Abstract
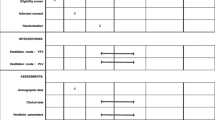
Evidence for target values of arterial oxygen saturation (SaO2), CO2, and pH has changed substantially over the last 20 years. A representative survey concerning treatment strategies in extremely low-birth-weight infants (ELBW) was sent to all German neonatal intensive care units (NICUs) treating ELBW infants in 1997. A follow-up survey was conducted in 2011 and sent to all NICUs in Germany, Austria, and Switzerland. During the observation period, NICUs targeting SaO2 of 80, 85, and 90 % have increased, while units aiming for 94 and 96 % decreased (all p < 0.001). Similarly, NICUs aiming for pH 7.25 or lower increased, while 7.35 or higher decreased (both p < 0.001). Furthermore, more units targeted a CO2 of 50 mmHg (7.3 kPa) or higher (p < 0.001), while fewer targeted 40 or 35 mmHg (p < 0.001). Non-invasive ventilation (NIV) was used in 80.2 % of NICUs in 2011. The most frequently used ventilation modes were synchronized intermittent mandatory ventilation (SIMV) (67.5 %) and intermittent positive pressure ventilation (IPPV) (59.7 %) in 1997 and SIMV (77.2 %) and synchronized intermittent positive pressure ventilation (SIPPV) (26.8 %) in 2011. NICUs reporting frequent or always use of IPPV decreased to 11.0 % (p < 0.001). SIMV (77.2 %) and SIPPV (26.8 %) did not change from 1997 to 2011, while high-frequency oscillation (HFO) increased from 9.1 to 19.7 % (p = 0.018). Differences between countries, level of care, and size of the NICU were minimal.
Conclusions: Target values for SaO2 decreased, while CO2 and pH increased significantly during the observation period. Current values largely reflect available evidence at time of the surveys.
What is Known: | |
• Evidence concerning target values of oxygen saturation, CO 2 , and pH in extremely low-birth-weight infants has grown substantially. • It is not known to which extent this knowledge is transferred into clinical practice and if treatment strategies have changed. | |
What is New: | |
• Target values for oxygen saturation in ELBW infants decreased between 1997 and 2011 while target values for CO 2 and pH increased. • Similar treatment strategies existed in different countries, hospitals of different size, or university versus nonuniversity hospitals in 2011. |



Similar content being viewed by others
Abbreviations
- BIPAP:
-
Biphasic positive airway pressure ventilation
- BPD:
-
Bronchopulmonary dysplasia
- ELBW:
-
Extremely low birth weight, less than 1000 g
- FiO2 :
-
Fraction of inspired oxygen
- GA:
-
Gestational age
- GNPI:
-
Gesellschaft für Neonatologie und pädiatrische Intensivmedizin, Society of Neonatology and Pediatric Intensive Care
- IVH:
-
Intraventricular hemorrhage
- IMV:
-
Intermittent mandatory ventilation
- IPPV:
-
Intermittent positive pressure ventilation
- NICU:
-
Neonatal intensive care unit
- NIV:
-
Non invasive ventilation
- pCO2 :
-
Partial pressure of carbon dioxide
- PEEP:
-
Positive end expiratory pressure
- PiP:
-
Peak inspiratory pressure
- RDS:
-
Respiratory distress syndrome
- SaO2 :
-
Arterial oxygen saturation
- SIMV:
-
Synchronized intermittent mandatory ventilation
- SIPPV:
-
Synchronized Intermittent positive pressure ventilation
- VG:
-
Volume guarantee ventilation
- VLBW:
-
Very low birth weight, less than 1500 g
References
Agresti A, Min Y (2001) On small-sample confidence intervals for parameters in discrete distributions. Biometrics 57(3):963–971
Askie LM, Henderson-Smart DJ, Ko H (2009) Restricted versus liberal oxygen exposure for preventing morbidity and mortality in preterm or low birth weight infants. Cochrane Database Syst Rev 1, CD001077. doi:10.1002/14651858.CD001077.pub2
Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, Adler A, Vera Garcia C, Rohde S, Say L, Lawn JE (2012) National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379(9832):2162–2172. doi:10.1016/S0140-6736(12)60820-4
Carlo WA, Finer NN, Walsh MC, Rich W, Gantz MG, Laptook AR, Yoder BA, Faix RG, Das A, Poole WK, Schibler K, Newman NS, Ambalavanan N, Frantz ID 3rd, Piazza AJ, Sanchez PJ, Morris BH, Laroia N, Phelps DL, Poindexter BB, Cotten CM, Van Meurs KP, Duara S, Narendran V, Sood BG, O’Shea TM, Bell EF, Ehrenkranz RA, Watterberg KL, Higgins RD (2010) Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med 362(21):1959–1969. doi:10.1056/NEJMoa0911781
