Abstract
Purpose
The study’s purpose is to evaluate the long-term outcome after vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM) and to identify predictors of quality of life associated with intensive care.
Methods
Fifty-five patients who underwent open abdomen management at our institution from 2006 to 2013 were prospectively enrolled in this study. After a median follow-up period of 3.8 years, 27 patients completed the 36-Item Short Form Survey (SF-36) quality of life questionnaire. As this is a report solely focused on quality of life, direct treatment-related outcome measures like mortality, closure rates, and incisional hernia development of this study cohort have been reported previously.
Results
SF-36 physical role (54.6 ± 41.0 (0–100), p < 0.01), physical functioning (68.4 ± 29.5 (0–100), p = 0.01), and physical component summary (41.6 ± 13.0 (19–62), p = 0.01) scores for the patient population were significantly lower than normative scores. Significant correlations were found between physical functioning and total treatment costs (r = −0.66, p = 0.01), total units of packed red blood cells (r = −0.56, p = 0.04), and the complex intensive care scores (r = −0.50, p = 0.02). Simple and multiple regression analyses demonstrated that the complex intensive care score was the only predictor of physical functioning (R 2 = 0.50, β = −0.70, p = 0.02).
Conclusions
Despite high short-term mortality and morbidity rates for these critically ill patients, open abdomen treatment using VAWCM allows patients to recover to an acceptable long-term quality of life. The complex intensive care score can be used as a surrogate parameter for the global severity of illness and was the only predictor of physical functioning (SF-36).
Similar content being viewed by others
Introduction
In recent years, the open abdomen has become a common technique in the management of patients who require surgery for severe abdominal conditions [1]. Complex underlying conditions such as abdominal trauma, abdominal compartment syndrome, pancreatitis, and peritonitis are indications for leaving the abdomen open and are associated with high morbidity and mortality rates [2, 3]. Especially at the beginning of treatment, the management of an open abdomen presents enormous intensive care challenges [4–6].
The most common severe complications are ventilator-associated pneumonia (30%) and acute renal failure (22%), which adversely affect prognosis [6]. The most frequent cause of death is septic multi-organ failure [2, 4–10]. Depending on the underlying condition, the average length of intensive care unit (ICU) stay ranges from 13 to 65 days [7–12]. The mean perioperative mortality rate is 30% with a range from 10 to 61% [1–3, 8–10, 13, 14]. Patients experience an extremely critical phase that is characterized by a maximal compromise of physiological and mechanical integrity. They can survive only if they receive optimal intensive care and standardized surgical treatment [4–6]. During the course of treatment, they can develop a wide variety of complications [1, 4, 6], e.g., pneumonia (30%), acute renal failure (22%), and enteroatmospheric fistulas (1.3–54.8%). Furthermore, incisional hernias (32–100%), intra-abdominal abscesses (2.1–21%), postoperative adhesions, and impaired digestion (12%) can occur. Approximately 20% of the patients develop neurological and psychological problems as well as polyneuropathies [1, 4, 9, 15–18].
Outcome depends not only on direct surgical complications and the severity of the underlying condition but also on the type of intensive care and laparostomy management [1, 4, 5]. In recent years, open abdomen management has gone through various evolutions and, together with an optimization of intensive care support, has contributed to an improvement in survival rates and a decrease in the rates of complications and late effects [1, 18–21]. For the management of this complex condition, it is therefore of utmost importance that surgeons and intensive care specialists cooperate closely and coordinate surgical and non-surgical measures in order to achieve early fascial closure and minimize complication rates [5, 22]. In a different context, complex and prolonged intensive care was found to have considerable effects on long-term outcome [23, 24]. The combination of negative pressure therapy and mechanical fascial traction is the latest improvement of open abdomen management [1, 5, 18, 21, 25–27].
Available medium-term and long-term results after delayed primary fascial closure using vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM) are too few to provide the basis for recommendations that are supported by high-level evidence [1, 5, 21]. Only few studies on the outcome after VAWCM treatment have been published, yet [16, 17]. A report on directly treatment-related outcome measures like mortality, closure rates, and incisional hernia development of this study cohort has been published recently [18]. Even fewer studies focused especially on quality of life (QoL) like that by Petersson et al. [17]. Thus, there is hardly any existing evidence about this very critical outcome dimension after VAWCM. In particular, the influence of complex and invasive intensive treatment on the outcome after open abdomen management is currently unclear. Against this background, we conducted the present study to analyze in detail intensive care and associated parameters in order to quantify the cost, complexity, and intensity of treatment. In addition, we assessed quality of life as a relevant long-term parameter of the outcome of patients undergoing open abdomen management and investigated factors influencing quality of life.
