Abstract
Background
Premalignant duodenal lesions such as adenomas are rare. Surgical resection has been the standard approach to the treatment of these lesions. Endoscopic resection of superficial premalignant or malignant lesions of the gastrointestinal tract is used with increasing frequency. This study aimed to evaluate the safety and efficacy of endoscopic resection of duodenal neoplasms.
Methods
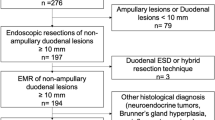
Patients with nonampullary duodenal adenomas or duodenal adenocarcinomas without familial polyposis syndrome between August 2002 and February 2009 were retrospectively analyzed. Data including location and size, technique used for the endoscopic resection, complications, and follow-up evaluation of the lesions were reviewed.
Results
The study enrolled 24 patients with duodenal neoplasms. Of these patients, 23 had duodenal adenomas and 1 had an adenocarcinoma confined to the mucosa. The mean age of the patients was 57 years (range, 40–82). In terms of location, 12 lesions (50%, 12/24) were found in the second portion of the duodenum, and 11 (45.8%, 11/24) were found in the first portion. Tubular adenomas were the most common type (17/24, 70.8%). There were four cases of the villotubular type and three of the villous type. Conventional endoscopic mucosal resection (EMR) was performed for 19 patients, EMR with ligation (EMR-L) for 3 patients, and snare polypectomy for 2 patients. Complete resection was achieved for 87.5% (21/24) of the patients, and the recurrence rate was 8.3% (2/24). All the complications were intraprocedural bleeding (n = 7), with no occurrence of perforation or infection. During a median follow-up period of 6 months (range, 3–36 months), recurrence of the duodenal neoplasm was observed in two cases. There was no procedure-related mortality.
Conclusions
Endoscopic resection of duodenal neoplasms was safe and effective treatment. During the short-term follow-up evaluation, EMR showed outcomes and complications comparable with prior procedures, including adenocarcinomas confined to the mucosa.
Similar content being viewed by others
Gastroduodenoscopy used for patients with gastrointestinal symptoms has identified a duodenal mass with increasing frequency. Duodenal adenomas, the most common manifestation of a duodenal neoplasm, are known to be precancerous lesions with a relatively high rate of malignant transformation [1, 2]. Most duodenal adenomas are resected surgically, although endoscopic mucosal resection (EMR) has comparable efficacy for the treatment of premalignant lesions as well as early malignant lesions of the esophagus, stomach, and colorectum [3, 4].
To date, the data on EMR for duodenal neoplasms are limited [5–7]. The safety and efficacy of EMR for the treatment of nonampullary duodenal neoplasms, predominantly duodenal adenomas, was evaluated for patients who had no familial polyposis syndrome.
Patients and methods
Study population
Between August 2002 and February 2009, 24 patients with a nonampullary duodenal neoplasm and no familial polyposis syndrome were included in the study and evaluated retrospectively. All the patients underwent diagnostic esophagoduodenoscopy whether they had gastrointestinal symptoms or not. In addition, data on the duodenal mass or polyp such as type and size were estimated, and a biopsy was performed using a conventional gastroscope or side-view duodenoscope (Olympus, Tokyo, Japan). Cases in which the lesion involved the ampulla or was confirmed histologically as an adenocarcinoma with submucosal invasion were excluded from the study.
Technical aspects of the EMR
After the adenoma or adenocarcinoma confined to the mucosa was confirmed by histology, EMR was performed. The EMR was carried out by experienced endoscopists (S.W.J., C.M.C.) who had managed more than 100 EMR cases over several years. With the patient under sedation using propofol and midazolam, conventional EMR and EMR with ligation (EMR-L) were performed using a snare-assisted technique and submucosal injection of normal saline solution with a single-use 21-gauge needle (Olympus). In two cases, a standard snare polypectomy without submucosal injection was performed. Two types of oval-shaped electrosurgical snares were used (diameters of 10 and 25 mm, Olympus).
The EMR technique was individualized by the endoscopist on a case-by-case basis. All duodenal lesions were trapped and resected as a whole lesion (en bloc method). Intraprocedural bleeding was defined as bleeding during the EMR. Hemostasis was provided using one or more of the following: treatment with a 1:10,000 epinephrine injection, clipping with hemoclips, or electrocoagulation with a coagulation probe (Fig. 1). The EMR was performed during a hospital admission or in the outpatient clinic.
Definition of terms and follow-up evaluation
A residual adenoma was defined as microscopically identified adenoma tissue with or without a remnant lesion identified macroscopically. A recurrent adenoma was defined as a microscopic adenoma at any time during the follow-up period after complete removal of the primary duodenal lesion. The duration of the follow up-period was defined as the number of months from the initial diagnostic endoscopy to the most recent endoscopy.
