royal College of surgeons of England, Healthcare Quality Improvement Partnership Ltd. (HQIP), The Association of Upper GI surgeons (AUGIS), The British Society of Gastroenterology (BSG)
Veeramootoo D, Shore AC, Shields B et al (2010) Ischemic conditioning shows a time-dependent influence on the fate of the gastric conduit after minimally invasive esophagectomy. Surg Endosc 24(5):1126–1131. doi:10.1007/s00464-009-0739-1
www.cancerresearchuk.org > oesophageal cancer > survival. Accessed July 29 16
Portale G, Hagen JA, Peters JH et al (2005) Modern 5-year survival of resectable esophageal adenocarcinoma: single institution experience with 263 patients. j.jamcollsurg. doi:10.1016/j.jamcollsurg.2005.12.022
Burdall OC, Boddy AP, Fullick J et al (2015) A comparative study of survival after minimally invasive and open oesophagectomy. Surg Endosc 29(2):431–437. doi:10.1007/s00464-014-3694-4
Zhou C, Zhang L, Wang H et al (2015) Superiority of minimally invasive oesophagectomy in reducing in-hospital mortality of patients with resectable oesophageal cancer: a meta-analysis. PLoS One. doi:10.1371/journal.pone.0132889
Chan DS, Reid TD, Howell I, Lewis WG (2013) Systematic review and meta-analysis of the influence of circumferential resection margin involvement on survival in patients with operable oesophageal cancer. Br J Surg 100(4):456–464. doi:10.1002/bjs.9015
Sihag S, Wright CD, Wain JC et al (2012) Comparison of perioperative outcomes following open versus minimally invasive Ivor Lewis oesophagectomy at a single, high-volume centre. Eur J Cardiothorac Surg 42(3):430–437. doi:10.1093/ejcts/ezs031
Scottish Intercollegiate Guidelines Network (2006) Management of oesophageal and gastric cancer. A national clinical guideline. ISBN 1 899893 59 8. www.sign.ac.uk. Accessed 6 Jan 2017
Lagergren J, Mattsson F, Zylstra J et al (2016) Extent of lymphadenectomy and prognosis after esophageal cancer surgery. JAMA Surg 151(1):32–39. doi:10.1001/jamasurg.2015.2611
Biere SS, van Berge Henegouwen MI, Maas KW et al (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379(9829):1887–1892. doi:10.1016/S0140-6736(12)60516-9
Safranek PM, Cubitt J, Booth MI, Dehn TC (2010) Review of open and minimal access approaches to oesophagectomy for cancer. Br J Surg 97(12):1845–1853. doi:10.1002/bjs.7231
Zehetner J (2015) Intraoperative assessment of perfusion of the gastric graft and correlation with anastomotic leaks after esophagectomy. Ann Surg 262(1):74–78
Wormuth JK, Heitmiller RF (2006) Esophageal conduit necrosis. Thorac Surg Clin 2006(16):11–22
Hu H, Ye T, Zhang Y et al (2012) Modifications in retrosternal reconstruction after oesophagogastrectomy may reduce the incidence of anastomotic leakage. Eur J Cardiothorac Surg 42(2):359–363. doi:10.1093/ejcts/ezs015
Urschel JD (1995) Esophagogastrostomy anastomotic leaks complicating esophagectomy: a review. Am J Surg 169(6):634–640
Zhong S, Wu Q, Sun S et al (2014) Risk factors of benign anastomostic strictures after esophagectomy with cervical reconstruction. Zhonghua Wei Chang Wai Ke Za Zhi 17(9):877–880
Johansson J, Oberg S, Wenner J et al (2009) Impact of proton pump inhibitors on benign anastomotic stricture formations after esophagectomy and gastric tube reconstruction: results from a randomized clinical trial. Ann Surg 250(5):667–673. doi:10.1097/SLA.0b013e3181bcb139
Ruurda JP, van der Sluis PC, van der Horst S, van Hilllegersberg R (2015) Robot-assisted minimally invasive esophagectomy for esophageal cancer: a systematic review. J Surg Oncol 112:257–265. doi:10.1002/jso.23922
Van der Sluis PC, Ruurda JP, van der Horst S et al (2012) Robot-assisted minimally invasive thoraco-laparoscopic esophagectomy versus open transthoracic esophagectomy for resectable esophageal cancer, a randomized controlled trial (ROBOT trial). Trials 13:230. doi:10.1186/1745-6215-13-230
Acknowledgements
Sarah Trickett, Mike Goodman, Jane Wraight, Emma Chester (upper GI cancer clinical nurse specialists).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Laura Findlay, Caroline Yao, David Bennett, Richard Byrom and Nick Davies have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Findlay, L., Yao, C., Bennett, D.H. et al. Non-inferiority of minimally invasive oesophagectomy: an 8-year retrospective case series. Surg Endosc 31, 3681–3689 (2017). https://doi.org/10.1007/s00464-016-5406-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5406-8