Abstract
Background and purpose
Antiphospholipid syndrome (APS) is one of the uncommon causes of ischemic stroke, and is associated with young and female patients. However, the significance of antiphospholipid antibody (aPL) in older ischemic stroke patients is uncertain. We aimed to examine the significance of aPLs in ischemic stroke in these older patients.
Materials and methods
A total of 739 patients with acute ischemic stroke within 7 days of initial symptoms were collected consecutively. Clinical and laboratory data were obtained from medical records. aPLs (lupus anticoagulant, anti-cardiolipin antibody, anti-β2glycoprotein-I antibody) were measured the day after admission and the presence of at least one antibody was regarded as positive aPL. Patients with positive aPL were rechecked after at least 12 weeks for confirmation of APS.
Result
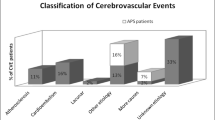
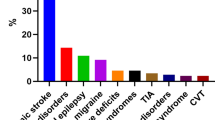
Of the 739 patients, 103 (13.9%) had at least one aPL initially. These patients were older, had more atrial fibrillation and higher levels of inflammatory markers. Among the 103 aPL positive patients, 41 remained positive at 3 months, 23 showed negative conversion, and 39 were not available for follow-up. Patients diagnosed with APS had higher numbers of aPL and had specifically anti-β2glycoprotein-I IgG antibody. The patients with aPLs did not differ significantly from the others in terms of stroke subtype.
Conclusion
aPL was rather common in ischemic stroke patients regardless of age. Although the influence of transient positive aPL on ischemic stroke remains uncertain, two or more aPLs and the presence of anti-β2glycoprotein-I IgG may predict a diagnosis of APS.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, DerksenDeg RHPG, Koike T, Meroni PL, Reber G, Shoenfeld Y, Tincani A, Vlachoyiannopoulos PG, Krilis SA (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4(2):295–306. https://doi.org/10.1111/j.1538-7836.2006.01753.x
Garcia D, Erkan D (2018) Diagnosis and management of the antiphospholipid syndrome. N Engl J Med 378(21):2010–2021. https://doi.org/10.1056/NEJMra1705454
Svenungsson E, Antovic A (2020) The antiphospholipid syndrome: often overlooked cause of vascular occlusions? J Intern Med 287(4):349–372. https://doi.org/10.1111/joim.13022
Cervera R, Piette JC, Font J, Khamashta MA, Shoenfeld Y, Camps MT, Jacobsen S, Lakos G, Tincani A, Kontopoulou-Griva I, Galeazzi M, Meroni PL, Derksen RH, de Groot PG, Gromnica-Ihle E, Baleva M, Mosca M, Bombardieri S, Houssiau F, Gris JC, Quere I, Hachulla E, Vasconcelos C, Roch B, Fernandez-Nebro A, Boffa MC, Hughes GR, Ingelmo M, Euro-Phospholipid Project G (2002) Antiphospholipid syndrome: clinical and immunologic manifestations and patterns of disease expression in a cohort of 1000 patients. Arthritis Rheum 46(4):1019–1027. https://doi.org/10.1002/art.10187
Muscal E, Brey RL (2008) Neurologic manifestations of the antiphospholipid syndrome: integrating molecular and clinical lessons. Curr Rheumatol Rep 10(1):67–73. https://doi.org/10.1007/s11926-008-0012-y
Urbanus RT, Siegerink B, Roest M, Rosendaal FR, de Groot PG, Algra A (2009) Antiphospholipid antibodies and risk of myocardial infarction and ischaemic stroke in young women in the RATIO study: a case-control study. Lancet Neurol 8(11):998–1005. https://doi.org/10.1016/S1474-4422(09)70239-X