Material and methods
Study population and open abdomen technique
Patients who underwent open abdomen (laparostomy) management at our institution between 1 July 2006 and 30 June 2013 were prospectively enrolled in this study. All patients or their authorized relatives gave their written informed consent for participation in the study, which had been approved by the ethics committee of the University of Mainz (No.: 837.238.14-9477). Excluded were patients whose open abdomen treatment had been initiated at another hospital. Accordingly, the only patients who were included had been managed on the basis of a standardized treatment approach (termed the Koblenz algorithm [18, 26]) from the beginning to the end of treatment.
All patients were treated in accordance with the Koblenz algorithm for managing the open abdomen, which has been described in detail elsewhere [18]. The algorithm uses a VAWCM technique similar to that described for the first time by Petersson et al. in 2007 [19, 26, 28].
Generally, the decision for leaving the abdomen open in this study cohort was made based on the following considerations:
-
1.
The intestines were too swollen to allow primary fascial closure (e.g., in the situation of an abdominal compartment syndrome or burst abdomen).
-
2.
A second look operation was necessary because of the intra-abdominal conditions (e.g., generalized peritonitis). Also, if the first operation was actually a damage control surgery (DCS) procedure or an abbreviated procedure in case of abdominal trauma or peritonitis, such a scenario caused an open abdomen therapy as, e.g., anastomoses would have been sewn in later operations.
As this is a report solely focused on quality of life, direct treatment-related outcome measures like mortality, closure rates, and incisional hernia development of this study cohort have been reported previously in detail [18]. With reference to that report, the study group consisted of 55 patients, 39 (70.9%) of whom were male and 16 (29.1%) were female. At the time of laparotomy, the mean age of the patients was 54 years. Inhospital mortality was 16.4%. The median duration of open abdomen management was 10.0 days with median 4.0 operations. Intestinal fistulas developed in 1.8% of the patients. Delayed primary fascial closure was achieved in 75% in an intention-to-treat analysis and 89% in a per-protocol analysis. The majority of patients (43.6%) required open abdomen management for peritonitis, followed by the group of patients with an abdominal compartment syndrome (ACS) or a burst abdomen (29.1%) and abdominal trauma (27.3%). The term ACS in this study was comprised of patients with massive intestinal edema, whose intestines became to swollen to close the fascia during the initial operation. In this context, we allocated patients in this group whenever the treating surgeon considered that situation as the actual reason for establishing an open abdomen. Hence, patients who developed an ACS after having an open abdomen due to a previous trauma or peritonitis were not suitable for the ACS group. At follow-up, incisional hernia rate was 35%. Of these, 42% had been surgically closed at our institution before follow-up.
Parameters
Apart from general patient data such as age and gender, we assessed the underlying conditions necessitating treatment and the indications for the open abdomen. All obtained study parameters are shown in Table 1; thus, here is only a brief explanation of the used scores given.
Mannheim Peritonitis Index
We used the Mannheim Peritonitis Index (MPI) to describe patients with peritonitis. This score was introduced in 1986 by Linder et al. [19] in order to estimate mortality in peritonitis patients. Designed as a sum score, MPI is based on age, sex, coexistent organ failure, presence of malignancy, preoperative duration of peritonitis, extent of peritonitis, and nature of exudate.
Injury Severity Score
The Injury Severity Score (ISS) was used to assess the severity of trauma. First published in 1974 by Baker et al., it has become widely used to quantify the severity of trauma [20]. Each injury is assigned an Abbreviated Injury Scale (AIS) score and allocated to one of six body regions; thus, the total score is equal to the ISS. It is common in the clinical routine to consider patients with an ISS score greater than 15 as polytrauma patients.
Simplified Acute Physiology Score II
The Simplified Acute Physiology Score (SAPS) is a score for measuring the physiological state of a patient and the risk of death independent of the underlying diagnosis [21].
Sepsis-Related Organ Failure Assessment
The Sepsis-Related Organ Failure Assessment score serves as a parameter that describes the course of organ dysfunction/failure during intensive care on the basis of six criteria [29].
The complex intensive care score is determined for every ICU patient on a daily basis in accordance with the coding guidelines of the German Institute of Medical Documentation and Information (Deutsches Institut für Medizinische Dokumentation und Information, DIMDI) and includes the SAPS II score [21] without the Glasgow Coma Scale (GCS) score and the Therapeutic Intervention Scoring System (TISS) Core-10 score, which comprises the ten elements of the TISS-28 [30] that require the most complex treatment [31]. The German hospital reimbursement system requires that complex intensive care scores be calculated on a daily basis for ICU patients who are older than 14 years of age [32]. We calculated summary scores for all days in the ICU.
In addition, we documented the length of ICU stay, the duration of mechanical ventilation, antibiotic therapy, the need for catecholamine therapy, and the need for blood products were examined as parameters correlated or associated with intensive care. At last, we obtained data on the costs of open abdomen management from the accounting department of our institution.
