Abstract
Background
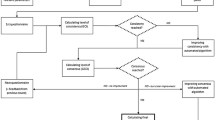
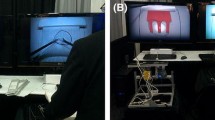
The FLS trainer lacks objective and automated assessments of laparoscopic performance and requires a large supply of relatively expensive consumables. Virtual reality simulation has a great potential as a training and assessment tool of laparoscopic skills and can overcome some limitations of the FLS trainer. This study was carried out to assess the value of our Virtual Basic Laparoscopic Surgical Trainer (VBLaST©) in the peg transfer task compared to the FLS trainer and its ability to differentiate performance between novice, intermediate, and expert groups.
Methods
Thirty subjects were divided into three groups: novices (PGY1-2, n = 10), intermediates (PGY3-4, n = 10), and experts (PGY5, surgical fellows and attendings, n = 10). All subjects performed ten trials of the peg transfer task on each simulator. Assessment of laparoscopic performance was based on FLS scoring while a questionnaire was used for subjective evaluation.
Results
The performance scores in the two simulators were correlated, though subjects performed significantly better in the FLS trainer. Experts performed better than novices only on the FLS trainer while no significant differences were observed between the other groups. Moreover, a significant learning effect was found on both trainers, with a greater improvement of performance on the VBLaST©. Finally, 82.6 % of the subjects preferred the FLS over the VBLaST© for surgical training which could be attributed to the novelty of the VR technology and existing deficiencies of the user interface for the VBLaST©.
Conclusion
This study demonstrated that the VBLaST© reproduced faithfully some aspects of the FLS peg transfer task (such as color, size, and shape of the peg board, etc.) while other aspects require additional development. Future improvement of the user interface and haptic feedback will enhance the value of the system as an alternative to the FLS as the standard training tool for laparoscopic surgery skills.





Similar content being viewed by others
References
Maithel S, Sierra R, Korndorffer J, Neumann P, Dawson S, Callery M, Jones D, Scott D (2006) Construct and face validity of MIST-VR, Endotower, and CELTS: are we ready for skills assessment using simulators? Surg Endosc 20(1):104–112
Munz Y, Kumar B, Moorthy K, Bann S, Darzi A (2004) Laparoscopic virtual reality and box trainers: is one superior to the other? Surg Endosc 18(3):485–494
Cao C, MacKenzie C, Payandeh S (1996) Task and motion analyses in endoscopic surgery. In: Proceedings of the ASME dynamic systems and controls division (fifth annual symposium on haptic interfaces for virtual environment and teleoperator systems)
Cao C, MacKenzie L, Payandeh S (1996) Precision and safety constraints in laparoscopic surgery. J Sport Exerc Psychol 18
Cao C, MacKenzie L (1997) Direct, 2-D vs. 3-D endoscopic viewing and surgical task performance. A symposium on evolving technologies: surgeons’ performance of surgical tasks. J Sport Exercise Psychol 19
Powers T, Murayama K, Toyama M, Murphy S, Denham E, Derossis A, Joehl R (2002) House staff performance is improved by participation in a laparoscopic skills curriculum. Am J Surg 184:626–629
Fried GM (2008) FLS assessment of competency using simulated laparoscopic tasks. J Gastrointest Surg 12(2):210–212
Fraser SA, Klassen DR, Feldman LS, Ghitulescu GA, Stanbridge D, Fried GM (2003) Valuating laparoscopic skills: setting the pass/fail score for the MISTELS system. Surg Endosc 17(6):964–967
Peters J, Fried G, Swanstrom L, Soper N, Sillin L, Schirmer B, Hoffman K, Committee SAGESFLS (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135(1):21–27
Botden S, Buzink S, Schijven MJJ (2007) Augmented versus virtual reality laparoscopic simulation: what is the difference? World J Surg 31(4):764–772
Grantcharov T, Rosenberg J, Pahle E, Fench P (2001) Virtual reality computer simulation. Surg Endosc 15:242–244
