Abstract
Background
Laparoscopic distal pancreatic surgery has gained popularity in the last decade. However, well-designed studies comparing laparoscopic distal pancreatectomy (LDP) to open distal pancreatectomy (ODP) are limited. We present a single-institution case-control study comparing outcomes of LDP to ODP.
Methods
From a prospectively accruing database, 104 patients who underwent distal pancreatectomy for pancreatic pathologies were eligible. Of these, 30 LDPs were matched with 30 ODPs using a 1:1 case-match design. Matching criteria were final histopathologic diagnosis and lesion size. Twelve LDPs were excluded from analysis because of lack of adequate ODP controls. In all cases, an attempt was made at conservation of the spleen.
Results
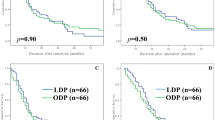
There were more females in the LDP group (p = 0.001). Other clinicopathologic characteristics of the LDP and ODP groups such mean age (52.4 ± 17.2 vs. 59 ± 12.8, p = 0.104), prior history of upper abdominal surgery (6.7% vs. 20.0%, p = 0.254) or pancreatitis (13.3% vs. 10.0%, p = 1.000), histopathologic diagnosis (p = 1.000), lesion size on imaging (3.7 ± 2.7 vs. 4.4 ± 2.4 cm, p = 0.170), and histopathology (3.8 ± 2.3 vs. 4.3 ± 2.3, p = 0.386) were comparable. There were no significant differences in postoperative complication rates (50.0% vs. 43.3%, p = 0.604), major complication rates (20% vs. 20%, p = 0.829), grade B/C pancreatic fistula rates (16.7% vs. 13.3%, p = 0.717), or reoperation rates (3.3% vs. 6.7%, p = 1.000) between LDP and ODP groups, respectively. There was a significantly higher rate of splenic conservation in the LDP group (70% vs. 30%, p = 0.002). The intraoperative blood loss (294 ± 245 vs. 726 ± 709 ml, p < 0.001) and mean duration of hospitalization (8.7 ± 4.2 vs. 12.6 ± 8.7 days, p = 0.009) were significantly lower in the LDP group compared to the ODP group.
Conclusion
LDP is a safe and feasible option for distal pancreatic resections in experienced centers. The postoperative complication rate is comparable to that of ODP. LDP is associated with lower operative blood loss, higher rate of splenic conservation, and shorter duration of hospitalization. These encouraging results demand further validation in prospective randomized trials.
Similar content being viewed by others
References
Vijan SS, Ahmed KA, Harmsen WS, Que FG, Reid-Lombardo KM, Nagorney DM, Donohue JH, Farnell MB, Kendrick ML (2010) Laparoscopic vs open distal pancreatectomy: a single-institution comparative study. Arch Surg 145(7):616–621
Kooby DA, Hawkins WG, Schmidt CM, Weber SM, Bentrem DJ, Gillespie TW, Sellers JB, Merchant NB, Scoggins CR, Martin RC 3rd, Kim HJ, Ahmad S, Cho CS, Parikh AA, Chu CK, Hamilton NA, Doyle CJ, Pinchot S, Hayman A, McClaine R, Nakeeb A, Staley CA, McMasters KM, Lillemoe KD (2010) A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg 210(5):779–787
Baker MS, Bentrem DJ, Ujiki MB, Stocker S, Talamonti MS (2009) A prospective single institution comparison of peri-operative outcomes for laparoscopic and open distal pancreatectomy. Surgery 146(4):635–643 discussion 643–645
Nakamura Y, Uchida E, Aimoto T, Matsumoto S, Yoshida H, Tajiri T (2009) Clinical outcome of laparoscopic distal pancreatectomy. J Hepatobiliary Pancreat Surg 16(1):35–41
Abu Hilal M, Jain G, Kasasbeh F, Zuccaro M, Elberm H (2009) Laparoscopic distal pancreatectomy: critical analysis of preliminary experience from a tertiary referral centre. Surg Endosc 23:2743–2747
Taylor C, O’Rourke N, Nathanson L, Martin I, Hopkins G, Layani L, Ghusn M, Fielding G (2008) Laparoscopic distal pancreatectomy: the Brisbane experience of forty-six cases. HPB (Oxford) 10(1):38–42
Kim SC, Park KT, Hwang JW, Shin HC, Lee SS, Seo DW, Lee SK, Kim MH, Han DJ (2008) Comparative analysis of clinical outcomes for laparoscopic distal pancreatic resection and open distal pancreatic resection at a single institution. Surg Endosc 22(10):2261–2268
Fernandez-Cruz L, Blanco L, Cosa R, Rendon H (2008) Is laparoscopic resection adequate in patients with neuroendocrine pancreatic tumors? World J Surg 32(5):904–917