Follow-up
After discharge, all surviving patients were systematically followed up and invited for an examination. All follow-up examinations were conducted in a standardized manner and followed an identical approach. Apart from history taking and a physical examination by the investigator, we asked the patients to complete a 36-Item Short Form Survey (SF-36) questionnaire (QualityMetric, Inc., Lincoln, RI, USA) [33] in order to quantify quality of life. The SF-36 is a measure of physical and mental health [34]. It is a well-validated and widely used tool for assessing the effects of long treatment and chronic diseases. The responses are analyzed and used to calculate scores for eight domains describing physical and mental health. These scores can be compared with those obtained for other study cohorts or control groups. In addition, patients who had a hernia and did not undergo surgery formed a further subgroup that allowed us to assess how the presence of a hernia after open abdomen management influenced the quality of life. These scores were compared with normative data that had been reported for a German general population sample.
Statistical analysis
Data were collected and statistically analyzed using SPSS 22.0 (Statistical Package of the Social Sciences, SPSS, Inc., Chicago, IL, USA). The SPSS syntax file, which was part of the commercially available test kit [35], was used to calculate SF-36 scores. The test kit also included the normative scores obtained for a German general population sample in 1994. Inhospital data and posthospital data, which were collected at follow-up, were analyzed in an exploratory manner. Normally distributed data were reported as means ± standard deviations and ranges. Non-normally distributed data were presented as medians, interquartile ranges (IQRs), and ranges. Differences between groups were assessed using the t test for normally distributed data, the Mann-Whitney U test for non-normally distributed continuous data, and the chi-square test for dichotomous data. The level of significance was set at p <0.05. Pearson’s correlation coefficient was calculated to test for correlations between variables. The point biserial correlation coefficient was used for dichotomous variables. Simple and multiple regression analyses, using both the enter and stepwise methods, were performed to assess causal relationships.
Results
Intensive care
The results of the evaluation of intensive care-related parameters are given in Table 2. The mean ICU stay was 18 days including a mean ventilation period of about 100 h. Antibiotics were administered to almost all patients who were treated in the ICU over a period which corresponds to about half of the mean duration of ICU treatment. Our analysis showed that packed red blood cells (PRBCs) were given in about twice the cases compared to other blood products.
The mean complex intensive care score varied widely. It thus reflects the wide range of values obtained for the length of the ICU stay. All score results must be evaluated separately for the different indications for open abdomen management. Patients with ACS had a significantly lower SOFA score than patients with other indications. The mean ISS, which, of course, was calculated only for patients who required open abdomen management for trauma, was 34.0. The minimum score was 18, and the maximum score was 51. This is remarkable since all these patients thus were polytrauma patients as defined by an ISS equal to or greater than 16.
Similar to the complex intensive care score, which plays an important role in cost reimbursement, and the length of ICU stay, costs of management too varied widely. The daily costs of the management of a patient with peritonitis were significantly higher than the costs associated with other indications.
Follow-up
Overall mortality during the study period was 27% (Fig. 2). As a result, 40 patients (73%) were invited for a follow-up examination. Of these, 34 patients attended follow-up. This corresponds to a follow-up rate of 87% in a per-protocol analysis and 63% in an intention-to-treat analysis. The median time of follow-up was 3.8 years or 46 months (range 12–88 months). At this time point, the patients had a mean age of 56 (24–91) years. Twenty-seven patients in our follow-up group (79%) agreed to complete the SF-36 questionnaire.
Quality of life (SF-36)
Comparison with normative data
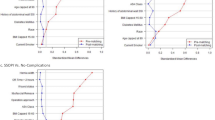
Table 3 as well as Figs. 1 and 2 provide an overview of the SF-36 scores that were obtained for the various domains in the entire study population and in the subgroups of patients with peritonitis, trauma, or ACS.
There were no significant differences in gender and mean age between our study population and the sample of the German population that had been investigated in 1994. Whereas there were no significant differences in the mental health domains, our study population had significantly lower scores for the physical component summary scale, which can be used as a surrogate for global physical function (Table 3, p = 0.01).
A comparison between the normative population and our subgroups of patients showed some noteworthy differences. Expectedly, patients with peritonitis (mean age 60.6 years) were older than the normative population (mean age 46.7 years, p = 0.01) and the proportion of men was considerably higher in the trauma subgroup (90.0%) than in the sample of the German population (44.4%, p < 0.01).
The scores obtained for the physical quality of life domains of the SF-36 (physical component summary scale, physical role, and physical functioning) in our study population were significantly lower than the normative scores. When we compared our patient subgroups that were formed on the basis of the indications for open abdomen management, we detected some significant differences between subgroups and the normative population.
The peritonitis group had significantly lower physical role scores (47.5 versus 80.7, p < 0.01) and physical component summary scores (41.3 versus 49.3, p = 0.02). The trauma group too had a lower physical role score (45.0 versus 80.7, p = 0.04). A further difference was found in the score for physical role between the subgroup of patients who presented with a hernia and the normative population (36.4 versus 80.7, p < 0.01). The score for general health perceptions was significantly lower in the ACS group when compared with normative data (49.3 versus 66.2, p = 0.04).