Results
Characteristics of the patients and the lesions
The mean age of the 17 men and 7 women included in the study was 57 years (range, 40–82 years). A total of 15 patients with comorbidities such as cardiopulmonary disease or diabetes were admitted to the hospital for the endoscopic resection (mean admission duration, 6.2 days; range, 3–9 days). The patients were followed up for a mean of 6 months (range, 3–36 months).
Outcome of the endoscopic resection
During the study period, 24 patients were included in the analysis. Duodenal adenoma was diagnosed for 23 patients and duodenal adenocarcinoma of the mucosa for 1 patient. For the patient with the mucosal adenocarcinoma, an abdominal computed tomography and positive emission tomography showed no evidence of metastatic or locally invasive disease.
In terms of tumor type, 17 tumors were tubular, 4 were villotubular, and 3 were villous. Of the 24 patients, 21 had mild dysplasia and 2 had high-grade dysplasia. All the patients had a single duodenal polyp except for one patient with three duodenal polyps. For 12 patients, the duodenal adenoma was located in the second portion of the duodenum, the most common site for its location. The lesion was located in the first portion of the duodenum for 11 patients and in the third portion for 1 patient. Although no objective measurements were obtained for the size of the polyp, it was estimated that 13 patients had polyps 1 to 2 cm in size, and 8 patients had a polyp was smaller than 1 cm (Table 1).
With regard to management, a conventional EMR was performed in 19 cases, an EMR-L in 3 cases, and a snare polypectomy in 2 cases. A complete resection was performed for 17 patients after the first conventional EMR. Two patients who underwent a conventional EMR had residual lesions defined by the presence of adenoma tissue in the resected margins (2/2 positive vertical and lateral margins). The one patient was confirmed to have adenocarcinoma at the follow-up endoscopy 1 month after the EMR and was referred for surgical management. The other patient showed a visible macroscopic lesion, diagnosed as a recurrent adenoma at follow-up endoscopy 1 month after the EMR and resected by conventional EMR. No macroscopic lesion was identified at the next follow-up endoscopy. Two of three patients who underwent an EMR-L were completely resected, and one had involvement of the lateral resected margin. None of these patients showed recurrence at follow-up endoscopy. Two patients had a snare polypectomy and showed no recurrence at follow-up endoscopy (Fig. 2).
Complications
Intraprocedural bleeding was noted in seven patients. Five of these patients underwent endoscopic hemostasis with hemoclips and electrocoagulation. Only electrocoagulation was needed for two patients with bleeding. Delayed bleeding was not detected, and other complications such as perforation or infection did not occur. There was no procedure-related death.
Discussion
Duodenal adenomas are precancerous lesions characterized by a high rate of malignant transformation. Despite considerable technical advances in endoscopic resection for superficial neoplasms of the gastrointestinal tract, few reports have described duodenal EMR. Due to the risk of perforation and difficulty with bleeding control, many investigators consider duodenal endoscopic treatment a high-risk procedure [5]. The duodenal adenoma causes nonspecific clinical manifestations such as epigastric pain (36%), jaundice (34%), weight loss (20%), anemia (12%), vomiting (5%), and diarrhea (2%). In many cases, the lesion is found incidentally [8]. However, these lesions occur more frequently with aging. The mean age at diagnosis is 60 to 72 years [9].
Although surgical resection has been considered the standard treatment for duodenal adenomas, a high rate of complications has been associated with the surgery due to the structures around the duodenum [10, 11]. For this reason, endoscopic resection of duodenal polyps may be a better approach and has been used more frequently in recent years.
The recurrence rate in the current series was 8.3% (2/24). Three cases had a villous adenoma, which is known to have a relatively high rate of recurrence [12]. Farnell et al. [13] reported that among 50 patients with benign tumors managed by transduodenal local excision, 17 had a recurrence. The recurrence rate was 32% at 5 years and 43% at 10 years. However, in the current study, none of the patients with a villous adenoma, including the mucosal adenocarcinoma, had a recurrence. However, the follow-up period was short. Two of the four villotubular adenomas recurred (patients 2 and 4 in Table 1). In the one case, the recurrence was managed with complete resection using the endoscopic procedure. However, in the other case, a snare polypectomy was performed at 6 months for a recurrent villous adenoma at the same site, and an adenocarcinoma with submucosal invasion was confirmed at the 12-month follow up evaluation. Although the follow-up period was short, the patients with nontubular adenomas seemed to show a tendency for a high recurrence rate.
