Abstract
Purpose
To examine (1) the retinal structure by optical coherence tomography (OCT) and function by means of multifocal electroretinography (mfERG) in eyes with and without nonproliferative diabetic retinopathy (NPDR) (2) for correspondence between local retinal function and OCT zones with retinal lesions.
Methods
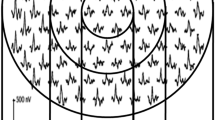
One hundred and thirty-two eligible participants (30 with nonproliferative DR (NPDR) and 102 with diabetes with no DR) underwent comprehensive ophthalmic examination, optical coherence tomography for retinal thickness measures, mfERG, and ultra-wide field fundus photography. OCT Early Treatment Diabetic Retinopathy Study (ETDRS) grid was overlaid on to mfERG plots.
Results
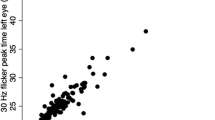
Those with NPDR had significantly thicker full retinal measures in the nine (ETDRS) zones compared to no DR. mfERG P1 latencies in rings 1–6 were significantly delayed, while the response densities in rings 4–6 were lower in the NPDR group. Significant negative correlation was noted between OCT thickness and mfERG P1 response densities in many ETDRS zones. Significant positive correlation was noted between P1 latencies and OCT thickness in a few zones. The combination of cystic spaces, microaneurysms, and hard exudates were present in all zones and were associated with a decrease in P1 response densities compared to no lesions. Reduced P1 response densities were associated with a sporadic delay in the mfERG latencies and vice versa. The number of lesions did not show correspondence to the mfERG measures.
Conclusions
In eyes with NPDR, retinal function is differentially correlated with the DR lesions on OCT and can be assessed using multimodal imaging modalities.




Similar content being viewed by others
Data availability
Data are contained within the article and are included in the form of a Microsoft excel sheet (supplementary material).
Code availability
Not applicable.
References
Barber AJ, Lieth E, Khin SA, Antonetti DA, Buchanan AG, Gardner TW (1998) Neural apoptosis in the retina during experimental and human diabetes. Early onset and effect of insulin. J Clin Invest 102:783–791. https://doi.org/10.1172/JCI2425
Bursell SE, Clermont AC, Kinsley BT, Simonson DC, Aiello LM, Wolpert HA (1996) Retinal blood flow changes in patients with insulin-dependent diabetes mellitus and no diabetic retinopathy. Invest Ophthalmol Vis Sci 37:886–897
Ghafour IM, Foulds WS, Allan D, McClure E (1982) Contrast sensitivity in diabetic subjects with and without retinopathy. Br J Ophthalmol 66:492–495. https://doi.org/10.1136/bjo.66.8.492
Hsiao C-C, Hsu H-M, Yang C-M, Yang C-H (2019) Correlation of retinal vascular perfusion density with dark adaptation in diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol 257:1401–1410. https://doi.org/10.1007/s00417-019-04321-2
Bearse MA, Sutter EE (1996) Imaging localized retinal dysfunction with the multifocal electroretinogram. JOSA A. 13:634–640. https://doi.org/10.1364/JOSAA.13.000634
Findl O, Dallinger S, Rami B, Polak K, Schober E, Wedrich A et al (2000) Ocular haemodynamics and colour contrast sensitivity in patients with type 1 diabetes. Br J Ophthalmol 84:493–498. https://doi.org/10.1136/bjo.84.5.493
Li T, Jia Y, Wang S, Wang A, Gao L, Yang C et al (2019) Retinal microvascular abnormalities in children with type 1 diabetes mellitus without visual impairment or diabetic retinopathy. Invest Ophthalmol Vis Sci 60:990–998. https://doi.org/10.1167/iovs.18-25499
Åkerblom H, Andreasson S, Holmström G (2016) Macular function in preterm children at school age. Doc Ophthalmol Adv Ophthalmol 133:151–157. https://doi.org/10.1007/s10633-016-9564-8
Holm K, Ponjavic V, Lövestam-Adrian M (2010) Using multifocal electroretinography hard exudates affect macular function in eyes with diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 248:1241–1247. https://doi.org/10.1007/s00417-010-1347-4
Bloodworth JMB (1962) Diabetic retinopathy. Diabetes 11:1–22
Waldstein SM, Wright J, Warburton J, Margaron P, Simader C, Schmidt-Erfurth U et al (2016) Predictive value of retinal morphology for visual acuity outcomes of different ranibizumab treatment regimens for neovascular AMD. Ophthalmol 123:60–69. https://doi.org/10.1016/j.ophtha.2015.09.013
