Abstract
Background
To improve patient safety, training of psychomotor laparoscopic skills is often done on virtual reality (VR) simulators outside the operating room. Haptic sensations have been found to influence psychomotor performance in laparoscopy. The emulation of haptic feedback is thus an important aspect of VR simulation. Some VR simulators try to simulate these sensations with handles equipped with haptic feedback. We conducted a survey on how laparoscopic surgeons perceive handles with and without haptic feedback.
Methods
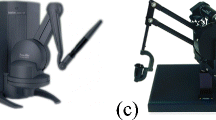
Surgeons with different levels of experience in laparoscopy were asked to test two handles: Xitact IHP with haptic feedback and Xitact ITP without haptic feedback (Mentice AB, Gothenburg, Sweden), connected to the LapSim (Surgical Science AB, Sweden) VR simulator. They performed two tasks on the simulator before answering 12 questions regarding the two handles. The surgeons were not informed about the differences in the handles.
Results
A total of 85 % of the 20 surgeons who participated in the survey claimed that it is important that handles with haptic feedback feel realistic. Ninety percent of the surgeons preferred the handles without haptic feedback. The friction in the handles with haptic feedback was perceived to be as in reality (5 %) or too high (95 %). Regarding the handles without haptic feedback, the friction was perceived as in reality (45 %), too low (50 %), or too high (5 %). A total of 85 % of the surgeons thought that the handle with haptic feedback attempts to simulate the resistance offered by tissue to deformation. Ten percent thought that the handle succeeds in doing so.
Conclusions
The surveyed surgeons believe that haptic feedback is an important feature on VR simulators; however, they preferred the handles without haptic feedback because they perceived the handles with haptic feedback to add additional friction, making them unrealistic and not mechanically transparent.







Similar content being viewed by others
References
van Hove PD, Tuijthof GJ, Verdaasdonk EG, Stassen LP, Dankelman J (2010) Objective assessment of technical surgical skills. Br J Surg 97:972–987
Reznick RK, MacRae H (2006) Teaching surgical skills—changes in the wind. N Engl J Med 355:2664–2669
Gallagher AG, Traynor O (2008) Simulation in surgery: opportunity or threat? Ir J Med Sci 177:283–287
Aggarwal R, Mytton OT, Derbrew M, Hananel D, Heydenburg M, Issenberg B, MacAulay C, Mancini ME, Morimoto T, Soper N, Ziv A, Reznick R (2010) Training and simulation for patient safety. Qual Saf Health Care 19(suppl 2):i34–i43
Liu A, Tendick F, Cleary K, Kaufmann C (2003) A survey of surgical simulation: applications, technology, and education. Presence Teleop Virt 12:599–614
Seymour NE (2008) VR to OR: a review of the evidence that virtual reality simulation improves operating room performance. World J Surg 32:182–188
Schijven M, Jakimowicz J (2003) Virtual reality surgical laparoscopic simulators. Surg Endosc 17:1943–1950
Satava RM (2001) Surgical education and surgical simulation. World J Surg 25:1484–1489
Picod G, Jambon AC, Vinatier D, Dubois P (2005) What can the operator actually feel when performing a laparoscopy? Surg Endosc 19:95–100
Ottermo MV, Ovstedal M, Lango T, Stavdahl O, Yavuz Y, Johansen TA, Marvik R (2006) The role of tactile feedback in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 16:390–400
Westebring-van der Putten EP, Goossens RH, Jakimowicz JJ, Dankelman J (2008) Haptics in minimally invasive surgery—a review. Minim Invasive Ther Allied Technol 17:3–16
Lamata P, Gomez EJ, Sanchez-Margallo FM, Lamata F, Antolin M, Rodriguez S, Oltra A, Uson J (2006) Study of laparoscopic forces perception for defining simulation fidelity. Stud Health Technol Inform 119:288–292
van der Meijden OA, Schijven MP (2009) The value of haptic feedback in conventional and robot-assisted minimal invasive surgery and virtual reality training: a current review. Surg Endosc 23:1180–1190
Tholey G, Desai JP, Castellanos AE (2005) Force feedback plays a significant role in minimally invasive surgery: results and analysis. Ann Surg 241:102–109
Bholat OS, Haluck RS, Murray WB, Gorman PJ, Krummel TM (1999) Tactile feedback is present during minimally invasive surgery. J Am Coll Surg 189:349–355
