Abstract
Background
Chromoendoscopy is traditionally used to identify inconspicuous Barrett’s neoplasia and mark the boundaries before endoscopic mucosal resection (EMR). Trimodal imaging endoscopy is useful in identifying early neoplasia in Barrett’s esophagus. The purpose of this study was to determine the efficacy (lateral and deep margin clearance) of trimodal imaging endoscopy-assisted EMR in early Barrett’s neoplasia in a tertiary referral setting.
Methods
The entire Barrett’s segment was visualized by high-resolution endoscopy followed by autofluorescence imaging, and suspicious areas were identified. Narrow band imaging and magnification was used to confirm the suspicious areas. The outer boundary of the lesion was then marked using the tip of a snare diathermy and EMR was performed using multiband mucosectomy technique by a single operator (KR).
Results
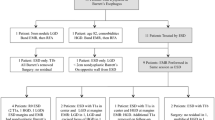
Sixteen patients were included: 13 patients had high-grade intraepithelial neoplasia (HGIN); 3 patients had intramucosal carcinoma (IMC); (8 males, median age, 69.5 (range, 50–77) years with Barrett’s esophagus (interquartile range (IQR), 2–5 cm; median length, 3 cm). All lesions were successfully identified, using trimodal imaging endoscopy. Overall EMR was complete in 14 of 16 (81.2%) patients with early Barrett’s neoplasia. Four of 16 patients (18%; all with pre-EMR HGIN) were considered to have incomplete EMR (deep margins involved), but operative histology showed only Barrett’s metaplasia in 2 (histological false positive) and IMC in 1. Thus, overall 14 of 16 (87.5%) patients had complete EMR of the original lesions. In patients who did not undergo esophagectomy, there was no disease recurrence on endoscopic biopsies at a mean follow-up of 8 (IQR, 6–12) months. Three of the 16 patients (18.75%) with post-EMR bleeding were successfully treated with APC/hemoclips.
Conclusions
Trimodal imaging endoscopy is a feasible alternative to chromoendoscopy to identify inconspicuous neoplasia and assist EMR of early neoplasia in Barrett’s esophagus.

Similar content being viewed by others
References
Kiesslich R, Hahn M, Herrmann G et al (2001) Screening for specialized columnar epithelium with methylene blue: chromoendoscopy in patient’s with Barrett’s esophagus and a normal control group. Gastrointest Endosc 53:47–52
Dave U, Shousha S, Westaby D (2001) Methylene blue staining: is it really useful in Barrett’s esophagus? Gastrointest Endosc 53:333–335
Curvers WL, Singh R, Song LM et al (2008) Endoscopic tri-modal imaging for detection of early neoplasia in Barrett’s oesophagus: a multi-centre feasibility study using high-resolution endoscopy, autofluorescence imaging and narrow band imaging incorporated in one endoscopy system. Gut 57:167–172
Anagnostopoulos G, Yao K, Kaye P et al (2007) Novel endoscopic observation in Barrett’s oesophagus using high resolution magnification endoscopy and narrow band imaging. Aliment Pharmacol Ther 26:501–507
Ell C, May A, Pech O et al (2007) Curative endoscopic resection of early esophageal adenocarcinomas (Barrett’s cancer). Gastrointest Endosc 65:3–10
Endoscopy Classification Review Group (2005) Update on the Paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy 37:570–578
Chaves DM, Sakai P, Mester M et al (1994) A new endoscopic technique for the resection of flat polypoid lesions. Gastrointest Endosc 40:224–226
May A, Gossner L, Behrens A et al (2003) A prospective randomized trial of two different endoscopic resection techniques for early stage cancer of the oesophagus. Gastrointest Endosc 58:167–175
Oliver JR, Wild CP, Sahay P et al (2003) Chromoendoscopy with methylene blue and associated DNA damage in Barrett’s oesophagus. Lancet 362:373–374
Nijhawan PK, Wang KK (2000) Endoscopic mucosal resection for lesions with endoscopic features suggestive of malignancy and high-grade dysplasia within Barrett’s esophagus. Gastrointest Endosc 52:328–332
Peters FP, Kara MA, Rosmolen WD et al (2006) Stepwise radical endoscopic resection is effective for complete removal of Barrett’s esophagus with early neoplasia: a prospective study. Am J Gastroenterol 101:1449–1457
Gondrie JJ, Pouw RE, Sondermeijer CM et al (2008) Effective treatment of early Barrett’s neoplasia with stepwise circumferential and focal ablation using the HALO system. Endoscopy 40:370–379
Stein HJ, von Rahden BH, Feith M (2005) Surgery for early stage oesophageal adenocarcinoma. J Surg Oncol 92:210–217
Acknowledgment
Dr. Singh received the Lancet International Fellowship 2006, to pursue an Advanced Endoscopy Fellowship at the Queens Medical Centre, Nottingham, UK.
Disclosure
Dr. Ragunath has received educational grants, speaker honorarium, and research support from Wilson-Cook Medical and Olympus-Keymed, UK.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomas, T., Singh, R. & Ragunath, K. Trimodal imaging-assisted endoscopic mucosal resection of early Barrett’s neoplasia. Surg Endosc 23, 1609–1613 (2009). https://doi.org/10.1007/s00464-009-0429-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0429-z