Eom BW, Jang JY, Lee SE, Han HS, Yoon YS, Kim SW (2008) Clinical outcomes compared between laparoscopic and open distal pancreatectomy. Surg Endosc 22(5):1334–1338
Teh SH, Tseng D, Sheppard BC (2007) Laparoscopic and open distal pancreatic resection for benign pancreatic disease. J Gastrointest Surg 11(9):1120–1125
Pryor A, Means JR, Pappas TN (2007) Laparoscopic distal pancreatectomy with splenic preservation. Surg Endosc 21(12):2326–2330
Pierce RA, Spitler JA, Hawkins WG, Strasberg SM, Linehan DC, Halpin VJ, Eagon JC, Brunt LM, Frisella MM, Matthews BD (2007) Outcomes analysis of laparoscopic resection of pancreatic neoplasms. Surg Endosc 21(4):579–586
Palanivelu C, Shetty R, Jani K, Sendhilkumar K, Rajan PS, Maheshkumar GS (2007) Laparoscopic distal pancreatectomy: results of a prospective non-randomized study from a tertiary center. Surg Endosc 21(3):373–377
Melotti G, Butturini G, Piccoli M, Casetti L, Bassi C, Mullineris B, Lazzaretti MG, Pederzoli P (2007) Laparoscopic distal pancreatectomy: results on a consecutive series of 58 patients. Ann Surg 246(1):77–82
Fernandez-Cruz L, Cosa R, Blanco L, Levi S, Lopez-Boado MA, Navarro S (2007) Curative laparoscopic resection for pancreatic neoplasms: a critical analysis from a single institution. J Gastrointest Surg 11(12):1607–1621 discussion 1621–1622
Velanovich V (2006) Case-control comparison of laparoscopic versus open distal pancreatectomy. J Gastrointest Surg 10(1):95–98
Corcione F, Marzano E, Cuccurullo D, Caracino V, Pirozzi F, Settembre A (2006) Distal pancreas surgery: outcome for 19 cases managed with a laparoscopic approach. Surg Endosc 20(11):1729–1732
Mabrut JY, Fernandez-Cruz L, Azagra JS, Bassi C, Delvaux G, Weerts J, Fabre JM, Boulez J, Baulieux J, Peix JL, Gigot JF (2005) Laparoscopic pancreatic resection: results of a multicenter European study of 127 patients. Surgery 137(6):597–605
Dulucq JL, Wintringer P, Stabilini C, Feryn T, Perissat J, Mahajna A (2005) Are major laparoscopic pancreatic resections worthwhile? A prospective study of 32 patients in a single institution. Surg Endosc 19(8):1028–1034
Fabre JM, Dulucq JL, Vacher C, Lemoine MC, Wintringer P, Nocca D, Burgel JS, Domergue J (2002) Is laparoscopic left pancreatic resection justified? Surg Endosc 16(9):1358–1361
Kimura W, Inoue T, Futakawa N, Shinkai H, Han I, Muto T (1996) Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein. Surgery 120(5):885–890
Warshaw AL (1988) Conservation of the spleen with distal pancreatectomy. Arch Surg 123(5):550–553
Andy T, Colevas AD, Ann S, Valerie R, David J, Volker B, Corey L, Barbara M, Richard C, Coleman CN, Philip R (2003) CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 13(3):176–181
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Kanda M, Fujii T, Sahin TT, Kanzaki A, Nagai S, Yamada S, Sugimoto H, Nomoto S, Takeda S, Kodera Y, Morita S, Nakao A (2010) Invasion of the splenic artery is a crucial prognostic factor in carcinoma of the body and tail of the pancreas. Ann Surg 251(3):483–487
Yamaguchi K, Mizumoto K, Noshiro H, Sugitani A, Shimizu S, Chijiiwa K, Tanaka M (1999) Pancreatic carcinoma: ≤2 cm versus >2 cm in size. Int Surg 84(3):213–219
Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC (2002) The value of splenic preservation with distal pancreatectomy. Arch Surg 137(2):164–168
Goh BK, Tan YM, Chung YF, Cheow PC, Ong HS, Chan WH, Chow PK, Soo KC, Wong WK, Ooi LL (2008) Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg 143(10):956–965
Kleeff J, Diener MK, Z’Graggen K, Hinz U, Wagner M, Bachmann J, Zehetner J, Muller MW, Friess H, Buchler MW (2007) Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg 245(4):573–582
Lee SE, Jang JY, Lee KU, Kim SW (2008) Clinical comparison of distal pancreatectomy with or without splenectomy. J Korean Med Sci 23(6):1011–1014
Disclosure
Drs. Sanket Sharad Mehta, Ghalia Doumane, Thibault Mura, David Nocca, and Jean-Michel Fabre have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mehta, S.S., Doumane, G., Mura, T. et al. Laparoscopic versus open distal pancreatectomy: a single-institution case-control study. Surg Endosc 26, 402–407 (2012). https://doi.org/10.1007/s00464-011-1887-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1887-7