Westebring-van der Putten EP, van den Dobbelsteen JJ, Goossens RH, Jakimowicz JJ, Dankelman J (2009) Effect of laparoscopic grasper force transmission ratio on grasp control. Surg Endosc 23:818–824
Chmarra MK, Dankelman J, van den Dobbelsteen JJ, Jansen FW (2008) Force feedback and basic laparoscopic skills. Surg Endosc 22:2140–2148
van den Dobbelsteen JJ, Schooleman A, Dankelman J (2007) Friction dynamics of trocars. Surg Endosc 21:1338–1343
Sjoerdsma W, Herder JL, Horward MJ, Jansen A, Bannenberg JJG, Grimbergen CA (1997) Force transmission of laparoscopic grasping instruments. Minim Invasive Ther 6:274–278
Basdogan C, De S, Kim J, Muniyandi M, Kim H, Srinivasan MA (2004) Haptics in minimally invasive surgical simulation and training. IEEE Comput Graph Appl 24:56–64
Lamata P, Gomez EJ, Bello F, Kneebone RL, Aggarwal R, Lamata F (2006) Conceptual framework for laparoscopic VR simulators. IEEE Comput Graph 26:69–79
El Saddik A (ed) (2012) Haptics rendering and applications. InTech, faridabad, p 246
Salkini MW, Doarn CR, Kiehl N, Broderick TJ, Donovan JF, Gaitonde K (2010) The role of haptic feedback in laparoscopic training using the LapMentor II. J Endourol 24:99–102
Panait L, Akkary E, Bell RL, Roberts KE, Dudrick SJ, Duffy AJ (2009) The role of haptic feedback in laparoscopic simulation training. J Surg Res 156:312–316
Thompson JR, Leonard AC, Doarn CR, Roesch MJ, Broderick TJ (2011) Limited value of haptics in virtual reality laparoscopic cholecystectomy training. Surg Endosc 25:1107–1114
Okamura AM (2009) Haptic feedback in robot-assisted minimally invasive surgery. Curr Opin Urol 19:102–107
Botden SM, Torab F, Buzink SN, Jakimowicz JJ (2008) The importance of haptic feedback in laparoscopic suturing training and the additive value of virtual reality simulation. Surg Endosc 22:1214–1222
Zhou M, Tse S, Derevianko A, Jones DB, Schwaitzberg SD, Cao CG (2012) Effect of haptic feedback in laparoscopic surgery skill acquisition. Surg Endosc 26:1128–1134
Strom P, Hedman L, Sarna L, Kjellin A, Wredmark T, Fellander-Tsai L (2006) Early exposure to haptic feedback enhances performance in surgical simulator training: a prospective randomized crossover study in surgical residents. Surg Endosc 20:1383–1388
Yiasemidou M, Glassman D, Vasas P, Badiani S, Patel B (2011) Faster simulated laparoscopic cholecystectomy. Open Access Surg 4:39–44
Buzink SN, Goossens RH, De Ridder H, Jakimowicz JJ (2010) Training of basic laparoscopy skills on SimSurgery SEP. Minim Invasive Ther Allied Technol 19:35–41
Vapenstad C, Hofstad EF, Bo LE, Chmarra MK, Kuhry E, Johnsen G, Marvik R, Lango T (2012) Limitations of haptic feedback devices on construct validity on the LapSim® virtual reality simulator. Surg Endosc. doi:10.1007/s00464-012-2621-9
Vapenstad C, Buzink SN (2012) Procedural virtual reality simulation in minimally invasive surgery. Surg Endosc. doi:10.1007/s00464-012-2503-1
Ro CY, Toumpoulis IK, Ashton RC Jr, Jebara T, Schulman C, Todd GJ, Derose JJ Jr, McGinty JJ (2005) The LapSim: a learning environment for both experts and novices. Stud Health Technol Inform 111:414–417
Botden SM, Buzink SN, Schijven MP, Jakimowicz JJ (2007) Augmented versus virtual reality laparoscopic simulation: what is the difference? A comparison of the ProMIS augmented reality laparoscopic simulator versus LapSim virtual reality laparoscopic simulator. World J Surg 31:764–772
Ahlberg G, Enochsson L, Gallagher AG, Hedman L, Hogman C, McClusky DA 3rd, Ramel S, Smith CD, Arvidsson D (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193:797–804
van Dongen KW, Tournoij E, van der Zee DC, Schijven MP, Broeders IA (2007) Construct validity of the LapSim: can the LapSim virtual reality simulator distinguish between novices and experts? Surg Endosc 21:1413–1417
Aggarwal R, Tully A, Grantcharov T, Larsen CR, Miskry T, Farthing A, Darzi A (2006) Virtual reality simulation training can improve technical skills during laparoscopic salpingectomy for ectopic pregnancy. BJOG 113:1382–1387
Aggarwal R, Grantcharov TP, Eriksen JR, Blirup D, Kristiansen VB, Funch-Jensen P, Darzi A (2006) An evidence-based virtual reality training program for novice laparoscopic surgeons. Ann Surg 244:310–314
Larsen CR, Grantcharov T, Aggarwal R, Tully A, Sorensen JL, Dalsgaard T, Ottesen B (2006) Objective assessment of gynecologic laparoscopic skills using the LapSimGyn virtual reality simulator. Surg Endosc 20:1460–1466
