Abstract
Background
The volume–outcome relationship has been validated previously for surgical procedures and cancer treatments. However, no studies have longitudinally compared the relationships between volume and outcome, and none have systematically compared laparoscopic cholecystectomy (LC) surgery outcomes in Taiwan. This study purposed to explore the relationship between volume and hospital treatment cost after LC.
Methods
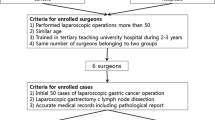
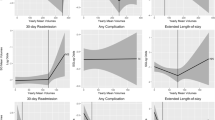
This cohort study retrospectively analyzed 247,751 LCs performed from 1998 to 2009. Hospitals were classified as low-, medium-, and high-volume hospitals if their annual number of LCs were 1–29, 30–84, ≥85, respectively. Surgeons were classified as low-, medium-, and high-volume surgeons if their annual number of LCs were 1–10, 11–24, ≥25, respectively. Hierarchical linear regression model and propensity score were used to assess the relationship between volume and hospital treatment cost.
Results
The mean hospital treatment cost was US $2,504.53, and the average hospital costs for high-volume hospitals/surgeons were 33/47 % lower than those for low-volume hospitals and surgeons. When analyzed by propensity score, the hospital treatment cost differed significantly between high-volume hospitals/surgeons and low/medium-volume hospitals/surgeons (2,073.70 vs. 2,350.91/2,056.73 vs. 2,553.76, P < 0.001).
Conclusions
Analysis using a hierarchical linear regression model and propensity score found an association between high-volume hospitals and surgeons and hospital treatment cost in LC patients. Moreover, the significant factors associated with hospital resource utilization for this procedure include age, gender, comorbidity, hospital type, hospital volume, and surgeon volume. Additionally, analysis of the treatment strategies adopted at high-volume hospitals or by high-volume surgeons may improve overall hospital treatment cost.
Similar content being viewed by others
References
Singla A, Simons JP, Carroll JE, Li Y, Ng SC, Tseng JF, Shah SA (2010) Hospital volume as a surrogate for laparoscopically assisted colectomy. Surg Endosc 24:662–669
Saad S, Paul A, Treckmann J, Tarabichi A, Nagelschmidt M, Arns W (2010) Laparoscopic live donor nephrectomy: are ten cases per year enough to reach the quality standards? A report from a single small-volume transplant center. Surg Endosc 24:594–600
Lehmann KS, Ritz JP, Wibmer A, Gellert K, Zornig C, Burghardt J, Büsing M, Runkel N, Kohlhaw K, Albrecht R, Kirchner TG, Arlt G, Mall JW, Butters M, Bulian DR, Bretschneider J, Holmer C, Buhr HJ (2010) The German registry for natural orifice translumenal endoscopic surgery: report of the first 551 patients. Ann Surg 252:263–270
Shi HY, Lee HH, Tsai MH, Chiu CC, Uen YH, Lee KT (2011) Long-term outcomes of laparoscopic cholecystectomy: a prospective piecewise linear regression analysis. Surg Endosc 25:2132–2140
Mercado MÁ, Franssen B, Dominguez I, Arriola-Cabrera JC, Ramírez-Del Val F, Elnecavé-Olaiz A, Arámburo-García R, García A (2011) Transition from a low- to a high-volume centre for bile duct repair: changes in technique and improved outcome. HPB (Oxford) 13:767–773
Csikesz NG, Singla A, Murphy MM, Tseng JF, Shah SA (2010) Surgeon volume metrics in laparoscopic cholecystectomy. Dig Dis Sci 55:2398–2405
Livingston EH, Cao J (2010) Procedure volume as a predictor of surgical outcomes. JAMA 304:95–97
D’Hoore W, Sicotte C, Tilquin C (1993) Risk adjustment in outcome assessment: the Charlson comorbidity index. Methods Inf Med 32:382–387
Marí-Dell’Olmo M, Martínez-Beneito MA, Borrell C, Zurriaga O, Nolasco A, Domínguez-Berjón MF (2011) Bayesian factor analysis to calculate a deprivation index and its uncertainty. Epidemiology 22:356–364
Hobbs BP, Carlin BP, Mandrekar SJ, Sargent DJ (2011) Hierarchical commensurate and power prior models for adaptive incorporation of historical information in clinical trials. Biometrics 67:1047–1056
Joffe MM, Rosenbaum PR (1999) Invited commentary: propensity scores. Am J Epidemiol 150:327–333
Rubin DB (1997) Estimating causal effects from large data sets using propensity scores. Ann Intern Med 127:757–763
Okrainec A, Ferri LE, Feldman LS, Fried GM (2011) Defining the learning curve in laparoscopic paraesophageal hernia repair: a CUSUM analysis. Surg Endosc 25:1083–1087
Kiran RP, Kirat HT, Ozturk E, Geisler DP, Remzi FH (2010) Does the learning curve during laparoscopic colectomy adversely affect costs? Surg Endosc 24:2718–2722
Bergamini C, Martellucci J, Tozzi F, Valeri A (2011) Complications in laparoscopic adrenalectomy: the value of experience. Surg Endosc 25:3845–3851
Harboe KM, Bardram L (2011) The quality of cholecystectomy in Denmark: outcome and risk factors for 20,307 patients from the national database. Surg Endosc 25:1630–1641
Panageas KS, Schrag D, Riedel E, Bach PB, Begg CB (2003) The effect of clustering of outcomes on the association of procedure volume and surgical outcomes. Ann Intern Med 139:658–665
Tiwari MM, Reynoso JF, High R, Tsang AW, Oleynikov D (2011) Safety, efficacy, and cost-effectiveness of common laparoscopic procedures. Surg Endosc 25:1127–1135
Jacobson KM, Hall Long K, McMurtry EK, Naessens JM, Rihal CS (2007) The economic burden of complications during percutaneous coronary intervention. Qual Saf Health Care 16:154–159
Lai CL, Fan CM, Liao PC, Tsai KC, Yang CY, Chu SH, Chien KL (2009) Impact of an audit program and other factors on door-to-balloon times in acute ST-elevation myocardial infarction patients destined for primary coronary intervention. Acad Emerg Med 16:333–342
Wang MJ, Lin SP (2010) Study on doctor shopping behavior: insight from patients with upper respiratory tract infection in Taiwan. Health Policy 94:61–67
Cheng SH, Song HY (2004) Physician performance information and consumer choice: a survey of subjects with the freedom to choose between doctors. Qual Saf Health Care 13:98–101
Disclosures
Hon-Yi Shi, King-Teh Lee, Chong-Chi Chiu, and Hao-Hsien Lee have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shi, HY., Lee, KT., Chiu, CC. et al. The volume–outcome relationship in laparoscopic cholecystectomy: a population-based study using propensity score matching. Surg Endosc 27, 3139–3145 (2013). https://doi.org/10.1007/s00464-013-2867-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2867-x