Anticardiolipin antibodies are an independent risk factor for first ischemic stroke. The Antiphospholipid Antibodies in Stroke Study (APASS) Group (1993). Neurology 43 (10):2069–2073. https://doi.org/10.1212/wnl.43.10.2069
Carmel-Neiderman NN, Tanne D, Goren I, Rotman-Pikielny P, Levy Y (2017) Classical and additional antiphospholipid antibodies in blood samples of ischemic stroke patients and healthy controls. Immunol Res 65(2):470–476. https://doi.org/10.1007/s12026-017-8897-z
Levine SR, Brey RL, Tilley BC, Thompson JL, Sacco RL, Sciacca RR, Murphy A, Lu Y, Costigan TM, Rhine C, Levin B, Triplett DA, Mohr JP, Investigators A (2004) Antiphospholipid antibodies and subsequent thrombo-occlusive events in patients with ischemic stroke. JAMA 291(5):576–584. https://doi.org/10.1001/jama.291.5.576
Brey RL, Abbott RD, Curb JD, Sharp DS, Ross GW, Stallworth CL, Kittner SJ (2001) beta(2)-Glycoprotein 1-dependent anticardiolipin antibodies and risk of ischemic stroke and myocardial infarction: the honolulu heart program. Stroke 32(8):1701–1706. https://doi.org/10.1161/01.str.32.8.1701
Rodriguez-Sanz A, Martinez-Sanchez P, Prefasi D, Fuentes B, Pascual-Salcedo D, Blanco-Banares MJ, Diez-Tejedor E (2015) Antiphospholipid antibodies correlate with stroke severity and outcome in patients with antiphospholipid syndrome. Autoimmunity 48(5):275–281. https://doi.org/10.3109/08916934.2014.988329
Andreoli L, Chighizola CB, Banzato A, Pons-Estel GJ, Ramire de Jesus G, Erkan D (2013) Estimated frequency of antiphospholipid antibodies in patients with pregnancy morbidity, stroke, myocardial infarction, and deep vein thrombosis: a critical review of the literature. Arthritis Care Res (Hoboken) 65(11):1869–1873. https://doi.org/10.1002/acr.22066
Sciascia S, Sanna G, Khamashta MA, Cuadrado MJ, Erkan D, Andreoli L, Bertolaccini ML, Action APS (2015) The estimated frequency of antiphospholipid antibodies in young adults with cerebrovascular events: a systematic review. Ann Rheum Dis 74(11):2028–2033. https://doi.org/10.1136/annrheumdis-2014-205663
Shoenfeld Y, Twig G, Katz U, Sherer Y (2008) Autoantibody explosion in antiphospholipid syndrome. J Autoimmun 30(1–2):74–83. https://doi.org/10.1016/j.jaut.2007.11.011
Belizna C, Lartigue A, Favre J, Gilbert D, Tron F, Levesque H, Thuillez C, Richard V (2008) Antiphospholipid antibodies induce vascular functional changes in mice: a mechanism of vascular lesions in antiphospholipid syndrome? Lupus 17(3):185–194. https://doi.org/10.1177/0961203307086931
de Groot PG, Derksen RH (2005) Pathophysiology of the antiphospholipid syndrome. J Thromb Haemost 3(8):1854–1860. https://doi.org/10.1111/j.1538-7836.2005.01359.x
Islam MA, Alam F, Sasongko TH, Gan SH (2016) Antiphospholipid antibody-mediated thrombotic mechanisms in antiphospholipid syndrome: towards pathophysiology-based treatment. Curr Pharm Des 22(28):4451–4469. https://doi.org/10.2174/1381612822666160527160029
Rand JH (2002) Molecular pathogenesis of the antiphospholipid syndrome. Circ Res 90(1):29–37. https://doi.org/10.1161/hh0102.102795
Willis R, Pierangeli SS (2011) Pathophysiology of the antiphospholipid antibody syndrome. Auto Immun Highlights 2(2):35–52. https://doi.org/10.1007/s13317-011-0017-9
Haviv YS (2000) Association of anticardiolipin antibodies with vascular injury: possible mechanisms. Postgrad Med J 76(900):625–628. https://doi.org/10.1136/pmj.76.900.625
