Abstract
Background and aims
A contaminated or infected surgical site is considered a contraindication for the use of the nonabsorbable alloplastic materials employed to repair abdominal wall defects. Therefore, the biocompatibility of new prosthetic materials was investigated.
Materials and methods
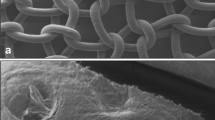
Meshes measuring 1.5×1.5 cm made of conventional and titanium-coated polypropylene, polyglycol, or porcine dermal collagen were implanted under the abdominal wall of 96 rats (eight groups of 12 animals each) employing the inlay technique. Implantation of all four materials was performed both under semisterile conditions and bacterial contamination of the mesh. The meshes were explanted after 28 days.
Results
All the materials implanted under semisterile conditions were incorporated into the abdominal wall with only few intraabdominal adhesions (mean adhesion scores: 1.0, 1.2, 1.0, 0.8 points, respectively, not significant). With the porcine dermal collagen, proliferation rate and the proportion of inflammatory cells were statistically lower (p<0.01). In the bacterial contamination group, all meshes were associated with a suppurating infection and strong adhesions between the bowel and mesh, which were most prominent in the case of dermal collagen (mean adhesion scores: 1.6, 1.7, 1.7, and 1.9 points, respectively, not significant). In this group, two animals died of peritonitis. In comparison with the other materials, the proliferation rate was significantly elevated (p=0.03). No significant differences were seen between the other materials employed.
Conclusion
Irrespective of the material employed, implantation of alloplastic meshes in an abdominal wall contaminated with bacteria, is associated with suppurating infections, in particular in the case of the membrane-like porcine dermal collagen. Nonabsorbable alloplastic meshes and dermal skin grafts should therefore not be used to repair infected abdominal wall defects.


Similar content being viewed by others
References
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343(6):392–398
Korenkov M, Sauerland S, Arndt M, Bograd L, Neugebauer EA, Troidl H (2002) Randomized clinical trial of suture repair, polypropylene mesh or autodermal hernioplasty for incisional hernia. Br J Surg 89(1):50–56
Flum DR, Horvath K, Koepsell T (2003) Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg 237(1):129–135
Law NW, Ellis H (1991) A comparison of polypropylene mesh and expanded polytetrafluoroethylene patch for the repair of contaminated abdominal wall defects—an experimental study. Surgery 109(5):652–655
Scheidbach H, Tannapfel A, Schmidt U, Lippert H, Köckerling F (2004) Influence of titanium coating on the biocompatibility of a heavyweight polypropylene mesh. An animal experimental model. Eur Surg Res 36(5):313–317
Chaplin JM, Costantino PD, Wolpoe ME, Bederson JB, Griffey ES, Zhang WX (1999) Use of an acellular dermal allograft for dural replacement: an experimental study. Neurosurgery 45:320–327
Klinge U, Junge K, Spellerberg B, Piroth C, Klosterhalfen B, Schumpelick V (2002) Do multifilament alloplastic meshes increase the infection rate? Analysis of the polymeric surface, the bacteria adherence, and the in vivo consequences in a rat model. J Biomed Mater Res 63:765–771
van ‘t Riet M, de Vos van Steenwijk PJ, Bonthuis F, Marquet RL, Steyerberg EW, Jeekel J, Bonjer HJ (2003) Prevention of adhesion to prosthetic mesh: comparison of different barriers using an incisional hernia model. Ann Surg 237(1):123–128
Lopez Villalta GC, Furio-Bacete V, Ortiz Oshiro E, Lopez DO, Vaca Vaticon D, Fdez-Represa JA (1995) Experimentally contaminated reabsorbable meshes: their evolution in abdominal wall defects. Int Surg 80(3):223–226
Junge K, Rosch R, Klinge U, Saklak M, Klosterhalfen B, Peiper C, Schumpelick V (2005) Titanium coating of a polypropylene mesh for hernia repair: effect on biocompatibility. Hernia 9(2):115–119
Birolini C, Utiyama EM, Rodrigues AJ Jr, Birolini D (2000) Elective colonic operation and prosthetic repair of incisional hernia: does contamination contraindicate abdominal wall prosthesis use? J Am Coll Surg 191(4):366–372
Leber GE, Garb JL, Alexander AI, Reed WP (1998) Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 133(4):378–382
Vrijland WW, Jeekel J, Steyerberg EW, Den Hoed PT, Bonjer HJ (2000) Intraperitoneal polypropylene mesh repair of incisional hernia is not associated with enterocutaneous fistula. Br J Surg 87(3):348–352
Costerton JW, Stewart PS, Greenberg EP (1999) Bacterial biofilms: a common cause of persistent infections. Science 284:1318–1321
An YH, Friedman RJ (1998) Concise review of bacterial adhesion to biomaterial surfaces. J Biomed Mater Res 43:338–348
Bellon JM, Garcia-Carranza A, Garcia-Honduvilla N, Carrera-San Martin A, Bujan J (2004) Tissue integration and biochemical behaviour of contaminated experimental polypropylene and expanded polytetrafluoroethylene implants. Br J Surg 91:489–494
Bellon JM, Contreras LA, Bujan J (2000) Ultrastructural alterations of polytetrafluoroethylene prostheses implanted in abdominal wall provoked by infection: clinical and experimental study. World J Surg 24:528–532
Bleichrodt RP, Simmermacher RK, van der Lei B, Schakenraad JM (1993) Expanded polytetrafluoroethylene patch versus polypropylene mesh for the repair of contaminated defects of the abdominal wall. Surg Gynecol Obstet 176(1):18–24
Junge K, Rosch R, Klinge U, Krones C, Klosterhalfen B, Mertens PR, Lynen P, Kunz D, Preiss A, Peltroche-Llacsahuanga H, Schumpelick V (2005) Gentamicin supplementation of polyvinylidenfluoride mesh materials for infection prophylaxis. Biomaterials 26(7):787–793
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ott, R., Hartwig, T., Tannapfel, A. et al. Biocompatibility of bacterial contaminated prosthetic meshes and porcine dermal collagen used to repair abdominal wall defects. Langenbecks Arch Surg 392, 473–478 (2007). https://doi.org/10.1007/s00423-006-0080-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-006-0080-2