Cheong JL, Anderson P, Roberts G, Duff J, Doyle LW (2013) Postnatal corticosteroids and neurodevelopmental outcomes in extremely low birthweight or extremely preterm infants: 15-year experience in Victoria, Australia. Arch Dis Child Fetal Neonatal Ed 98(1):F32–F36. doi:10.1136/fetalneonatal-2011-301355
Cooke RW (1981) Factors associated with periventricular haemorrhage in very low birthweight infants. Arch Dis Child 56(6):425–431
Duffett M, Burns KE, Adhikari NK, Arnold DM, Lauzier F, Kho ME, Meade MO, Hayani O, Koo K, Choong K, Lamontagne F, Zhou Q, Cook DJ (2012) Quality of reporting of surveys in critical care journals: a methodologic review. Crit Care Med 40(2):441–449. doi:10.1097/CCM.0b013e318232d6c6
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, Wrage LA, Poole K (2005) Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 116(6):1353–1360. doi:10.1542/peds. 2005-0249
Gerull R, Manser H, Kuster H, Arenz T, Nelle M, Arenz S (2013) Increase of caffeine and decrease of corticosteroids for extremely low birthweight infants with respiratory failure from 1997 to 2011. Acta Paediatr. doi:10.1111/apa.12419
Iriondo M, Thio M, Buron E, Salguero E, Aguayo J, Vento M (2009) A survey of neonatal resuscitation in Spain: gaps between guidelines and practice. Acta Paediatr 98(5):786–791. doi:10.1111/j.1651-2227.2009.01233.x
Kaiser JR, Gauss CH, Pont MM, Williams DK (2006) Hypercapnia during the first 3 days of life is associated with severe intraventricular hemorrhage in very low birth weight infants. J Perinatol 26(5):279–285. doi:10.1038/sj.jp.7211492
Kirpalani H, Millar D, Lemyre B, Yoder BA, Chiu A, Roberts RS (2013) A trial comparing noninvasive ventilation strategies in preterm infants. N Engl J Med 369(7):611–620. doi:10.1056/NEJMoa1214533
Laughon MM, Smith PB, Bose C (2009) Prevention of bronchopulmonary dysplasia. Semin Fetal Neonatal Med 14(6):374–382. doi:10.1016/j.siny.2009.08.002
Lemyre B, Davis PG, De Paoli AG, Kirpalani H (2014) Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev 9, CD003212. doi:10.1002/14651858.CD003212.pub2
Levene MI, Fawer CL, Lamont RF (1982) Risk factors in the development of intraventricular haemorrhage in the preterm neonate. Arch Dis Child 57(6):410–417
Levene MI, Shortland D, Gibson N, Evans DH (1988) Carbon dioxide reactivity of the cerebral circulation in extremely premature infants: effects of postnatal age and indomethacin. Pediatr Res 24(2):175–179. doi:10.1203/00006450-198808000-00007
Mariani G, Cifuentes J, Carlo WA (1999) Randomized trial of permissive hypercapnia in preterm infants. Pediatrics 104(5 Pt 1):1082–1088
Meneses J, Bhandari V, Alves JG (2013) Questions concerning nasal intermittent positive-pressure ventilation vs nasal continuous positive airway pressure—reply. JAMA Pediatr 167(9):873. doi:10.1001/jamapediatrics.2013.2212
Parsons PE, Eisner MD, Thompson BT, Matthay MA, Ancukiewicz M, Bernard GR, Wheeler AP (2005) Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med 33(1):1–6, discussion 230-232
Reiss I, Schaible T, van den Hout L, Capolupo I, Allegaert K, van Heijst A, Gorett Silva M, Greenough A, Tibboel D (2010) Standardized postnatal management of infants with congenital diaphragmatic hernia in Europe: the CDH EURO Consortium consensus. Neonatology 98(4):354–364. doi:10.1159/000320622
Ruegger C, Hegglin M, Adams M, Bucher HU (2012) Population based trends in mortality, morbidity and treatment for very preterm- and very low birth weight infants over 12 years. BMC Pediatr 12:17. doi:10.1186/1471-2431-12-17
Saugstad OD, Aune D (2014) Optimal oxygenation of extremely low birth weight infants: a meta-analysis and systematic review of the oxygen saturation target studies. Neonatology 105(1):55–63. doi:10.1159/000356561
Schmidt B, Whyte RK, Asztalos EV, Moddemann D, Poets C, Rabi Y, Solimano A, Roberts RS (2013) Effects of targeting higher vs lower arterial oxygen saturations on death or disability in extremely preterm infants: a randomized clinical trial. JAMA 309(20):2111–2120. doi:10.1001/jama.2013.5555
