Abstract
Purpose
Persistent metamorphopsia, particularly aniseikonia, is a troublesome problem which may occur after epiretinal membrane (ERM) surgery. To clarify if the preoperative foveal avascular zone (FAZ) morphology can be used as a predictor of postoperative residual aniseikonia, the morphological changes in the FAZ and the degree of aniseikonia between before and 12 months after vitrectomy for epiretinal membrane (ERM) were measured and analyzed.
Methods
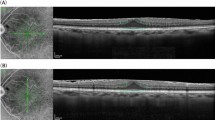
Thirty patients, each with a unilateral idiopathic ERM, who underwent treatment between September 2016 and March 2017 were enrolled for this prospective case series study. Best-corrected visual acuity (BCVA), the degree of aniseikonia, central foveal thickness (CFT), FAZ area (FAZa), perimeter (FAZp), and circularity in ERM eyes were examined before and 1, 3, 6 and 12 months after surgery. The fellow eye without an ERM was also examined and used as the control. The interocular ratios of the CFT, FAZa, and FAZp in ERM eyes with those in control eyes were also calculated. Multiple regression analysis was performed on preoperative parameters that were found to be significantly correlated with the 12-month aniseikonia in univariate analyses.
Results
The BCVA in the ERM eyes was significantly improved at 1 month after surgery (P < .0001) The degree of aniseikonia was significantly reduced only after 12 months (P = .004). The CFT had decreased significantly by 3 months after the surgery and continued decreasing thereafter (P < .0001). Both FAZa and FAZp were significantly smaller in the ERM eyes than in the control eyes throughout the study period (P < .0001 and P < .0001, respectively), with no change in either parameter over the study period. Correlation analyses revealed that the degree of aniseikonia was significantly correlated with pre- and postoperative CFT, CFT ratio, FAZa, FAZa ratio, FAZp, and FAZp ratio. Within preoperative OCT parameters, FAZa ratio remained significant after multiple regression analysis was performed (P < .0001).
Conclusions
Aniseikonia changed little over the long term following ERM surgery. Preoperative FAZ area ratio was identified as a significant predictor of postoperative aniseikonia.



Similar content being viewed by others
References
Rahman R, Stephenson J (2014) Early surgery for epiretinal membrane preserves more vision for patients. Eye (Lond) 28:410–414. https://doi.org/10.1038/eye.2013.305
Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T (2014) Time course of changes in aniseikonia and foveal microstructure after vitrectomy for epiretinal membrane. Ophthalmology 121:2255–2260. https://doi.org/10.1016/j.ophtha.2014.05.016
Chung H, Son G, Hwang DJ, Lee K, Park Y, Sohn J (2015) Relationship between vertical and horizontal aniseikonia scores and vertical and horizontal OCT images in idiopathic epiretinal membrane. Invest Ophthalmol Vis Sci 56:6542–6548. https://doi.org/10.1167/iovs.15-16874
Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T (2017) Aniseikonia in various retinal disorders. Graefes Arch Clin Exp Ophthalmol 255:1063–1071. https://doi.org/10.1007/s00417-017-3597-x
Takabatake M, Higashide T, Udagawa S, Sugiyama K (2017) Postoperative changes and prognostic factors of visual acuity, metamorphopsia, and aniseikonia after vitrectomy for epiretinal membrane. Retina 38:2118–2127. https://doi.org/10.1097/IAE.0000000000001831
Arimura E, Matsumoto C, Okuyama S, Takada S, Hashimoto S, Shimomura Y (2005) Retinal contraction and metamorphopsia scores in eyes with idiopathic epiretinal membrane. Invest Ophthalmol Vis Sci 46:2961–2966. https://doi.org/10.1167/iovs.04-1104