Bhende M, Shetty S, Parthasarathy MK, Ramya S (2018) Optical coherence tomography: A guide to interpretation of common macular diseases. Indian J Ophthalmol 66:20–35. https://doi.org/10.4103/ijo.IJO_902_17
Li X, Xie J, Zhang L, Cui Y, Zhang G, Wang J, Zhang A, Chen X, Huang T, Meng Q (2020) Differential distribution of manifest lesions in diabetic retinopathy by fundus fluorescein angiography and fundus photography. BMC Ophthalmol 120:471. https://doi.org/10.1186/s12886-020-01740-2
Jensen SP, Jeppesen P, Bek T (2011) Differential diameter responses in macular and peripheral retinal arterioles may contribute to the regional distribution of diabetic retinopathy lesions. Graefes Arch Clin Exp Ophthalmol 249:407–412. https://doi.org/10.1007/s00417-010-1549-9
Goebel W, Kretzchmar-Gross T (2002) Retinal thickness in diabetic retinopathy: a study using optical coherence tomography (OCT). Retina Phila Pa 22:759–767. https://doi.org/10.1097/00006982-200212000-00012
Oshima Y, Emi K, Yamanishi S, Motokura M (1999) Quantitative assessment of macular thickness in normal subjects and patients with diabetic retinopathy by scanning retinal thickness analyser. Br J Ophthalmol 83:54–61. https://doi.org/10.1136/bjo.83.1.54
Lattanzio R, Brancato R, Pierro L, Bandello F, Iaccher B, Fiore T et al (2002) Macular thickness measured by optical coherence tomography (OCT) in diabetic patients. Eur J Ophthalmol 12:482–487. https://doi.org/10.1177/112067210201200606
Massin P, Erginay A, Haouchine B, Mehidi AB, Paques M, Gaudric A (2002) Retinal thickness in healthy and diabetic subjects measured using optical coherence tomography mapping software. Eur J Ophthalmol 12:102–108. https://doi.org/10.1177/112067210201200205
Cunha-Vaz J, Ribeiro L, Nunes S, Lobo C. Biomarkers of diabetic retinopathy Review. In 2014. https://doi.org/10.1900/RDS.2015.12.159
Simó R, Stitt AW, Gardner TW (2018) Neurodegeneration in diabetic retinopathy: does it really matter? Diabetologia 61:1902–1912. https://doi.org/10.1007/s00125-018-4692-1
Joussen AM, Poulaki V, Le ML, Koizumi K, Esser C, Janicki H, Schraermeyer U, Kociok N, Fauser S, Kirchhof B, Kern TS, Adamis AP (2004) A central role for inflammation in the pathogenesis of diabetic retinopathy. FASEB J 18:1450–1452. https://doi.org/10.1096/fj.03-1476fje
Hafner J, Karst S, Schmidt-Erfurth U (2017) Potential imaging biomarkers in the development and progression of diabetic retinopathy. Early Events Diabet Retin Interv Strateg [Internet]. Dec 20 [cited 2019 Aug 13]; Available from: https://www.intechopen.com/books/early-events-in-diabetic-retinopathy-and-intervention-strategies/potential-imaging-biomarkers-in-the-development-and-progression-of-diabetic-retinopathy. https://doi.org/10.5772/intechopen.71747
Chua J, Sim R, Tan B, Wong D, Yao X, Liu X, Ting DSW, Schmidl D, Ang M, Garhöfer G, Schmetterer L (2020) Optical coherence tomography angiography in diabetes and diabetic retinopathy. J Clin Med 9:1723. https://doi.org/10.3390/jcm9061723
Dimitrova G, Chihara E, Takahashi H, Amano H, Okazaki K (2017) Quantitative retinal optical coherence tomography angiography in patients with diabetes without diabetic retinopathy. Invest Ophthalmol Vis Sci 58:190–196. https://doi.org/10.1167/iovs.16-20531
Arima M, Nakao S, Kaizu Y, et al (2021) Diabetic vascular hyperpermeability: optical coherence tomography angiography and functional loss assessments of relationships among retinal vasculature changes [published correction appears in Sci Rep. Jun 7;11(1):12344]. Sci Rep. 2021;11:4185. Published 2021 Feb 18. https://doi.org/10.1038/s41598-021-83334-6
Das A, McGuire PG, Rangasamy S (2015) Diabetic macular edema: Pathophysiology and novel therapeutic targets. Ophthalmology 122:1375–1394. https://doi.org/10.1016/j.ophtha.2015.03.024
Cunha-Vaz J (2021) A central role for ischemia and OCTA metrics to follow DR progression. J Clin Med 10:1821. https://doi.org/10.3390/jcm10091821
