Abstract
Background
Early medical palliative care has been shown to improve overall survival of patients with metastatic cancer, but the role of cardiac surgical interventions in such patients is not clear. The limited life expectancy of these patients often poses a dilemma to clinicians and involves a detailed analysis of the risks and benefits of such interventions. This study examines the outcomes of percutaneous coronary intervention (PCI) in patients with metastatic cancer.
Methods
The National Inpatient Database of USA was used to identify patients aged ≥18 years who had a diagnosis of metastatic cancer and acute coronary syndrome (ACS) between 2000 and 2009 using ICD-9-CM codes. These were categorized into ST elevation myocardial infarction (STEMI) and non-ST elevation myocardial infarction (NSTEMI). The utilization of PCI was also identified using ICD-9-CM codes. The outcomes studied were in-hospital mortality, length of hospital stay and discharge disposition. The association between various outcomes and use of cardiac catheterization was assessed using multivariate regression models.
Results
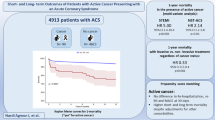
There were 49,515 patients with metastatic disease who were discharged with a diagnosis of ACS. Of these, 15,964 had STEMI and 33,551 had NSTEMI. 3981 patients (24.9 %) with STEMI and 3209 patients (9.6 %) with NSTEMI received percutaneous coronary intervention. Caucasian male patients under age 65 years were more likely to receive PCI in the setting of an ACS. The hospital characteristics associated with higher use of PCI included academic affiliation, large bedsize, private for-profit hospitals and Midwestern and Western regions of USA. The adjusted odds of receiving PCI in this group of patient have gradually increased by 1.14 every year in last decade (95 % CI 1.11–1.16). The beneficial effect of PCI on in-hospital mortality has declined in NSTEMI such that by 2009, there was no significant difference between patients who received PCI and those who did not receive PCI. This has remained unchanged for STEMI patients.
Conclusions
In metastatic cancer patients with ACS, the rate of PCI has increased over the last decade. In the current era, metastatic cancer patients with NSTEMI may perform equally well without PCI in terms of in-hospital mortality. The decision to provide such care may be considered on an individual basis based on the extent of their medical comorbidity and tumor burden.


Similar content being viewed by others
References
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr et al (2014) 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130(25):2354–2394. doi:10.1161/CIR.0000000000000133
Cook MB, McGlynn KA, Devesa SS, Freedman ND, Anderson WF (2011) Sex disparities in cancer mortality and survival. Cancer Epidemiol Biomarkers Prev. 20(8):1629–1637. doi:10.1158/1055-9965.EPI-11-0246
Fryar CD, Chen TC, Li X (2012) Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999-2010. NCHS data brief 103:1–8
Gaglia MA Jr, Torguson R, Xue Z, Gonzalez MA, Ben-Dor I, Maluenda G et al (2011) Effect of insurance type on adverse cardiac events after percutaneous coronary intervention. Am J Cardiol 107(5):675–680. doi:10.1016/j.amjcard.2010.10.041
Ganti AK, Siedlik E, Marr AS, Loberiza FR Jr, Kessinger A (2011) Predictive ability of Charlson comorbidity index on outcomes from lung cancer. Am J Clin Oncol 34(6):593–596. doi:10.1097/COC.0b013e3181fe445b
Group USCSW (2014) United States Cancer Statistics: 1999–2011 Incidence and Mortality Web-based Report. US Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. 2014–2015
Khakoo AY, Yeh ET (2008) Therapy insight: management of cardiovascular disease in patients with cancer and cardiac complications of cancer therapy. Nat Clin Pract Oncol 5(11):655–667. doi:10.1038/ncponc1225
Labianca R, Beretta G, Clerici M, Fraschini P, Luporini G (1982) Cardiac toxicity of 5-fluorouracil: a study on 1083 patients. Tumori. 68(6):505–510
Lejonc JL, Vernant JP, Macquin J, Castaigne A (1980) Myocardial infarction following vinblastine treatment. Lancet 2(8196):692
Mandel EM, Lewinski U, Djaldetti M (1975) Vincristine-induced myocardial infarction. Cancer 36(6):1979–1982
O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA et al (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 127(4):e362–e425. doi:10.1161/CIR.0b013e3182742cf6
Prosnitz RG, Marks LB (2005) Radiation-induced heart disease: vigilance is still required. J Clin Oncol 23(30):7391–7394. doi:10.1200/JCO.2005.07.011
Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA et al (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363(8):733–742. doi:10.1056/NEJMoa1000678
Velders MA, Boden H, Hofma SH, Osanto S, van der Hoeven BL, Heestermans AA et al (2013) Outcome after ST elevation myocardial infarction in patients with cancer treated with primary percutaneous coronary intervention. Am J Cardiol 112(12):1867–1872. doi:10.1016/j.amjcard.2013.08.019
Voskoboynik M, Urban D, Mileshkin L (2012) Early cardiovascular death in patients with cancer. N Engl J Med 367(16):1572–1573. doi:10.1056/NEJMc1209012
Yeh ET (2006) Cardiotoxicity induced by chemotherapy and antibody therapy. Annu Rev Med 57:485–498. doi:10.1146/annurev.med.57.121304.131240
Yusuf SW, Daraban N, Abbasi N, Lei X, Durand JB, Daher IN (2012) Treatment and outcomes of acute coronary syndrome in the cancer population. Clin Cardiol 35(7):443–450. doi:10.1002/clc.22007
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This study was based on a publicly available database of the US government which uses de-identified patient data. This article does not contain any studies with human participants or animals performed by any of the authors.
Appendix
Appendix
List of ICD-9-CM codes used for identification of medical comorbidities (Table 5).
Rights and permissions
About this article
Cite this article
Guddati, A.K., Joy, P.S. & Kumar, G. Analysis of outcomes of percutaneous coronary intervention in metastatic cancer patients with acute coronary syndrome over a 10-year period. J Cancer Res Clin Oncol 142, 471–479 (2016). https://doi.org/10.1007/s00432-015-2056-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-015-2056-5