Smiddy WE, Maguire AM, Green WR, Michels RG, de la Cruz Z, Enger C, Jaeger M, Rice TA (1989) Idiopathic epiretinal membranes. Ultrastructural characteristics and clinicopathologic correlation. Ophthalmology 96:811–820 discussion 821
Bu SC, Kuijer R, Li XR, Hooymans JM, Los LI (2014) Idiopathic epiretinal membrane. Retina 34:2317–2335. https://doi.org/10.1097/IAE.0000000000000349
Spaide RF, Fujimoto JG, Waheed NK, Sadda SR, Staurenghi G (2018) Optical coherence tomography angiography. Prog Retin Eye Res 64:1–55. https://doi.org/10.1016/j.preteyeres.2017.11.003
Shiihara H, Terasaki H, Sonoda S, Kakiuchi N, Shinohara Y, Tomita M, Sakamoto T (2018) Objective evaluation of size and shape of superficial foveal avascular zone in normal subjects by optical coherence tomography angiography. Sci Rep 8:10143. https://doi.org/10.1038/s41598-018-28530-7
Kitagawa Y, Shimada H, Shinojima A, Nakashizuka H (2017) Foveal avascular zone area analysis using optical coherence tomography angiography before and after idiopathic epiretinal membrane surgery. Retina. https://doi.org/10.1097/IAE.0000000000001972
Kim JH, Kang SW, Kong MG, Ha HS (2013) Assessment of retinal layers and visual rehabilitation after epiretinal membrane removal. Graefes Arch Clin Exp Ophthalmol 251:1055–1064. https://doi.org/10.1007/s00417-012-2120-7
Han J, Han SH, Kim JH, Koh HJ (2016) Restoration of retinally induced aniseikonia in patients with epiretinal membrane after early vitrectomy. Retina 36:311–320. https://doi.org/10.1097/IAE.0000000000000731
Watanabe A, Arimoto S, Nishi O (2009) Correlation between metamorphopsia and epiretinal membrane optical coherence tomography findings. Ophthalmology 116:1788–1793. https://doi.org/10.1016/j.ophtha.2009.04.046
Lim JW (2011) Results of spectral-domain optical coherence tomography by preferential hyperacuity perimeter in patients after idiopathic epiretinal membrane surgery. Curr Eye Res 36:364–369. https://doi.org/10.3109/02713683.2010.545499
Franze K, Grosche J, Skatchkov SN, Schinkinger S, Foja C, Schild D, Uckermann O, Travis K, Reichenbach A, Guck J (2007) Muller cells are living optical fibers in the vertebrate retina. Proc Natl Acad Sci U S A 104:8287–8292. https://doi.org/10.1073/pnas.0611180104
Reichenbach A, Bringmann A (2013) New functions of Muller cells. Glia 61:651–678. https://doi.org/10.1002/glia.22477
Colakoglu A, Balci Akar S (2017) Potential role of Muller cells in the pathogenesis of macropsia associated with epiretinal membrane: a hypothesis revisited. Int J Ophthalmol 10:1759–1767. https://doi.org/10.18240/ijo.2017.11.19
Fingler J, Readhead C, Schwartz DM, Fraser SE (2008) Phase-contrast OCT imaging of transverse flows in the mouse retina and choroid. Invest Ophthalmol Vis Sci 49:5055–5059. https://doi.org/10.1167/iovs.07-1627
Fingler J, Schwartz D, Yang C, Fraser SE (2007) Mobility and transverse flow visualization using phase variance contrast with spectral domain optical coherence tomography. Opt Express 15:12636–12653
Fingler J, Zawadzki RJ, Werner JS, Schwartz D, Fraser SE (2009) Volumetric microvascular imaging of human retina using optical coherence tomography with a novel motion contrast technique. Opt Express 17:22190–22200. https://doi.org/10.1364/OE.17.022190
Kim DY, Fingler J, Werner JS, Schwartz DM, Fraser SE, Zawadzki RJ (2011) In vivo volumetric imaging of human retinal circulation with phase-variance optical coherence tomography. Biomed Opt Express 2:1504–1513. https://doi.org/10.1364/BOE.2.001504
Kim DY, Fingler J, Zawadzki RJ, Park SS, Morse LS, Schwartz DM, Fraser SE, Werner JS (2012) Noninvasive imaging of the foveal avascular zone with high-speed, phase-variance optical coherence tomography. Invest Ophthalmol Vis Sci 53:85–92. https://doi.org/10.1167/iovs.11-8249