Browning DJ, Apte RS, Bressler SB, Chalam KV, Danis RP, Davis MD, Kollman C, Qin H, Sadda S, Scott IU, Diabetic Retinopathy Clinical Research Network (2009) Association of the extent of diabetic macular edema as assessed by optical coherence tomography with visual acuity and retinal outcome variables. Retina 29:300–305. https://doi.org/10.1097/IAE.0b013e318194995d
Tzekov R, Arden GB (1999) The electroretinogram in diabetic retinopathy. Surv Ophthalmol 44:53–60. https://doi.org/10.1016/s0039-6257(99)00063-6
Yamamoto S, Kamiyama M, Nitta K, Yamada T, Hayasaka S (1996) Selective reduction of the S cone electroretinogram in diabetes. Br J Ophthalmol 80:973–975. https://doi.org/10.1136/bjo.80.11.973
Luu CD, Szental JA, Lee SY, Lavanya R, Wong TY (2010) Correlation between retinal oscillatory potentials and retinal vascular caliber in type 2 diabetes. Invest Ophthalmol Vis Sci 51:482–486. https://doi.org/10.1167/iovs.09-4069
Hammer M, Heller T, Jentsch S, Dawczynski J, Schweitzer D, Peters S, Schmidtke KU, Müller UA (2012) Retinal vessel oxygen saturation under flicker light stimulation in patients with nonproliferative diabetic retinopathy. Invest Ophthalmol Vis Sci 53:4063–4068. https://doi.org/10.1167/iovs.12-9659
Mandecka A, Dawczynski J, Blum M, Müller N, Kloos C, Wolf G, Vilser W, Hoyer H, Müller UA (2007) Influence of flickering light on the retinal vessels in diabetic patients. Diabetes Care 30:3048–3052. https://doi.org/10.2337/dc07-0927
Hood DC (2000) Assessing retinal function with the multifocal technique. Prog Retin Eye Res 19:607–646. https://doi.org/10.1016/S1350-9462(00)00013-6
Hood DC, Frishman LJ, Saszik S, Viswanathan S (2002) Retinal origins of the primate multifocal ERG: implications for the human response. Invest Ophthalmol Vis Sci 43:1673–1685
Yip YWY, Ngai JWS, Fok ACT, Lai RYK, Li H, Lam DSC et al (2010) Correlation between functional and anatomical assessments by multifocal electroretinography and optical coherence tomography in central serous chorioretinopathy. Doc Ophthalmol Adv Ophthalmol 120:193–200. https://doi.org/10.1007/s10633-010-9213-6
Santos AR, Ribeiro L, Bandello F, Lattanzio R, Egan C, Frydkjaer-Olsen U et al (2017) Functional and structural findings of neurodegeneration in early stages of diabetic retinopathy: cross-sectional analyses of baseline data of the EUROCONDOR Project. Diabetes 66:2503–2510. https://doi.org/10.2337/db16-1453
Bearse MA, Adams AJ, Han Y, Schneck ME, Ng J, Bronson-Castain K et al (2006) A multifocal electroretinogram model predicting the development of diabetic retinopathy. Prog Retin Eye Res 25:425–448. https://doi.org/10.1016/j.preteyeres.2006.07.001
Whatham AR, Nguyen V, Zhu Y, Hennessy M, Kalloniatis M (2014) The value of clinical electrophysiology in the assessment of the eye and visual system in the era of advanced imaging. Clin Exp Optom 97:99–115. https://doi.org/10.1111/cxo.12085
Funding
This work was supported by the Wellcome Trust/DBT India Alliance Early Career Fellowship [grant number IA/CPHE/16/1/502670] awarded to Dr Sangeetha Srinivasan.
Author information
Authors and Affiliations
Contributions
SS, RRN, and MPB contributed to the study concepts and study design and obtained funding and patient examination; SS, RRN, MPB, and GM were responsible for data acquisition; SS and GM were responsible for data analysis; SS was responsible for statistical analysis; SS and MPB were responsible for manuscript preparation and editing. All authors critically reviewed the manuscript. SS and MPB act as guarantors.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board was approved by the Ethics Committee of Vision Research Foundation [Approval no: 642–2017-P, date of approval: 11.1.2018], Chennai, India.
Consent to participate
Participants provided written informed consent.
Consent for publication
All authors are in agreement with the content of the manuscript.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Srinivasan, S., Sivaprasad, S., Munusamy, G. et al. Zone-wise examination of optical coherence tomography features and their correspondence to multifocal electroretinography in eyes with nonproliferative diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 260, 827–837 (2022). https://doi.org/10.1007/s00417-021-05446-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05446-z