The complete resection rate in this series was 87.5% (21/24) during the first 3 months of the follow-up period. The total length of the follow-up period varied widely. However, based on the short-term follow-up evaluation, the feasibility of endoscopic resection was comparable with that of more traditional procedures. Due to the en bloc resection of the neoplasm and no additional ablative thermal treatment such as argon plasma coagulation that could destroy adenomatous tissue, the histologic assessment of the resection margin and confirmation of a complete resection were reliable and accurate.
Two patients with residual lesions after the first endoscopic resection, excluding the patient with later development of an adenocarcinoma, had positive resection margins. Because they had no macroscopic lesion at follow-up assessment 1 to 3 months after the endoscopic resection, they received a diagnosis of “no recurrence.”
The complication rate in the current study was 26.2% (7/24). Ahmad et al. [6] reported a 33% frequency of bleeding during a duodenal EMR, and Lepilliez et al. [14] reported a 25% frequency of bleeding. In our series, all the patients with bleeding had intraprocedural bleeding. These findings are similar to those of previous reports. There was no case of massive bleeding requiring a transfusion. However, for patients with bleeding, additional hospitalization was required.
In conclusion, endoscopic resection had an outcome comparable with that of more traditional procedures and proved to be a safe and effective treatment for duodenal polyps. Therefore, EMR should be considered as an alternative to surgery, especially for patients that are not good candidates for surgery. Additional studies are needed to determine the long-term outcome for endoscopic resection of duodenal neoplasms.
References
Galandiuk S, Hermann RE, Jagelman DG, Fazio VW, Sivak MV (1988) Villous tumors of the duodenum. Ann Surg 207:234–239
Miller JH, Gisvold JJ, Weiland LH, Mcllrath DC (1980) Upper gastrointestinal tract: villous tumors. AJR Am J Roentgenol 134:933–936
Bories E, Pesenti C, Monges G, Lelong B, Moutardier V, Delpero JR, Giovannini M (2006) Endoscopic mucosal resection for advanced sessile adenoma and early-stage colorectal adenocarcinoma. Endoscopy 38:231–235
Jameel JK, Pillinger SH, Moncur P, Tsai HH, Duthie GS (2006) Endoscopic mucosal resection (EMR) in the management of large colorectal polyps. Colorectal Dis 8:497–500
Apel D, Jakobs R, Spiethoff A, Rieman JF (2005) Follow-up after endoscopic snare resection of duodenal adenomas. Endoscopy 37:444–448
Ahmad NA, Kochman ML, Long WB, Furth EE, Ginsberg GG (2002) Efficacy, safety, and clinical outcome of endoscopic mucosal resection: a study of 101 cases. Gastrointest Endosc 3:390–396
Bjork KJ, Davis CJ, Nagorney DM, Mucha P Jr (1990) Duodenal villous tumors. Arch Surg 125:961–965
Motton G, Veraldi GF, Fracastoro G, Ricci F, Laterza E, Dorrucci V, Cordiano C (1996) Vater’s papilla and periampullary area villous adenoma: personal experience about nine cases and review of the literature. Hepatogastroenterology 43:448–455
Chappius CW, Di Vincenti FC, Cohn I Jr (1989) Villous tumors of the duodenum. Ann Surg 209:593–599
Krukowski ZH, Ewen SW, Davidson AI, Matheson NA (1988) Operative management of tubulovillous neoplasms of the duodenum and ampulla. Br J Surg 75:150–153
Perez A, Saltzman JR, Carr-Locke DL, Brooks DC, Osteen RT, Zinner MJ, Ashley SW, Whang EE (2003) Benign nonampullary duodenal neoplasms. J Gastrointest Surg 7:536–541
Perzin KH, Bridge MF (1981) Adenomas of the small intestine: a clinicopathologic review of 51 cases and a study of their relationship to carcinoma. Cancer 48:799–819
Farnell MB, Sakorafas GH, Sarr MG, Rowland CM, Tsiotos GG, Farley DR, Nagorney DM (2000) Villous tumors of the duodenum: reappraisal of local vs. extended resection. J Gastrointest Surg 4:13–23
Lepilliez V, Chemaly M, Ponchon T, Napoleon B, Saurin JC (2008) Endoscopic resection of sporadic duodenal adenoma: an efficient technique with a substantial risk of delayed bleeding. Endoscopy 40:806–810
Disclosures
Jong Won Sohn, Seong Woo Jeon, Chang Min Cho, Min Kyu Jung, Sung Kook Kim, Dong Seok Lee, Hyuk Su Son, and In Kwon Chung have no conflicts of interest or financial ties to disclosure.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sohn, J.W., Jeon, S.W., Cho, C.M. et al. Endoscopic resection of duodenal neoplasms: a single-center study. Surg Endosc 24, 3195–3200 (2010). https://doi.org/10.1007/s00464-010-1114-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1114-y