Mahmud MS, Cadotte DW, Vuong B, Sun C, Luk TW, Mariampillai A, Yang VX (2013) Review of speckle and phase variance optical coherence tomography to visualize microvascular networks. J Biomed Opt 18:50901. https://doi.org/10.1117/1.JBO.18.5.050901
Tan CS, Lim LW, Chow VS, Chay IW, Tan S, Cheong KX, Tan GT, Sadda SR (2016) Optical coherence tomography angiography evaluation of the parafoveal vasculature and its relationship with ocular factors. Invest Ophthalmol Vis Sci 57:OCT224–OCT234. https://doi.org/10.1167/iovs.15-18869
Liu G, Keyal K, Wang F (2017) Interocular symmetry of vascular density and association with central macular thickness of healthy adults by optical coherence tomography angiography. Sci Rep 7:16297. https://doi.org/10.1038/s41598-017-16675-w
Ghassemi F, Mirshahi R, Bazvand F, Fadakar K, Faghihi H, Sabour S (2017) The quantitative measurements of foveal avascular zone using optical coherence tomography angiography in normal volunteers. J Curr Ophthalmol 29:293–299. https://doi.org/10.1016/j.joco.2017.06.004
Azuma K, Ueta T, Eguchi S, Aihara M (2017) Effects of internal limiting membrane peeling combined with removal of idiopathic epiretinal membrane: a systematic review of literature and meta-analysis. Retina 37:1813–1819. https://doi.org/10.1097/IAE.0000000000001537
Chang WC, Lin C, Lee CH, Sung TL, Tung TH, Liu JH (2017) Vitrectomy with or without internal limiting membrane peeling for idiopathic epiretinal membrane: a meta-analysis. PLoS One 12:e0179105. https://doi.org/10.1371/journal.pone.0179105
De Novelli FJ, Goldbaum M, Monteiro MLR, Bom Aggio F, Takahashi WY (2017) Surgical removal of epiretinal membrane with and without removal of internal limiting membrane: comparative study of visual acuity, features of optical coherence tomography, and recurrence rate. Retina. https://doi.org/10.1097/IAE.0000000000001983
Diaz-Valverde A, Wu L (2018) To peel or not to peel the internal limiting membrane in idiopathic epiretinal membranes. Retina 38(Suppl 1):S5–S11. https://doi.org/10.1097/IAE.0000000000001906
Obata S, Fujikawa M, Iwasaki K, Kakinoki M, Sawada O, Saishin Y, Kawamura H, Ohji M (2017) Changes in retinal thickness after vitrectomy for epiretinal membrane with and without internal limiting membrane peeling. Ophthalmic Res 57:135–140. https://doi.org/10.1159/000448956
Sultan H, Wykoff CC, Shah AR (2018) Five-year outcomes of surgically treated symptomatic epiretinal membranes with and without internal limiting membrane peeling. Ophthalmic Surg Lasers Imaging Retina 49:296–302. https://doi.org/10.3928/23258160-20180501-02
Lee JW, Kim IT (2010) Outcomes of idiopathic macular epiretinal membrane removal with and without internal limiting membrane peeling: a comparative study. Jpn J Ophthalmol 54:129–134. https://doi.org/10.1007/s10384-009-0778-0
Hirata A, Murata K, Hayashi K, Nakamura KI (2018) Three-dimensional analysis of peeled internal limiting membrane using focused ion beam/scanning electron microscopy. Transl Vis Sci Technol 7:15. https://doi.org/10.1167/tvst.7.1.15
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Hayashi Eye Hospital institutional review committee and with the 1964 Helsinki declaration.
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hirata, A., Nakada, H., Mine, K. et al. Relationship between the morphology of the foveal avascular zone and the degree of aniseikonia before and after vitrectomy in patients with unilateral epiretinal membrane. Graefes Arch Clin Exp Ophthalmol 257, 507–515 (2019). https://doi.org/10.1007/s00417-019-04245-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04245-x