There were no significant differences in the mental quality of life domains of the SF-36. Neither the scores for the various mental domains nor the mental component summary score for our patient population were different from those for the German general population sample.
An analysis of the SF-36 scores for the patient subgroups that were formed on the basis of the indications for the open abdomen showed that there were only a few significant differences between the subgroups. The group of patients with ACS had a significantly higher physical role score than the peritonitis and trauma groups. A further analysis that involved the calculation of Pearson’s correlation coefficient did not reveal any relevant associations between the scores for the health domains and the summary components of the SF-36 and the various indications of open abdomen management. In our patient population, the indication for the open abdomen thus had no influence on the quality of life at the time of follow-up.
The development of an incisional hernia after fascial closure, however, affected a few health domains of the SF-36. Patients who presented with an incisional hernia at follow-up had a lower score for physical functioning when compared to both the entire study population (50.5 versus 68.4, p = 0.01) and the normative population (50.5 versus 83.9, p < 0.01). Likewise, the hernia group had lower scores for general health perceptions than the entire study population (47.3 versus 58.7, p = 0.04) and the normative population (47.3 versus 66.2, p < 0.01) as well as lower summary scores for the physical component than the study population (35.6 versus 41.6, p = 0.04) and the normative population (35.6 versus 49.3, p < 0.01).
By contrast, follow-up examinations did not reveal any differences between the group of patients without a hernia and either the entire study population or the normative population in the scores for the various physical and mental domains and the physical and mental component summary scores. The development of a hernia thus appears to be the strongest factor that adversely affects the physical domains of the SF36.
Factors influencing the quality of life (SF-36)
Tests for correlations between the various physical and mental domains and the physical and mental component summary scores of the SF-36 as dependent variables and the general, surgical, intensive care, and economic parameters listed in Table 1 demonstrated only a few relevant associations. There were moderate correlations between the number of transfused platelet units (r = −0.60, p = 0.40) and the total costs of management (r = −0.50, p = 0.08) and the physical component summary scale score, but the level of statistical significance was not reached. The total costs of management (r = −0.66, p = 0.01), the number of transfused PRBC units (r = −0.56, p = 0.04), and the complex intensive care score (r = −0.50, p = 0.02) were found to correlate with physical functioning. In addition, there was a high correlation between physical functioning and the number of transfused platelet units which, however, was not significant (r = −0.89, p = 0.11). We did not find any relevant correlations with the mental domains of the SF-36 and the other physical domains.
The aforementioned factors can be used as surrogate parameters for the severity of illness at the time of open abdomen management, and the correlation results may indicate possible causal relationships that were tested by regression analysis.
Simple regression analysis was performed in order to investigate factors that were found to be significantly correlated with physical functioning as the dependent variable. The coefficient of determination (R 2) of the relationship between physical functioning and total costs of management was 0.44, that between physical functioning and the number of transfused PRBC units was 0.32, and that between physical functioning and the complex intensive care score was 0.50.
In a further step, multiple regression analysis was performed. When all three factors were included in the regression model, R 2 was 0.51. The complex intensive care score was the most important predictor with the highest beta value (β = −0.53, p = 0.33), followed by the total costs of management (β = −0.16, p = 0.75) and the number of transfused PRBC units (β = −0.07, p = 0.88). When, however, this combination of variables was used, none of the factors was found to be a significant predictor of physical functioning since all beta coefficients failed to reach the level of significance.
In stepwise regression, the number of transfused PRBC units and the total costs of treatment were not included in the regression model because of the collinearity of these variables. As a result, the complex intensive care score was the only significant predictor of physical functioning (R 2 = 0.50, β = −0.70, p = 0.02). The complex intensive care score alone can thus be used as a surrogate parameter for the severity of illness during the ICU stay and can account for as much as 50% of the variability of physical functioning. The greater the severity of the disease of a patient undergoing open abdomen management in the ICU, the lower the score for physical functioning at follow-up and, accordingly, the poorer the subjective physical outcome of patients several years after treatment.
Discussion
If provided to the right patient at the right time, open abdomen treatment can reduce mortality in patients with severe intra-abdominal conditions [1, 5, 36–38]. The open abdomen remains a major interdisciplinary challenge for the entire team and requires close coordination of surgical procedures and intensive care [5]. Open abdomen management seriously compromises the mechanical and physiological integrity of the human organism [39]. In spite of all improvements in surgical methods and intensive care, the open abdomen is associated with high mortality and morbidity rates, which depend on the underlying pathology and the technique used [1, 5, 40, 41]. During the last decade, open abdomen techniques have gone through various dynamic evolutions and a wide variety of modifications have been introduced [28]. Currently, a combination of negative pressure therapy, fascial traction, and the use of a visceral protective layer appears to be the technically most advanced procedure [1, 5, 42]. This technique allows surgeons to address key factors and, in particular, to reduce inhospital complications [25, 26]. The focus of attention has been placed on long-term outcome and on identifying factors that make further improvements possible [1].
