Abstract
Severe respiratory syncytial virus (RSV) infection during infancy is associated with ongoing respiratory morbidity. In a large birth cohort of 2210 healthy preterm infants born at 32–35 weeks of gestation, we aimed to determine the role of atopy in the link between RSV hospitalization and current wheeze at age 6. We defined current wheeze as parent-reported wheeze or the use of respiratory medication in the past 12 months. Based on a positive family history of atopic disease, we distinguished between children with and without atopic predisposition. Six-year follow-up data was obtained in 997/1559 (64%) children of which 102 (10.2%) children had been hospitalized with RSV during infancy. Current wheeze was present in 184/997 (18.6%) children. RSV hospitalization was an independent risk factor for current wheeze in children without atopic predisposition (aOR 4.05 [95% CI 1.22–12.52]) but not in children with this atopic background (aOR 1.50 [95% CI 0.81–2.71]).
Conclusion: This is the largest published birth cohort demonstrating that in late preterm infants, atopic predisposition defines the relationship between RSV hospitalization and current wheeze. Future RSV prevention trials aiming to prevent ongoing respiratory symptoms should be analyzed separately for atopic status.
What is Known: • RSV infection is responsible for a significant burden of disease in young children worldwide. • Severe RSV infection in early life is associated with asthmatic symptoms later in life. | |
What is New: • This is the largest published birth cohort reporting about the role of atopic predisposition in the link between severe RSV infection and current wheeze at school age. • We show that RSV hospitalization in infancy is an independent risk factor for current wheeze in late preterm children without atopic predisposition at age 6. This was not seen in children with atopic predisposition. |

Similar content being viewed by others
Abbreviations
- OR:
-
Odds ratio
- aOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- LRTI:
-
Lower respiratory tract infection
- RSV:
-
Respiratory syncytial virus
- RSVH:
-
RSV hospitalization
- wGA:
-
Weeks gestational age
References
Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbald B, Stewart AW, Strachan D, Weiland SK, Williams HC (1995) International study of asthma and allergies in childhood (ISAAC): rationale and methods. Eur Respir J 8:483–491
Been JV, Lugtenberg MJ, Smets E, van Schayck CP, Kramer BW, Mommers M, Sheikh A (2014) Preterm birth and childhood wheezing disorders: a systematic review and meta-analysis. PLoS Med 11:e1001596
Blanken MO, Rovers MM, Molenaar JM, Winkler-Seinstra PL, Meijer A, Kimpen JL, Bont L, Dutch RSV Neonatal Network (2013) Respiratory syncytial virus and recurrent wheeze in healthy preterm infants. N Engl J Med 368:1791–1799
Blanken MO, Koffijberg H, Nibbelke EE, Rovers MM, Bont L, Dutch RSVNN (2013) Prospective validation of a prognostic model for respiratory syncytial virus bronchiolitis in late preterm infants: a multicenter birth cohort study. PLoS One 8:e59161
Carbonell-Estrany X, Perez-Yarza EG, Garcia LS, Guzman Cabanas JM, Boria EV, Atienza BB et al (2015) Long-term burden and respiratory effects of respiratory syncytial virus hospitalization in preterm infants-the SPRING study. PLoS One 10:e0125422
Groenwold RH, Donders AR, Roes KC, Harrell FE Jr, Moons KG (2012) Dealing with missing outcome data in randomized trials and observational studies. Am J Epidemiol 175:210–217
Haerskjold A, Kristensen K, Kamper-Jorgensen M, Nybo Andersen AM, Ravn H, Graff Stensballe L (2016) Risk factors for hospitalization for respiratory syncytial virus infection: a population-based cohort study of Danish children. Pediatr Infect Dis J 35:61–65
Hall CB, Weinberg GA, Iwane MK, Blumkin AK, Edwards KM, Staat MA, Auinger P, Griffin MR, Poehling KA, Erdman D, Grijalva CG, Zhu Y, Szilagyi P (2009) The burden of respiratory syncytial virus infection in young children. N Engl J Med 360:588–598
