Abstract
Purpose
The purpose of this study was to investigate whether scheduling meals earlier in the day affects the circadian phase of the cardiac autonomic nervous system as assessed by heart rate variability (HRV) and serum lipid levels.
Methods
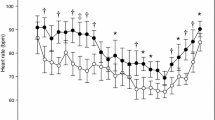
Healthy men aged 21.4 ± 0.5 years (n = 14) with a habit of regularly skipping breakfast participated in this parallel trial involving altered feeding schedules. Participants in the early mealtime group (EM group, n = 8) were asked to eat three meals at 8:00, 13:00, and 18:00, and the control group (n = 6) ate at 13:00, 18:00, and 23:00 for 2 weeks. On the measurement day before and after intervention, fasting blood samples and 24-h electrocardiograph recordings were collected. Spectral analysis was used for approximate 10-min HRV segments. Low frequency (LF) power, high frequency (HF) power, and the ratio of HF to total power (%HF) were calculated to assess sympathovagal balance. Acrophases of the circadian rhythm of HRV variables were obtained by nonlinear least squares regression.
Results
Triglyceride and total and LDL cholesterol levels were significantly decreased in the EM group when compared with the control group (p = 0.035, 0.008, and 0.004, respectively). Acrophases for HRV variables were advanced in the EM group and their difference between before and after the intervention in LF power (−3.2 ± 1.2 h) and %HF (−1.2 ± 0.5 h) reached significant level, respectively (p < 0.05).
Conclusions
Timing of meals was a key factor in regulating circadian phases of the cardiac autonomic nervous system and lipid metabolism.




Similar content being viewed by others
Abbreviations
- Bmal1:
-
Brain and muscle arnt-like protein-1
- BMI:
-
Body mass index
- ECG:
-
Electrocardiography
- HF power:
-
High frequency power
- HOMA-β:
-
Homeostasis model assessment for beta cell function
- HOMA-IR:
-
Homeostasis model assessment for insulin resistance
- HR:
-
Heart rate
- HRV:
-
Heart rate variability
- LF power:
-
Low frequency power
- NEFA:
-
Non-esterified fatty acid
- RRI:
-
R–R intervals
- TG:
-
Triglyceride
- %HF:
-
The ratio of HF to total power
References
Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ (1981) Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science 213:220–222
Boudreau P, Dumont G, Kin NM, Walker CD, Boivin DB (2011) Correlation of heart rate variability and circadian markers in humans. Conf Proc IEEE Eng Med Biol Soc, pp 681–682
DeBoer RW, Karemaker JM, Strackee J (1984) Comparing spectra of a series of point events particularly for heart rate variability data. IEEE Transac Bio-med Eng 31:384–387
Farshchi HR, Taylor MA, Macdonald IA (2005) Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr 81:388–396
Fuller PM, Lu J, Saper CB (2008) Differential rescue of light- and food-entrainable circadian rhythms. Science 320:1074–1077
Goel N, Stunkard AJ, Rogers NL, Van Dongen HP, Allison KC, O’Reardon JP, Ahima RS, Cummings DE, Heo M, Dinges DF (2009) Circadian rhythm profiles in women with night eating syndrome. J Biol Rhy 24:85–94
Hamilton PS, Tompkins WJ (1986) Quantitative investigation of QRS detection rules using the MIT/BIH arrhythmia database. IEEE Trans Bio-med Eng 33:1157–1165
Hastings MH, Reddy AB, Maywood ES (2003) A clockwork web: circadian timing in brain and periphery, in health and disease. Nat Rev Neurosci 4:649–661
Hilton MF, Umali MU, Czeisler CA, Wyatt JK, Shea SA (2000) Endogenous circadian control of the human autonomic nervous system. Comput Cardiol 27:197–200
Krauchi K, Wirz-Justice A (1994) Circadian rhythm of heat production, heart rate, and skin and core temperature under unmasking conditions in men. Am J Physiol 267:R819–R829
Malliani A, Pagani M, Lombardi F, Cerutti S (1991) Cardiovascular neural regulation explored in the frequency domain. Circulation 84:482–492
Massin MM, Maeyns K, Withofs N, Ravet F, Gerard P (2000) Circadian rhythm of heart rate and heart rate variability. Arch Dis Child 83:179–182
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Mendoza J (2007) Circadian clocks: setting time by food. J Neuroendocrinol 19:127–137
Mieda M, Williams SC, Richardson JA, Tanaka K, Yanagisawa M (2006) The dorsomedial hypothalamic nucleus as a putative food-entrainable circadian pacemaker. Proc Natl Acad Sci USA 103:12150–12155
Ministry of Health Labor and Welfare (2011) National health and nutrition examination survey. http://www.mhlw.go.jp/seisakunitsuite/bunya/kenkou_iryou/kenkou/
Nelson W, Tong YL, Lee JK, Halberg F (1979) Methods for cosinor-rhythmometry. Chronobiologia 6:305–323
