Abstract
Background
Patients with major comorbidities often are denied laparoscopic colorectal resections because they are thought to be at too “high risk.” Paradoxically, these patients generally have the most to gain from a minimally invasive surgical approach. This study aimed to examine the feasibility and safety of laparoscopic colorectal resection to determine whether it is contraindicated for “high-risk” patients.
Methods
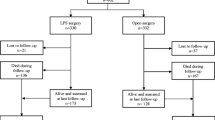
From August 1996 to February 2004, 368 consecutive patients (95 men) undergoing a laparoscopic colorectal procedure by a single surgeon were prospectively studied with regard to pre-, peri-, and postoperative events. High-risk patients (n = 190) were defined as elderly (age, >80 years; n = 28), morbidly obese (body mass index [BMI], >30 kg/m2; n = 55), American Society of Anesthesiology (ASA) 3 or 4 (n = 130), and recipients of preoperative radiotherapy (n = 54). Multiple risk factors were found for 67 patients, 7 of whom had three risk factors. The median age of the patients was 66 years (range, 19–92 years). The diagnoses included rectal cancer (n = 48), diverticulitis (n = 43), colon cancer (n = 34), benign polyp (n = 26), and other (n = 39). The following procedures were performed: colon resection (n = 114; left, 63; right, 41; total abdominal colectomy, 10), rectal resection (low anterior resection or pouch) (n = 49), coloanal anastomosis (n = 23), and other (n = 4). Data regarding intent to treat, operative events, morbidity, mortality, and outcomes were analyzed and form the basis of this report.
Results
No mortalities occurred. The major morbidity rate was 2%. There were no anastomotic leaks. The cases were laparoscopically performed (94%) or laparoscopically assisted, or were converted to open procedure (3%). The median estimated blood loss was 200 ml, and only 5% required perioperative transfusion. The perioperative course involved the following median periods: 2 days until flatus, 3 days until bowel movement, 1 day until clear liquid diet, 3 days until a regular diet, and 5 days until hospital discharge.
Conclusion
In experienced hands, laparoscopic colorectal resection can be performed safely for “high-risk” surgical patients. The better than expected outcomes in this patient population reinforce the benefits of minimally invasive surgery for this patient group and argues against using parameters of increased age, morbid obesity, high ASA class, or preoperative radiation alone as contraindications to even complex laparoscopic colorectal procedures.
Similar content being viewed by others
References
Payne JE, Chapuis PH, Pheils MT (1986) Surgery for large bowel cancer in people aged 75 years and older. Dis Colon Rectum 29:733–737
Fielding LP, Phillips RK, Hittinger R (1989) Factors influencing mortality after curative resection for large bowel cancer in elderly patients. Lancet 1:595–597
Isbister WH (1997) Colorectal surgery in the elderly: an audit of surgery in octogenarians. Aust N Z J Surg 67:557–561
Wise WE Jr, Padmanabhan A, Meesig DM, Arnold MW, Aguilar PS, Stewart WR (1991) Abdominal colon and rectal operations in the elderly. Dis Colon Rectum 34:959–963
Whittle J, Steinberg EP, Anderson GF, Herbert R (1992) Results of colectomy in elderly patients with colon cancer, based on Medicare claims data. Am J Surg 163:572–576
Spivak H, Maele DV, Friedman I, Nussbaum M (1996) Colorectal surgery in octogenarians. J Am Coll Surg 183:46–50
Bender JS, Maguson TH, Zenilman ME, Smith-Meek MM, Ratner LE, Jones CE, Smith GW (1996) Outcome following colon surgery in the octogenarian. Am Surg 62:276–279
Greenlund KJ, Zheng ZJ, Keenan NL, Giles WH, Casper ML, Mensah GA, Croft JB (2004) Trends in self-reported multiple cardiovascular disease risk factors among adults in the United States, 1991–1999. Arch Intern Med 164:181–188
Kushner RF (2002) Medical management of obesity. Semin Gastrointest Dis 13:123–132
Israelsson LA, Jonsson T (1997) Overweight and healing of midline incisions: the importance of suture technique. Eur J Surg 163:175–180
Pikarsky AJ, Saida Y, Yamagucki T, Martinez S, Chen W, Weiss EG, Nogueras JJ, Wexner SD (2002) Is obesity a high-risk factor for laparoscopic colorectal surgery? Surg Endosc 16:855–858
Riou JP, Cohen JR, Johnson H Jr (1992) Factors influencing wound dehiscence. Am J Surg 163:324–330
Roberts JV, Bates T (1992) The use of body mass index in studies of abdominal wound infection. J Hosp Infect 20:217–220