Short EJ, Kirchner HL, Asaad GR, Fulton SE, Lewis BA, Klein N, Eisengart S, Baley J, Kercsmar C, Min MO, Singer LT (2007) Developmental sequelae in preterm infants having a diagnosis of bronchopulmonary dysplasia: analysis using a severity-based classification system. Arch Pediatr Adolesc Med 161(11):1082–1087. doi:10.1001/archpedi.161.11.1082
Soll RF, Edwards EM, Badger GJ, Kenny MJ, Morrow KA, Buzas JS, Horbar JD (2013) Obstetric and neonatal care practices for infants 501 to 1500 g from 2000 to 2009. Pediatrics 132(2):222–228. doi:10.1542/peds. 2013-0501
Stenson B, Brocklehurst P, Tarnow-Mordi W (2011) Increased 36-week survival with high oxygen saturation target in extremely preterm infants. N Engl J Med 364(17):1680–1682. doi:10.1056/NEJMc1101319
Van de Bor M, Van Bel F, Lineman R, Ruys JH (1986) Perinatal factors and periventricular-intraventricular hemorrhage in preterm infants. Am J Dis Child 140(11):1125–1130
van Kaam AH, De Jaegere AP, Rimensberger PC (2013) Incidence of hypo- and hyper-capnia in a cross-sectional European cohort of ventilated newborn infants. Arch Dis Child Fetal Neonatal Ed 98(4):F323–F326. doi:10.1136/archdischild-2012-302649
van Kaam AH, Rimensberger PC, Borensztajn D, De Jaegere AP (2010) Ventilation practices in the neonatal intensive care unit: a cross-sectional study. J Pediatr 157(5):767–771 e761–763. doi:10.1016/j.jpeds.2010.05.043
Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network (2000). N Engl J Med 342(18):1301–1308. doi:10.1056/NEJM200005043421801
Villar J, Kacmarek RM, Perez-Mendez L, Aguirre-Jaime A (2006) A high positive end-expiratory pressure, low tidal volume ventilatory strategy improves outcome in persistent acute respiratory distress syndrome: a randomized, controlled trial. Crit Care Med 34(5):1311–1318. doi:10.1097/01.CCM.0000215598.84885.01
Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ, Simon NP, Wilson DC, Broyles S, Bauer CR, Delaney-Black V, Yolton KA, Fleisher BE, Papile LA, Kaplan MD (2000) Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993-1994. Pediatrics 105(6):1216–1226
Wallin LA, Rosenfeld CR, Laptook AR, Maravilla AM, Strand C, Campbell N, Dowling S, Lasky RE (1990) Neonatal intracranial hemorrhage: II. Risk factor analysis in an inborn population. Early Hum Dev 23(2):129–137
Wheeler KI, Klingenberg C, Morley CJ, Davis PG (2011) Volume-targeted versus pressure-limited ventilation for preterm infants: a systematic review and meta-analysis. Neonatology 100(3):219–227. doi:10.1159/000326080
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Funding
No sources of external funding
Authors’ contributions
The authors contributed to the manuscript in the following way: Roland Gerull was involved in the design of the second questionnaire, center recruitment, and data analysis and wrote the manuscript. Helen Manser was responsible for the second questionnaire in terms of design, development of the database, and data management and center recruitment. Tina Arenz was responsible for development and realization of the first survey. Helmut Küster supervised the development and contributed to the realization of the first survey. Stephan Arenz was responsible for center recruitment, development of the database of the second questionnaire, and data analysis and wrote parts of the manuscript. Mathias Nelle supervised the development and realization of the second survey, acquired hospital funds for the incentive, and was involved in writing the manuscript. All authors have participated in the concept and design, analysis and interpretation of data, and drafting or revising of the manuscript and contributed in discussions, reviews, and corrections of the submitted manuscript. All listed authors on the manuscript have seen and approved the submitted version of the manuscript and take full responsibility for the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Patrick Van Reempts
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 210 kb)
Rights and permissions
About this article
Cite this article
Gerull, R., Manser, H., Küster, H. et al. Less invasive ventilation in extremely low birth weight infants from 1997 to 2011: survey versus evidence. Eur J Pediatr 174, 1189–1196 (2015). https://doi.org/10.1007/s00431-015-2519-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-015-2519-3