Nguyen J, Wright KP Jr (2009) Influence of weeks of circadian misalignment on leptin levels. Nat Sci Sleep 2010:9–18
Niedhammer I, Lert F, Marne MJ (1996) Prevalence of overweight and weight gain in relation to night work in a nurses’ cohort. Intern J Obes Relat Metab Disord J Intern Assoc Study Obes 20:625–633
Resnicow K (1991) The relationship between breakfast habits and plasma cholesterol levels in schoolchildren. J Sch Health 61:81–85
Ribeiro DC, Hampton SM, Morgan L, Deacon S, Arendt J (1998) Altered postprandial hormone and metabolic responses in a simulated shift work environment. J Endocrinol 158:305–310
Sakamoto N, Yoshiuchi K, Kikuchi H, Takimoto Y, Kaiya H, Kumano H, Yamamoto Y, Akabayashi A (2008) Panic disorder and locomotor activity. Bio Psycho Soc Med 2:23
Scheer FA, Ter Horst GJ, van Der Vliet J, Buijs RM (2001) Physiological and anatomic evidence for regulation of the heart by suprachiasmatic nucleus in rats. Am J Physiol Heart Circ Physiol 280:H1391–H1399
Scheer FA, Hilton MF, Mantzoros CS, Shea SA (2009) Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA 106:4453–4458
Shimba S, Ishii N, Ohta Y, Ohno T, Watabe Y, Hayashi M, Wada T, Aoyagi T, Tezuka M (2005) Brain and muscle Arnt-like protein-1 (BMAL1), a component of the molecular clock, regulates adipogenesis. Proc Natl Acad Sci USA 102:12071–12076
Smith KJ, Gall SL, McNaughton SA, Blizzard L, Dwyer T, Venn AJ (2010) Skipping breakfast: longitudinal associations with cardio-metabolic risk factors in the childhood determinants of adult health study. Am J Clin Nutr 92:1316–1325
Stanton JL Jr, Keast DR (1989) Serum cholesterol, fat intake, and breakfast consumption in the United States adult population. J Am Coll Nutr 8:567–572
Suwazono Y, Dochi M, Sakata K, Okubo Y, Oishi M, Tanaka K, Kobayashi E, Kido T, Nogawa K (2008) A longitudinal study on the effect of shift work on weight gain in male Japanese workers. Obesity (Silver Spring) 16:1887–1893
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation 93:1043–1065
Togo F, Yamamoto Y (2001) Decreased fractal component of human heart rate variability during non-REM sleep. Am J Physiol Heart Circ Physiol 280:H17–H21
Turek FW, Joshu C, Kohsaka A, Lin E, Ivanova G, McDearmon E, Laposky A, Losee-Olson S, Easton A, Jensen DR, Eckel RH, Takahashi JS, Bass J (2005) Obesity and metabolic syndrome in circadian clock mutant mice. Science 308:1043–1045
Vandewalle G, Middleton B, Rajaratnam SM, Stone BM, Thorleifsdottir B, Arendt J, Dijk DJ (2007) Robust circadian rhythm in heart rate and its variability: influence of exogenous melatonin and photoperiod. J Sleep Res 16:148–155
Yamamoto Y, Hughson RL (1991) Coarse-graining spectral analysis: new method for studying heart rate variability. J Appl Physiol 71:1143–1150
Yamamoto Y, Hughson RL (1994) On the fractal nature of heart rate variability in humans: effects of data length and beta-adrenergic blockade. Am J Physiol 266:R40–R49
Yoshida C, Shikata N, Seki S, Koyama N, Noguchi Y (2012) Early nocturnal meal skipping alters the peripheral clock and increases lipogenesis in mice. Nut Metab 9:78
Yoshizaki T, Tada Y, Kodama T, Mori K, Kokubo Y, Hida A, Mitani K, Komatsu T, Togo F, Kawano Y (2010) Influence of shiftwork on association between body mass index and lifestyle or dietary habits in female nurses and caregivers. J Jpn Soc Nutr Food Sci 63:161–167
Yoshizaki T, Tada Y, Hida A, Sunami A, Yokoyama Y, Togo F, Kawano Y (2013) Influence of dietary behavior on the circadian rhythm of the autonomic nervous system as assessed by heart rate variability. Physiol Behav 118:122–128
Acknowledgments
We acknowledge the support of Manami Suzuki, Momoko Nishimura, and Kana Maeda in the Department of Nutritional Science, Faculty of Applied Biosciences, Tokyo University of Agriculture and the cooperation of study participants. This study was supported by a Grant-in-Aid for Research Fellowships of Japan Society for the Promotion of Science for Young Scientists.
Conflict of interest
The authors declare no conflicts of interest.
Ethical Standards
The experiments described herein comply with the current laws of Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Massimo Pagani.
Rights and permissions
About this article
Cite this article
Yoshizaki, T., Tada, Y., Hida, A. et al. Effects of feeding schedule changes on the circadian phase of the cardiac autonomic nervous system and serum lipid levels. Eur J Appl Physiol 113, 2603–2611 (2013). https://doi.org/10.1007/s00421-013-2702-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-013-2702-z