In the literature, there are only a few follow-up studies of patients who underwent open abdomen management in general and even fewer follow-up studies of patients who underwent VAWCM [9, 15, 16, 39, 43–45]. Particularly rare are studies that focus on assessing the patients’ quality of life as a measure of outcome of this invasive and lengthy treatment, which is physically and mentally distressing. In the absence of long-term results, it is at present impossible to provide recommendations for the management of the open abdomen which are based on evidence of high enough quality [1, 5].
There are substantial differences between studies not only in follow-up intervals and study criteria but also in the composition of patient populations and in open abdomen techniques. This makes a comparison of results very difficult [41]. In addition, studies on the open abdomen are based on only small numbers of patients. Three studies that address open abdomen management focus on abdominal wall integrity and hernia rates, which are not the central subject of this study [15, 16, 44]. Reported hernia rates range widely from 6% after 40 months to 66% after 5 years [15, 16, 44, 45]. Our hernia rate, i.e., 35% after 51 months, is thus in the middle range of values.
The study presented here shows that the entire patient population had significantly lower scores for physical functioning, physical role, and the physical component summary scale at follow-up after open abdomen management. A subgroup analysis revealed, however, that this difference applied only to the group of patients with a hernia. There was no difference between the subgroup of patients without a hernia and the normative population in any of the SF-36 domains. This finding is in line with a study by Cheatham et al. who reported a similar result [39]. The comparability of our study and the study by Cheatham et al. is, however, limited by substantial differences in the size and composition of the patient populations and the techniques used. Cheatham et al. investigated a total group of 30 patients and were able to follow up 13 of these patients. Unlike our patient group, these patients did not undergo open abdomen management with fascial traction [39]. Wondberg et al. examined a group of 30 patients with peritonitis. Of these patients, 53% attended follow-up. At follow-up, patients who underwent vacuum-assisted closure scored lower than the normal population on physical health domains and similar to the normal population on mental health domains. The authors, however, did not perform a subgroup analysis [45]. In a recently published study by Petersson on QoL after VAWMC treatment, they reported a follow-up rate of 91%, which is comparable with 87% in our study [17]. Moreover, they reported a higher incisional hernia incidence and conducted a QoL analysis based on SF-36 questionnaire as we did. In line with our findings, most of the physical component scores of SF-36 have been reported to be lower than the normative control. Conversely, they did not find an influence of having an incisional hernia on physical SF-36 subscores as we found physical component summary score, physical role, physical functioning, and general health perception to be significantly reduced in comparison with both the non-hernia group and the normative population [17].
In this context, however, the role of high primary fascial closure rates and the need of an evaluation of the prophylactic use of mesh for risk patients must be emphasized in efforts to minimize primary and secondary hernia rates [5, 15, 41, 46, 47]. Fortelny et al. reported that they occasionally used a prophylactic onlay mesh in risk patients and that these patients showed the lowest hernia rate after 40 months [44].
Our study demonstrates and quantifies the intensity, complexity, and high costs associated with the intensive care of patients undergoing open abdomen management. An analysis of the entire patient population reveals considerable variance and great interindividual differences. Our results for intensive care parameters are in the lower range of data reported so far [4]. In the literature, the length of ICU stay ranged between 7 and 52 days and the duration of ventilation between 5 and 32 days [2, 4, 6, 9, 10, 43, 45, 48, 49]. In our study, the durations of ICU treatment (18 days), ventilation, and open abdomen management were shorter than those reported by Perez et al. for patients with similar MPI scores and longer than those reported by Wondberg et al. for patients with lower MPI scores [43, 45]. In our study, the cost of treatment for trauma patients was EUR 75,169 and was thus considerably lower than the mean hospital charge reported by Vogel et al. for trauma patients with an almost identical ISS, i.e., USD 189,000 [7]. Compared with other studies, an ISS of 34 is in the upper range of scores reported in the literature [2, 7, 14, 49, 50].
The aforementioned findings suggest at least that VAWCM as described in our study is a technique that, compared with other studies, is associated with a short duration of intensive care during the open abdomen management of patients with the same severity of disease or injury. Our patient population is certainly too small, and the patient populations investigated in our study and other studies are too heterogeneous to allow any effects of different treatment modalities to be identified, especially since fascial traction and negative pressure are not always included in open abdomen management [7, 43, 45].