Hassan I, Maschuw K, Rothmund M, Koller M, Gerdes B (2006) Novices in surgery are the target group of a virtual reality training laboratory. Eur Surg Res 38:109–113
Woodrum DT, Andreatta PB, Yellamanchilli RK, Feryus L, Gauger PG, Minter RM (2006) Construct validity of the LapSim laparoscopic surgical simulator. Am J Surg 191:28–32
Eriksen JR, Grantcharov T (2005) Objective assessment of laparoscopic skills using a virtual reality stimulator. Surg Endosc 19:1216–1219
Langelotz C, Kilian M, Paul C, Schwenk W (2005) LapSim virtual reality laparoscopic simulator reflects clinical experience in German surgeons. Langenbecks Arch Surg 390:534–537
Sherman V, Feldman LS, Stanbridge D, Kazmi R, Fried GM (2005) Assessing the learning curve for the acquisition of laparoscopic skills on a virtual reality simulator. Surg Endosc 19:678–682
Duffy AJ, Hogle NJ, McCarthy H, Lew JI, Egan A, Christos P, Fowler DL (2005) Construct validity for the LAPSIM laparoscopic surgical simulator. Surg Endosc 19:401–405
van Dongen KW, Ahlberg G, Bonavina L, Carter FJ, Grantcharov TP, Hyltander A, Schijven MP, Stefani A, van der Zee DC, Broeders IA (2011) European consensus on a competency-based virtual reality training program for basic endoscopic surgical psychomotor skills. Surg Endosc 25(1):166–171
Hassan I, Sitter H, Schlosser K, Zielke A, Rothmund M, Gerdes B (2005) A virtual reality simulator for objective assessment of surgeons’ laparoscopic skill. Chirurg 76:151–156
Danila R, Gerdes B, Ulrike H, Dominguez Fernandez E, Hassan I (2009) Objective evaluation of minimally invasive surgical skills for transplantation. Surgeons using a virtual reality simulator. Chirurgia (Bucur) 104:181–185
Tanoue K, Uemura M, Kenmotsu H, Ieiri S, Konishi K, Ohuchida K, Onimaru M, Nagao Y, Kumashiro R, Tomikawa M, Hashizume M (2010) Skills assessment using a virtual reality simulator, LapSim, after training to develop fundamental skills for endoscopic surgery. Minim Invasive Ther Allied Technol 19:24–29
Salisbury K, Conti F, Barbagli F (2004) Haptic rendering: introductory concepts. IEEE Comput Graph Appl 24:24–32
Liu P, Zheng W, Chebbi B (2007) Surgical simulation with high-fidelity haptic feedback. Int J Robot Autom 22:59–68
Hofstad EF, Vapenstad C, Chmarra MK, Lango T, Kuhry E, Marvik R (2012) A study of pshycomotor skills in minimally invasive surgery: what differntiates expert and non-expert performance. Surg Endosc. doi:10.1007/s00464-012-2524-9
Munz Y, Kumar BD, Moorthy K, Bann S, Darzi A (2004) Laparoscopic virtual reality and box trainers: is one superior to the other? Surg Endosc 18:485–494
Tanoue K, Ieiri S, Konishi K, Yasunaga T, Okazaki K, Yamaguchi S, Yoshida D, Kakeji Y, Hashizume M (2008) Effectiveness of endoscopic surgery training for medical students using a virtual reality simulator versus a box trainer: a randomized controlled trial. Surg Endosc 22:985–990
Hiemstra E, Terveer EM, Chmarra MK, Dankelman J, Jansen FW (2011) Virtual reality in laparoscopic skills training: is haptic feedback replaceable? Minim Invasive Ther Allied Technol 20(3):179–184
Avgerinos DV, Goodell KH, Waxberg S, Cao CG, Schwaitzberg SD (2005) Comparison of the sensitivity of physical and virtual laparoscopic surgical training simulators to the user’s level of experience. Surg Endosc 19:1211–1215
Youngblood PL, Srivastava S, Curet M, Heinrichs WL, Dev P, Wren SM (2005) Comparison of training on two laparoscopic simulators and assessment of skills transfer to surgical performance. J Am Coll Surg 200:546–551
Acknowledgments
We thank all those who participated in the study. The work has been supported by the National Centre for Advanced Laparoscopic Surgery, SINTEF, the National Competence Services for Ultrasound and Image guided Therapy, the Norwegian University of Science and Technology (NTNU), Trondheim, Norway; and the Marie Curie ITN EU project “Integrated Interventional Imaging Operating System” (project 238802).
Disclosures
C. Våpenstad, E. F. Hofstad, T. Langø, R. Mårvik, and M. K. Chmarra have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Våpenstad, C., Hofstad, E.F., Langø, T. et al. Perceiving haptic feedback in virtual reality simulators. Surg Endosc 27, 2391–2397 (2013). https://doi.org/10.1007/s00464-012-2745-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2745-y