Henderson J, Hilliard TN, Sherriff A, Stalker D, Al Shammari N, Thomas HM (2005) Hospitalization for RSV bronchiolitis before 12 months of age and subsequent asthma, atopy and wheeze: a longitudinal birth cohort study. Pediatr Allergy Immunol 16:386–392
Koloski NA, Jones M, Eslick G, Talley NJ (2013) Predictors of response rates to a long term follow-up mail out survey. PLoS One 8:e79179
Korppi M, Piippo-Savolainen E, Korhonen K, Remes S (2004) Respiratory morbidity 20 years after RSV infection in infancy. Pediatr Pulmonol 38:155–160
Korsten K, Blanken MO, Nibbelke EE, Moons KG, Bont L, Dutch RSVNN (2016) Prediction model of RSV-hospitalization in late preterm infants: an update and validation study. Early Hum Dev 95:35–40
Lee C, Dobson AJ, Brown WJ, Bryson L, Byles J, Warner-Smith P, Young AF (2005) Cohort profile: the Australian longitudinal study on Women's health. Int J Epidemiol 34:987–991
Mochizuki H, Kusuda S, Okada K, Yoshihara S, Furuya H, Simoes EA (2017) Palivizumab prophylaxis in preterm infants and subsequent recurrent wheezing: 6 year follow up study. Am J Respir Crit Care Med 196:29–38
Mohangoo AD, de Koning HJ, Hafkamp-de Groen E, van der Wouden JC, Jaddoe VW, Moll HA, Hofman A, Mackenbach JP, de Jongste JC, Raat H (2010) A comparison of parent-reported wheezing or shortness of breath among infants as assessed by questionnaire and physician-interview: the generation R study. Pediatr Pulmonol 45:500–507
Pirzada A, Yan LL, Garside DB, Schiffer L, Dyer AR, Daviglus ML (2004) Response rates to a questionnaire 26 years after baseline examination with minimal interim participant contact and baseline differences between respondents and nonrespondents. Am J Epidemiol 159:94–101
Regnier SA, Huels J (2013) Association between respiratory syncytial virus hospitalizations in infants and respiratory sequelae: systematic review and meta-analysis. Pediatr Infect Dis J 32:820–826
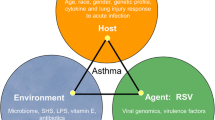
Rowe RK, Gill MA (2015) Asthma: the interplay between viral infections and allergic diseases. Immunol Allergy Clin N Am 35:115–127
Ruotsalainen M, Piippo-Savolainen E, Hyvarinen MK, Korppi M (2010) Respiratory morbidity in adulthood after respiratory syncytial virus hospitalization in infancy. Pediatr Infect Dis J 29:872–874
Saglani S (2013) Viral infections and the development of asthma in children. Ther Adv Infect Dis 1:139–150
Scheltema NM, Nibbelke EE, Pouw J, Blanken MO, Rovers MM, Naaktgeboren CA, Mazur NI, Wildenbeest JG, van der Ent CK, Bont LJ (2018) Respiratory syncytial virus prevention and asthma in healthy preterm infants: a randomised controlled trial. Lancet Respir Med 6:257–264
Shi T, McAllister DA, O'Brien KL, Simoes EAF, Madhi SA, Gessner BD, Polack FP, Balsells E, Acacio S, Aguayo C, Alassani I, Ali A, Antonio M, Awasthi S, Awori JO, Azziz-Baumgartner E, Baggett HC, Baillie VL, Balmaseda A, Barahona A, Basnet S, Bassat Q, Basualdo W, Bigogo G, Bont L, Breiman RF, Brooks WA, Broor S, Bruce N, Bruden D, Buchy P, Campbell S, Carosone-Link P, Chadha M, Chipeta J, Chou M, Clara W, Cohen C, de Cuellar E, Dang DA, Dash-Yandag B, Deloria-Knoll M, Dherani M, Eap T, Ebruke BE, Echavarria M, de Freitas Lázaro Emediato CC, Fasce RA, Feikin DR, Feng L, Gentile A, Gordon A, Goswami D, Goyet S, Groome M, Halasa N, Hirve S, Homaira N, Howie SRC, Jara J, Jroundi I, Kartasasmita CB, Khuri-Bulos N, Kotloff KL, Krishnan A, Libster R, Lopez O, Lucero MG, Lucion F, Lupisan SP, Marcone DN, McCracken J, Mejia M, Moisi JC, Montgomery JM, Moore DP, Moraleda C, Moyes J, Munywoki P, Mutyara K, Nicol MP, Nokes DJ, Nymadawa P, da Costa Oliveira MT, Oshitani H, Pandey N, Paranhos-Baccalà G, Phillips LN, Picot VS, Rahman M, Rakoto-Andrianarivelo M, Rasmussen ZA, Rath BA, Robinson A, Romero C, Russomando G, Salimi V, Sawatwong P, Scheltema N, Schweiger B, Scott JAG, Seidenberg P, Shen K, Singleton R, Sotomayor V, Strand TA, Sutanto A, Sylla M, Tapia MD, Thamthitiwat S, Thomas ED, Tokarz R, Turner C, Venter M, Waicharoen S, Wang J, Watthanaworawit W, Yoshida LM, Yu H, Zar HJ, Campbell H, Nair H, RSV Global Epidemiology Network (2017) Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. Lancet 390:946–958