Petri M (2000) Epidemiology of the antiphospholipid antibody syndrome. J Autoimmun 15(2):145–151. https://doi.org/10.1006/jaut.2000.0409
Juby AG, Davis P (1998) Prevalence and disease associations of certain autoantibodies in elderly patients. Clin Invest Med 21(1):4–11
Arboix A, Bechich S, Oliveres M, García-Eroles L, Massons J, Targa C (2001) Ischemic stroke of unusual cause: clinical features, etiology and outcome. Eur J Neurol 8(2):133–139
Arboix A, Cartanyà A, Lowak M, García-Eroles L, Parra O, Oliveres M, Massons J (2014) Gender differences and woman-specific trends in acute stroke: results from a hospital-based registry (1986–2009). Clin Neurol Neurosurg 127:19–24
Binder SR, Litwin CM (2017) Anti-phospholipid antibodies and smoking: an overview. Clin Rev Allergy Immunol 53(1):1–13
Aune D, Schlesinger S, Norat T, Riboli E (2018) Tobacco smoking and the risk of atrial fibrillation: a systematic review and meta-analysis of prospective studies. Eur J Prevent Cardiol 25(13):1437–1451
Radic M, Pattanaik D (2018) Cellular and molecular mechanisms of anti-phospholipid syndrome. Front Immunol 9:969. https://doi.org/10.3389/fimmu.2018.00969
Mehdi AA, Salti I, Uthman I (2011) Antiphospholipid syndrome: endocrinologic manifestations and organ involvement. Semin Thromb Hemost 37(1):49–57. https://doi.org/10.1055/s-0030-1270071
Iwaniec T, Kaczor MP, Celinska-Lowenhoff M, Polanski S, Musial J (2016) Identification of patients with triple antiphospholipid antibody positivity is platform and method independent. Pol Arch Med Wewn 126(1–2):19–24. https://doi.org/10.20452/pamw.3259
Pengo V, Ruffatti A, Del Ross T, Tonello M, Cuffaro S, Hoxha A, Banzato A, Bison E, Denas G, Bracco A, Padayattil Jose S (2013) Confirmation of initial antiphospholipid antibody positivity depends on the antiphospholipid antibody profile. J Thromb Haemost 11(8):1527–1531. https://doi.org/10.1111/jth.12264
Marquez Gomez J, Araujo Loperena O, Hernandez Toboso S (2017) Transient antiphospholipid syndrome and splenic infarction in a patient with parvovirus B19 acute infection. Med Clin (Barc) 149(9):419–420. https://doi.org/10.1016/j.medcli.2017.05.005
Nakayama T, Akahoshi M, Irino K, Kimoto Y, Arinobu Y, Niiro H, Tsukamoto H, Horiuchi T, Akashi K (2014) Transient antiphospholipid syndrome associated with primary cytomegalovirus infection: a case report and literature review. Case Rep Rheumatol 2014:271548. https://doi.org/10.1155/2014/271548
Battistelli S, Stefanoni M, Petrioli R, Genovese A, Dell’avanzato R, Donati G, Vittoria A, Roviello F (2008) Antiphospholipid antibodies and acute-phase response in non-metastatic colorectal cancer patients. Int J Biol Markers 23(1):31–35
Funding
This work was supported by the research fund of Hanyang University (HY-202000000003328).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there are no conflicts of interest relevant to this work.
Ethical standard statement
This study was approved by the Institutional Review Board of Hanyang University Hospital (HYUH 2019-12-022).
Rights and permissions
About this article
Cite this article
Yoo, J.S., Kim, Y.S., Kim, H.Y. et al. Comparison of patients with transient and sustained increments of antiphospholipid antibodies after acute ischemic stroke. J Neurol 268, 2541–2549 (2021). https://doi.org/10.1007/s00415-021-10432-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10432-w