Reich O, Noll M, Gratzke C, Bachmann A, Waidelich R, Seitz M, Schlenker B, Baumgartner R, Hofstetter A, Stief C (2006) High-level virtual reality simulator for endourologic procedures of lower urinary tract. Urology 67(6):1144–1148
Dang T, Annaswamy T, Srinivasan M (2001) Development and evaluation of an epidural injection simulator with force feedback for medical training. Stud Health Technol Inform 81:97–102
Chellali A, Dumas C, Milleville-Pennel I (2012) Haptic communication to support biopsy procedures learning in virtual environments. Presence Teleoperators Virtual Environ 21(4):470–489
Panait L, Akkary E, Bell R, Roberts K, Dudrick S, Duffy A (2009) The role of haptic feedback in laparoscopic simulation training. J Surg Res 156(2):312–316
Seymour NE, Gallagher AG, Roman SA, O’Bri BMK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance results of a randomized, double-blinded study. Ann Surg 236(4):458–464
Ström P, Hedman L, Särnå L, Kjellin A, Wredmark T, Felländer-Tsai L (2006) Early exposure to haptic feedback enhances performance in surgical simulator training: a prospective randomized crossover study in surgical residents. Surg Endosc 20(9):1383–1388
Sutherland LM, Middleton PF, Anthony A, Hamdorf J, Cregan P, Scott D, Maddern GJ (2006) Surgical simulation: a systematic review. Ann Surg 243(3):291–300
Aggarwal R, Grantcharov T, Eriksen J, Blirup D, Kristiansen V, Funch-Jensen P, Darzi A (2006) An evidence-based virtual reality training program for novice laparoscopic surgeons. Ann Surg 244(2):310–314
Zhang A, Hünerbein M, Dai Y, Schlag P, Beller S (2008) Construct validity testing of a laparoscopic surgery simulator (Lap Mentor): evaluation of surgical skill with a virtual laparoscopic training simulator. Surg Endosc 22(6):1440–1444
Epona Medical | LAP-X. http://www.lapx.eu/en/lapx.html. Accessed 26 June 2013
Iwata N, Fujiwara M, Kodera Y, Tanaka C, Ohashi N, Nakayama G, Koike M, Nakao A (2011) Construct validity of the LapVR virtual-reality surgical simulator. Surg Endosc 25(2):423–428
Sankaranarayanan G, Lin H, Arikatla V, Mulcare M, Zhang L, Derevianko A, Lim R, Fobert D, Cao C, Schwaitzberg S, Jones D, De S (2010) Preliminary face and construct validation study of a virtual basic laparoscopic skill trainer. J Laparoendosc Adv Surg Tech A 20(2):153–157
Zhang L, Grosdemouge C, Sankaranarayanan G, Anh W, Sreekanth A, De S, Jones D, Schwaitzberg S, Cao C (2012) The added value of virtual reality technology and force feedback for surgical training simulators. In: Proceedings of the IEA 2012 Meeting, Recife, Brazil
Arikatla V, Sankaranarayanan G, Ahn W, Chellali A, De S, Cao C, Hwabejire J, DeMoya M, Schwaitzberg S, Jones D (2013) Face and construct validation of a virtual peg transfer simulator. Surg Endosc 27(5):1721–1729
Zhang L, Sankaranarayanan G, Arikatla VS, Ahn W, Grosdemouge C, Rideout JM, Epstein SK, De S, Schwaitzberg SD, Jones DB, Cao C (2013) Characterizing the learning curve of the VBLaST-PT© (virtual basic laparoscopic skill trainer). Surg Endosc 27(10):3603–3615
Faul F, Erdfelder E, Lang A-G, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Acknowledgments
This project was supported by the National Institutes of Health (NIH) Grant NIBIB R01 EB010037-01. This work was supported by NIBIB/NIH Grant # R01EB010037.
Disclosures
Dr. Steven D. Schwaitzberg is a consultant for Stryker and Olympus and member of the advisory board for NeatStitch, AcuityBio, MITI, Cambridge Endo and Surgiquest. Dr. Daniel B. Jones is a consultant for Allurion. Likun Zhang, Venkata S. Arikatla, and Drs. Amine Chellali, Ganesh Sankaranarayanan, Woojin Ahn, Alexandre Derevianko, Marc DeMoya, and Caroline G.L. Cao have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chellali, A., Zhang, L., Sankaranarayanan, G. et al. Validation of the VBLaST peg transfer task: a first step toward an alternate training standard. Surg Endosc 28, 2856–2862 (2014). https://doi.org/10.1007/s00464-014-3538-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3538-2