Sigurs N, Bjarnason R, Sigurbergsson F, Kjellman B (2000) Respiratory syncytial virus bronchiolitis in infancy is an important risk factor for asthma and allergy at age 7. Am J Respir Crit Care Med 161:1501–1507
Sigurs N, Gustafsson PM, Bjarnason R, Lundberg F, Schmidt S, Sigurbergsson F, Kjellman B (2005) Severe respiratory syncytial virus bronchiolitis in infancy and asthma and allergy at age 13. Am J Respir Crit Care Med 171:137–141
Sigurs N, Aljassim F, Kjellman B, Robinson PD, Sigurbergsson F, Bjarnason R, Gustafsson PM (2010) Asthma and allergy patterns over 18 years after severe RSV bronchiolitis in the first year of life. Thorax 65:1045–1052
Simoes EA, Carbonell-Estrany X, Rieger CH, Mitchell I, Fredrick L, Groothuis JR et al (2010) The effect of respiratory syncytial virus on subsequent recurrent wheezing in atopic and nonatopic children. J Allergy Clin Immunol 126:256–262
Stensballe LG, Kristensen K, Simoes EA, Jensen H, Nielsen J, Benn CS et al (2006) Atopic disposition, wheezing, and subsequent respiratory syncytial virus hospitalization in Danish children younger than 18 months: a nested case-control study. Pediatrics 118:e1360–e1368
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Wadonda-Kabondo N, Sterne JA, Golding J, Kennedy CT, Archer CB, Dunnill MG et al (2004) Association of parental eczema, hayfever, and asthma with atopic dermatitis in infancy: birth cohort study. Arch Dis Child 89:917–921
Zomer-Kooijker K, van der Ent CK, Ermers MJ, Uiterwaal CS, Rovers MM, Bont LJ et al (2014) Increased risk of wheeze and decreased lung function after respiratory syncytial virus infection. PLoS One 9:e87162
Funding
This investigator-driven study was funded by a grant from the Netherlands Organization for Health Research and Development (NWO-AGIKO grant 920-035-89 to Dr. Blanken) and by an unrestricted grant from AbbVie. The study hypothesis, data collection, analysis, and interpretation were performed independently by the researchers. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript. The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the article. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
Koos Korsten designed the study, collected the data, drafted the manuscript, performed the analyses, and approved the manuscript to be published.
Maarten O. Blanken designed the study, critically reviewed the manuscript, and approved the manuscript to be published.
Brigitte J.M. Buiteman collected the data, critically reviewed the manuscript, and approved the manuscript to be published.
Elisabeth E. Nibbelke collected the data, critically reviewed the manuscript, and approved the manuscript to be published.
Christiana A. Naaktgeboren performed the analyses, critically reviewed the manuscript, and approved the manuscript to be published.
Louis J. Bont designed the study, critically reviewed the manuscript, and approved the manuscript to be published.
Joanne G. Wildenbeest drafted the manuscript, critically reviewed the manuscript, and approved the manuscript to be published.
Corresponding author
Ethics declarations
Ethics statement
The RISK study was reviewed and approved by the Institutional Review Board of the University Medical Centre Utrecht and subsequently approved by Institutional Review Boards of all participating hospitals. All parents provided written informed consent for screening of hospital records. The study was conducted in compliance with the Declaration of Helsinki and the standards of Good Clinical Practice. This manuscript was written according to the guidelines from the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [28].
Additional information
Communicated by Nicole Ritz
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplemental Table S1
(DOCX 199 kb)
Rights and permissions
About this article
Cite this article
Korsten, K., Blanken, M.O., Buiteman, B.J.M. et al. RSV hospitalization in infancy increases the risk of current wheeze at age 6 in late preterm born children without atopic predisposition. Eur J Pediatr 178, 455–462 (2019). https://doi.org/10.1007/s00431-018-03309-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-03309-0