We examined a number of possible correlations between intensive care parameters and SF-36 outcome scores and detected only a few significant correlations. It should come as no surprise that a higher complex intensive care score, a higher number of transfused PRBC units, and higher costs of management, which can all be used as surrogate parameters for higher intensive care requirements, were associated with a lower physical functioning score. Physical functioning is an SF-36 domain that comprises ten items. More precisely, this domain is used to quantify the extent to which health places limits on physical activities such as bathing or dressing oneself, walking, climbing stairs, bending, lifting objects, or performing moderate activities [35].
Our study did not identify further significant correlations between intensive care parameters and outcome scores. We can therefore conclude that patients who survived the acute phase of open abdomen management can usually recover to previous levels of health despite intensive and invasive treatment and can achieve a posthospital health status that is similar to that of the general population. This finding is in line with a few rare studies in the literature [36, 43]. Perez et al. came to a similar conclusion after a follow-up of only 1 year [43]. Following a period of recovery, the majority of their patients (70–75%) reported that their quality of life and their participation in everyday life were good [9, 51, 52]. These results are important to note although the aforementioned studies are based only on Karnofsky and Rankin scores and not on the SF-36. If there is an indication for open abdomen management, surgeons must therefore not be hesitant to leave a patient’s abdomen open in spite of the invasive nature of the procedure and potential consequences of treatment [36].
Apart from these results, the present study also shows that comparisons are difficult because of the rarity of patients undergoing open abdomen management, the wide variety of open abdomen techniques, and the heterogeneity of patient populations. As a result, the current level of evidence is insufficient [5, 41, 53, 54]. At present, it is therefore impossible to provide recommendations and guidelines for the management of the open abdomen which are based on evidence of high enough quality [1, 5, 41].
Single-center studies are unlikely to improve the evidence base in this respect [1]. Open abdomen management is an accepted and known procedure, but it is relatively uncommon and is therefore not based on a standardized approach. In Germany, for example, a median number of five patients per hospital undergo open abdomen management every year [54]. The Open Abdomen Registry of the European Hernia Society, which is a module of the European Registry of Abdominal Wall Hernias (EuraHS, www.eurahs.eu), provides a promising source of prospective standardized multi-center data. This registry was established by the Surgical Working Group for Military and Emergency Surgery (CAMIN) of the German Society for General and Visceral Surgery (DGAV). Data will also be transferred to the Study, Documentation and Quality Center (StuDoQ) of the DGAV. Promising first-line results of this registry have been published recently [41].
Conclusion
In the present study, we demonstrated and quantified the complexity and intensity of intensive care for patients undergoing open abdomen management for different types of indications. In terms of long-term outcome, patients who survive the critical acute phase of treatment can recover to previous levels of physical and mental health. Exceptions are patients who develop an abdominal wall hernia after open abdomen management. These patients have significantly lower physical health scores. For this reason, ventral hernias following open abdomen management should be avoided in risk patients either by high rates of delayed primary closure or by secondary fascial closure using an optimized technique with or without the preventive use of mesh.
The complex intensive care score was identified as a multi-factorial surrogate parameter for the global severity of illness and as a predictor of a poorer quality of life and, in particular, of lower scores for physical functioning during the ICU stay. This underlines the complexity of open abdomen treatment and the interdisciplinary challenge that intensive care specialists and surgeons have to face in their efforts to achieve an optimal outcome and, in particular, the best possible quality of life for patients.
Study limitations
The present study is limited by the relatively small patient population and by the single-center setting. Moreover, subgroup analyses in a small population can only be interpreted with caution. In addition, the comparability of the results presented here and those reported in other studies is limited. Even between the present study and two similar studies, there are differences in study design and the technique used [15, 16, 36, 44]. Moreover, there are substantial differences in the study populations, which is a general problem in assessing the evidence on open abdomen techniques [1, 5, 53].
