Abstract
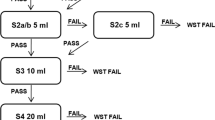
Aspiration is a common phenomenon in patients with oropharyngeal dysphagia. It can be studied using fiberoptic endoscopic evaluation of swallowing (FEES). FEES is well known and widely used in the diagnosis and treatment of swallowing disorders. However, various protocols exist, and there is no consensus on the examination protocol. The objective of this prospective study was to determine the FEES protocol derived estimates of sensitivity (Se′) to detection of aspiration in dysphagic patients. The study estimated the probability of aspiration as a function of the number of swallow trials in dysphagic patients using FEES. The derived sensitivity was calculated based on presence or absence of aspiration in a ten-swallow trial protocol as arbitrary ‘gold standard’. Eighty-four persons were included, comprising two patient populations with oropharyngeal dysphagia. Dysphagia in one group was due to head and neck cancer and possible oncological treatment effects on swallowing; in the other it was a result of neurological disease. All patients underwent a standardized FEES examination using ten swallows of thin liquid followed by ten swallows of thick liquid, all in boluses of 10 cc each. FEES recordings were rated for aspiration by an expert panel blinded to patients’ identity and clinical history. Descriptive statistics, Kaplan–Meier survival analysis techniques, and Log Rank/Mantel–Cox tests were used. In both patient populations the aspiration risk was underestimated when using a limited number (three or four) of swallow trials. The oncology and neurology patients differed significantly in the number of swallow trials required to determine aspiration for thin liquids (median values 2 and 7 respectively, P = 0.006). FEES protocols using a limited number of swallow trials can underestimate the aspiration risk in both oncological and neurological patients suffering from oropharyngeal dysphagia, especially when using boluses with a thin liquid consistency.




Similar content being viewed by others
References
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63.
Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003;124:328–36.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Kelly AM, Drinnan MJ, Leslie P. Assessing penetration and aspiration: how do videofluoroscopy and fiberoptic endoscopic evaluation of swallowing compare? Laryngoscope. 2007;117:1723–7.
Langmore SE, Aviv JE. Endoscopic evaluation and treatment of swallowing disorders. New York: Thieme; 2001.
Langmore SE. Evaluation of oropharyngeal dysphagia: which diagnostic tool is superior? Curr Opin Otolaryngol Head Neck Surg. 2003;11:485–9.
Dziewas R, Warnecke T, Ölenberg S, Teismann I, Zimmermann J, Krämer C, Ritter M, Ringelstein EB, Schäbitz WR. Towards a basic endoscopic assessment of swallowing in acute stroke – development and evaluation of a simple dysphagia score. Cerebrovasc Dis. 2008;26:41–7.
Leder SB, Espinosa JF. Aspiration risk after acute stroke: comparison of clinical examination and fiberoptic endoscopic evaluation of swallowing. Dysphagia. 2002;17:214–8.
Warnecke T, Teismann I, Meimann W, Ölenberg S, Zimmermann J, Krämer C, Ringelstein EB, Schäbitz WR, Dziewas R. Assessment of aspiration risk in acute ischaemic stroke—evaluation of the simple swallowing provocation test. J Neurol Neurosurg Psychiatry. 2008;79:312–4.
Baijens LW, Speyer R, Passos VL, Pilz W, van der Kruis J, Haarmans S, Desjardins-Rombouts C. Surface electrical stimulation in dysphagic parkinson patients: a randomized clinical trial. Laryngoscope. 2013. doi:10.1002/lary.24119.
Bours GJ, Speyer R, Lemmens J, Limburg M, de Wit R. Bedside screening tests vs. videofluoroscopy or fibreoptic endoscopic evaluation of swallowing to detect dysphagia in patients with neurological disorders: systematic review. J Adv Nurs. 2009;65:477–93.
Baijens LWJ. Multidisciplinaire polikliniek voor dysfagie. Nederlands Tijdschrift voor Keel-Neus-Oorheelkunde 18e jaargang nummer 1 januari 2012 p5-6.
Folstein MF, Folstein SE, McHugh PR. “Mini–mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Crary MA. Carnaby Mann GD, Groher ME. Initial psychometric assessment of a Functional Oral Intake Scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20.
Speyer R, Baijens L, Heijnen M, Zwijnenberg I. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia. 2010;25:40–65.
Last JM. A dictionary of epidemiology. Oxford: Oxford University Press; 2001.
Jager KJ, van Dijk PC, Zoccali C, Dekker FW. The analysis of survival data: the Kaplan–Meier method. Kidney Int. 2008;74:560–5.
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baijens, L.W.J., Speyer, R., Pilz, W. et al. FEES Protocol Derived Estimates of Sensitivity: Aspiration in Dysphagic Patients. Dysphagia 29, 583–590 (2014). https://doi.org/10.1007/s00455-014-9549-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-014-9549-2