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M (1998) Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg 85:355–358
Stockholm Rectal Cancer Study Group (1990) Preoperative short-term radiation therapy in operable rectal carcinoma. Cancer 66:49–55
Goldberg P, Nicholls R, Porter N, Love S, Grimsey J (1994) Long-term results of a randomized trial of short-course low-dose adjuvant preoperative radiotherapy for rectal cancer: reduction in local treatment failure. Eur J Cancer 30A:1597–1599
Marijnen CAM, Kapiteijn E, Van de Velde CJH, Martijn H, Steup WH, Wiggers T, Klein Kranenbarg E, Leer JWH (2002) Acute side effects and complications after short-term preoperative radiotherapy combined with total mesorectal excision in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 20:817–825
Falk PM, Beart RW Jr, Wexner SD, Thorson AG, Jagelman DG, Lavery IC, Johansen OB, Firzgibbons RJ Jr (1993) Laparoscopic colectomy: a critical appraisal. Dis Colon Rectum 36:28–34
Peters WR, Bartels TL (1993) Minimally invasive colectomy: are the potential benefits realized? Dis Colon Rectum 36:751–756
Lacy AM, Garcia-Valdecasas JC, Pique JM, Delgado S, Campo E, Bords JM, Taura P, Grande L, Fuster J, Pacheco JL (1995) Short-term outcome analysis of a randomized study comparing laparoscopic vs. open colectomy for colon cancer. Surg Endosc 9:1101–1105
Lord SA, Larach SW, Ferrara A, Williamson PR, Lago CP, Lube MW (1996) Laparoscopic resections for colorectal carcinoma: a three-year experience. Dis Colon Rectum 39:148–154
Franklin ME Jr, Rosenthal D, Abrego-Medina D, Dorman P, Glass JL, Norem R, Diaz A (1996) Prospective comparison of open vs. laparoscopic colon surgery for carcinoma: five-year results. Dis Colon Rectum 39(Suppl):S35–S46
Khalili TM, Fleshner PR, Hiatt JR, Sokol TP, Manookian C, Tsushima C, Phillips EH (1998) Colorectal cancer: comparison of laparoscopic with open approaches. Dis Colon Rectum 41:832–838
Schwenk W, Bohm B, Muller JM (1998) Postoperative pain and fatigue after laparoscopic or conventional colorectal resections: a prospective randomized trial. Surg Endosc 12:1131–1136
Schwenk W, Bohm B, Haase O, Junghans T, Muller JM (1998) Laparoscopic versus conventional colorectal resection: a prospective randomised study of postoperative ileus and early postoperative feeding. Langenbecks Arch Surg 383:49–55
Schwenk W, Bohm B, Witt C (1999) Pulmonary function following laparoscopic or conventional colorectal resection: a randomized controlled evaluation. Arch Surg 134:6–12
Chen HH, Wexner SD, Iroatulam AJ, Pikarsky AJ, Alabaz O, Nogueras JJ, Nessim A, Weiss EG (2000) Laparoscopic colectomy compares favorably with colectomy by laparotomy for reduction of postoperative ileus. Dis colon Rectum 43:61–65
Agachan F, Joo JS, Sher M, Weiss EG, Nogueras JJ, Wexner SD (1997) Laparoscopic colorectal surgery. Do we get faster? Surg Endosc 11:331–335
Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW Jr (1997) The learning curve for laparoscopic colorectal surgery: preliminary results from a prospective analysis of 1,194 laparoscopic-assisted colectomies. Arch Surg 132:41–44
Marusch F, Gastinger I, Schneider C, Scheidbach H, Konradt J, Bruch HP, Kohler L, Barlehner E, Kockerling F; Laparoscopic Colorectal Surgery Study Group (LCSSG) (2001) Experience as a factor influencing the indications for laparoscopic colorectal surgery and results. Surg Endosc 15:116–120
Schlacta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC (2001) Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum 44:217–222
Seshadri PA, Mamazza J, Schlachta CM, Cadeddu MO, Poulin EC (2001) Laparoscopic colorectal resection in octogenarians. Surg Endosc 15:802–805
Stewart BT, Stitz RW, Lumley JW (1999) Laparoscopically assisted colorectal surgery in the elderly. Br J Surg 86:938–941
Schwandner O, Schiedeck TH, Bruch H (1999) The role of conversion in laparoscopic colorectal surgery: do predictive factors exist? Surg Endosc 13:151–156
Dean PA, Beart RW Jr, Nelson H, Elftmann TD, Schlinkert RT (1994) Laparoscopic-assisted segmental colectomy: early Mayo Clinic experience. Mayo Clin Proc 69:834–840
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marks, J.H., Kawun, U.B., Hamdan, W. et al. Redefining contraindications to laparoscopic colorectal resection for high-risk patients. Surg Endosc 22, 1899–1904 (2008). https://doi.org/10.1007/s00464-008-9828-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-9828-9