References
Atema JJ, Gans SL, Boermeester MA (2015) Systematic review and meta-analysis of the open abdomen and temporary abdominal closure techniques in non-trauma patients. World J Surg 39:912–925
Miller RS, Morris JA, Diaz JJ, Herring MB, May AK (2005) Complications after 344 damage-control open celiotomies. J Trauma 59:1365–1371 discussion 1371-4
Rasilainen SK, Mentula PJ, Leppäniemi AK (2012) Vacuum and mesh-mediated fascial traction for primary closure of the open abdomen in critically ill surgical patients. Br J Surg 99:1725–1732
Jannasch O, Tautenhahn J, Lippert H, Meyer F (2011) Temporary abdominal closure and early and late pathophysiological consequences of treating an open abdomen. Zentralbl Chir 136:575–584
Coccolini F, Biffl W, Catena F, Ceresoli M, Chiara O et al (2015) The open abdomen, indications, management and definitive closure. World J Emerg Surg 10:32
Balentine C, Subramanian A, Palacio CH, Sansgiry S, Berger DH et al (2009) AVAS Best Clinical Resident Award (Tied): management and outcomes of the open abdomen in nontrauma patients. Am J Surg 198:588–592
Vogel TR, Diaz JJ, Miller RS, May AK, Guillamondegui OD et al (2006) The open abdomen in trauma: do infectious complications affect primary abdominal closure? Surg Infect 7:433–441
Bertram P, Schachtrupp A, Rosch R, Schumacher O, Schumpelick V (2006) Abdominal compartment syndrome. Chirurg 77:573–574 576-9
Bosscha K, Reijnders K, Jacobs MH, Post MW, Algra A et al (2001) Quality of life after severe bacterial peritonitis and infected necrotizing pancreatitis treated with open management of the abdomen and planned re-operations. Crit Care Med 29:1539–1543
Chavarria-Aguilar M, Cockerham WT, Barker DE, Ciraulo DL, Richart CM et al (2004) Management of destructive bowel injury in the open abdomen. J Trauma 56:560–564
Wild T, Stremitzer S, Budzanowski A, Rinder H, Tamandl D et al (2004) Abdominal dressing—a new method of treatment for open abdomen following secondary peritonitis. Zentralbl Chir 129(Suppl 1):S20–S23
Batacchi S, Matano S, Nella A, Zagli G, Bonizzoli M et al (2009) Vacuum-assisted closure device enhances recovery of critically ill patients following emergency surgical procedures. Crit Care 13:R194
Oetting P, Rau B, Schlag PM (2006) Abdominal vacuum device with open abdomen. Chirurg 77(586):588–593
Tremblay LN, Feliciano DV, Schmidt J, Cava RA, Tchorz KM et al (2001) Skin only or silo closure in the critically ill patient with an open abdomen. Am J Surg 182:670–675
Brandl A, Laimer E, Perathoner A, Zitt M, Pratschke J et al (2014) Incisional hernia rate after open abdomen treatment with negative pressure and delayed primary fascia closure. Hernia 18:105–111
Bjarnason T, Montgomery A, Ekberg O, Acosta S, Svensson M et al (2013) One-year follow-up after open abdomen therapy with vacuum-assisted wound closure and mesh-mediated fascial traction. World J Surg 37:2031–2038
Petersson U, Bjarnason T, Björck M, Montgomery A, Rogmark P et al (2016) Quality of life and hernia development 5 years after open abdomen treatment with vacuum-assisted wound closure and mesh-mediated fascial traction. Hernia 20:755–764
Willms A, Schaaf S, Schwab R, Richardsen I, Bieler D et al (2016) Abdominal wall integrity after open abdomen: long-term results of vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM). Hernia 20:849–858
Linder M, Wacha H, Wesch G, Feldmann U (1986) Welche klinischen Faktoren beeinflussen die Letalität bei bakterieller Peritonitis: Mannheimer Peritonitis-Index (MPI). Langenbeck’s Arch Surg 369:788–788
Baker SP, O’Neill B, Haddon W, Long WB (1974) The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14: 187–196.
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Hecker A, Hecker B, Hecker M, Riedel JG, Weigand MA et al (2016) Acute abdominal compartment syndrome: current diagnostic and therapeutic options. Langenbeck’s Arch Surg 401:15–24
Cuthbertson BH, Elders A, Hall S, Taylor J, MacLennan G et al (2013) Mortality and quality of life in the five years after severe sepsis. Crit Care 17:R70
Nesseler N, Defontaine A, Launey Y, Morcet J, Mallédant Y et al (2013) Long-term mortality and quality of life after septic shock: a follow-up observational study. Intensive Care Med 39:881–888
Acosta S, Bjarnason T, Petersson U, Pålsson B, Wanhainen A et al (2011) Multicentre prospective study of fascial closure rate after open abdomen with vacuum and mesh-mediated fascial traction. Br J Surg 98:735–743
Willms A, Güsgen C, Schaaf S, Bieler D, von Websky M et al (2015) Management of the open abdomen using vacuum-assisted wound closure and mesh-mediated fascial traction. Langenbeck’s Arch Surg 400:91–99
Kafka-Ritsch R, Birkfellner F, Perathoner A, Raab H, Nehoda H et al (2012) Damage control surgery with abdominal vacuum and delayed bowel reconstruction in patients with perforated diverticulitis Hinchey III/IV. J Gastrointest Surg 16:1915–1922
Petersson U, Acosta S, Björck M (2007) Vacuum-assisted wound closure and mesh-mediated fascial traction—a novel technique for late closure of the open abdomen. World J Surg 31:2133–2137
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Moreno R, Morais P (1997) Validation of the simplified therapeutic intervention scoring system on an independent database. Intensive Care Med 23:640–644
DIMDI (2016) Dokumentationsvorgaben zur Erfassung der IntensivmedizinischenKomplexbehandlung. Last accessed 19 May 2016
Hoehn T, Drabik A, Lehmann C, Christaras A, Stannigel H et al (2008) Correlation between severity of disease and reimbursement of costs in neonatal and paediatric intensive care patients. Acta Paediatr 97:1438–1442
Tarlov AR, Ware JE, Greenfield S, Nelson EC, Perrin E et al (1989) The medical outcomes study. An application of methods for monitoring the results of medical care. JAMA 262:925–930
Ware JE, Kosinski M (2001) SF-36 physical and mental health summary scales: a manual for users of version 1, Second edn. QualityMetric Incorporated, Lincoln
Morfeld M, Kirchberger I, Bullinger M (2011) SF-36 Fragebogen zum Gesundheitszustand, 2. Aufl edn. Hogrefe, Göttingen
Cheatham ML, Safcsak K (2010) Is the evolving management of intra-abdominal hypertension and abdominal compartment syndrome improving survival? Crit Care Med 38:402–407
Sartelli M, Abu-Zidan FM, Ansaloni L, Bala M, Beltrán MA et al (2015) The role of the open abdomen procedure in managing severe abdominal sepsis: WSES position paper. World J Emerg Surg 10:35
Boele van Hensbroek P, Wind J, Dijkgraaf MG, Busch OR, Goslings JC et al (2009) Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg 33:199–207
Cheatham ML, Safcsak K, Llerena LE, Morrow CE, Block EF (2004) Long-term physical, mental, and functional consequences of abdominal decompression. J Trauma 56:237–241 discussion 241-2
De Waele JJ, Hoste EA, Malbrain ML (2006) Decompressive laparotomy for abdominal compartment syndrome—a critical analysis. Crit Care 10:R51
Willms A, Muysoms F, Güsgen C, Schwab R, Lock J, et al. (2017) The open abdomen route by EuraHS: introduction of the data set and initial results of procedures and procedure-related complications. Hernia
Bruhin A, Ferreira F, Chariker M, Smith J, Runkel N (2014) Systematic review and evidence based recommendations for the use of negative pressure wound therapy in the open abdomen. International Journal of Surgery, London
Perez D, Wildi S, Demartines N, Bramkamp M, Koehler C et al (2007) Prospective evaluation of vacuum-assisted closure in abdominal compartment syndrome and severe abdominal sepsis. J Am Coll Surg 205:586–592
Fortelny RH, Hofmann A, Gruber-Blum S, Petter-Puchner AH, Glaser KS (2013) Delayed closure of open abdomen in septic patients is facilitated by combined negative pressure wound therapy and dynamic fascial suture. Surg Endosc
Wondberg D, Larusson HJ, Metzger U, Platz A, Zingg U (2008) Treatment of the open abdomen with the commercially available vacuum-assisted closure system in patients with abdominal sepsis: low primary closure rate. World J Surg 32:2724–2729
El-Khadrawy OH, Moussa G, Mansour O, Hashish MS (2009) Prophylactic prosthetic reinforcement of midline abdominal incisions in high-risk patients. Hernia 13:267–274
Hollinsky C, Sandberg S, Kocijan R (2007) Preliminary results with the reinforced tension line: a new technique for patients with ventral abdominal wall hernias. Am J Surg 194:234–239
Nieuwenhuijs VB, Besselink MG, van Minnen LP, Gooszen HG (2003) Surgical management of acute necrotizing pancreatitis: a 13-year experience and a systematic review. Scand. J. Gastroenterol. Suppl: 111–6
Teixeira PG, Salim A, Inaba K, Brown C, Browder T et al (2008) A prospective look at the current state of open abdomens. Am Surg 74:891–897
Kritayakirana K, Maggio PM, Brundage S, Purtill MA, Staudenmayer K et al (2010) Outcomes and complications of open abdomen technique for managing non-trauma patients. J Emerg Trauma Shock 3:118–122
Fenton-Lee D, Imrie CW (1993) Pancreatic necrosis: assessment of outcome related to quality of life and cost of management. Br J Surg 80:1579–1582
Eder F, Tautenhahn J, Lippert H (2006) Late complications of open abdomen. Chirurg 77:602–609
Open Abdomen Advisory Panel, Campbell A, Chang M, Fabian T, Franz M et al (2009) Management of the open abdomen: from initial operation to definitive closure. Am Surg 75:S1–22
Herrle F, Hasenberg T, Fini B, Jonescheit J, Shang E et al (2011) Open abdomen 2009. A national survey of open abdomen treatment in Germany. Chirurg 82:684–690
Acknowledgements
The authors would like to thank Barbara Isenberg from the German Office of Languages in Hürth for the linguistic advise.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No funding was received for this work.
The data reported here contain results of a yet unpublished doctoral thesis.
Rights and permissions
About this article
Cite this article
Willms, A., Schaaf, S., Schwab, R. et al. Intensive care and health outcomes of open abdominal treatment: long-term results of vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM). Langenbecks Arch Surg 402, 481–492 (2017). https://doi.org/10.1007/s00423-017-1575-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-017-1575-8