Abstract
Objective
To analyze deep brain stimulation (DBS) outcomes in patients with cervical dystonia (CD), the relationships between motor and disability/pain outcomes, and the differences in outcomes between globus pallidus internus (GPi) and subthalamic nucleus (STN) DBS, and to identify potential outcome predictors.
Methods
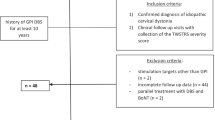
A systematic literature search identified individual patient data of CD patients who underwent DBS and whose outcomes were assessed with the Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS). Then, we performed a pooled meta-analysis on this cohort.
Results
A review of 39 papers yielded 208 patients with individual TWSTRS scores and demographic information. At a mean follow-up period of 23.3 months after either GPi or STN DBS, the TWSTRS total (58.8%), severity (53.9%), disability (61.3%), and pain (46.6%) scores significantly improved compared to baseline status (all p < 0.001). There were no significant outcome differences between short-term (< 23.3 months) and long-term (≥ 23.3 months). The TWSTRS outcomes after GPi and STN DBS were comparable, whereas these two targets showed different adverse effect profiles. The rates of responders to DBS according to the TWSTRS total and severity (defined as ≥ 25% improvement) were both 89%. Regression analyses demonstrated motor benefits associated with disability improvement more than pain relief (R2 = 0.345 and 0.195, respectively). No clinically meaningful predictors for DBS outcomes were identified.
Conclusion
DBS improves motor symptoms, disability, and pain in CD patients and may provide sustained benefits over 2 years. GPi and STN appear to be equally effective targets with different adverse effect profiles.


Similar content being viewed by others
References
Patel S, Martino D (2013) Cervical dystonia: from pathophysiology to pharmacotherapy. Behav Neurol 26:275–282. https://doi.org/10.3233/BEN-2012-120270
Stamelou M, Edwards MJ, Hallett M, Bhatia KP (2012) The non-motor syndrome of primary dystonia: clinical and pathophysiological implications. Brain 135:1668–1681. https://doi.org/10.1093/brain/awr224
Skogseid IM, Kerty E (2005) The course of cervical dystonia and patient satisfaction with long-term botulinum toxin A treatment. Eur J Neurol 12:163–170. https://doi.org/10.1111/j.1468-1331.2004.01053.x
Volkmann J, Mueller J, Deuschl G et al (2014) Pallidal neurostimulation in patients with medication-refractory cervical dystonia: a randomised, sham-controlled trial. Lancet Neurol 13:875–884. https://doi.org/10.1016/S1474-4422(14)70143-7
Kiss ZH, Doig-Beyaert K, Eliasziw M et al (2007) The Canadian multicentre study of deep brain stimulation for cervical dystonia. Brain 130:2879–2886. https://doi.org/10.1093/brain/awm229
Skogseid IM, Ramm-Pettersen J, Volkmann J et al (2012) Good long-term efficacy of pallidal stimulation in cervical dystonia: a prospective, observer-blinded study. Eur J Neurol 19:610–615. https://doi.org/10.1111/j.1468-1331.2011.03591.x
Ostrem JL, Racine CA, Glass GA et al (2011) Subthalamic nucleus deep brain stimulation in primary cervical dystonia. Neurology 76:870–878. https://doi.org/10.1212/WNL.0b013e31820f2e4f
Walsh RA, Sidiropoulos C, Lozano AM et al (2013) Bilateral pallidal stimulation in cervical dystonia: blinded evidence of benefit beyond 5 years. Brain 136:761–769. https://doi.org/10.1093/brain/awt009
Yamada K, Hamasaki T, Hasegawa Y, Kuratsu J (2013) Long disease duration interferes with therapeutic effect of globus pallidus internus pallidal stimulation in primary cervical dystonia. Neuromodulation 16:219–225. https://doi.org/10.1111/j.1525-1403.2012.00464.x
Tsuboi T, Wong JK, Okun MS, Ramirez-Zamora A (2019) Quality of life outcomes after deep brain stimulation in dystonia: a systematic review. Parkinsonism Relat Disord. https://doi.org/10.1016/j.parkreldis.2019.11.016(Epub ahead of print)
Witt JL, Moro E, Ash RS et al (2013) Predictive factors of outcome in primary cervical dystonia following pallidal deep brain stimulation. Mov Disord 28:1451–1455. https://doi.org/10.1002/mds.25560
Ravindran K, Ganesh Kumar N, Englot DJ et al (2019) Deep brain stimulation versus peripheral denervation for cervical dystonia: a systematic review and meta-analysis. World Neurosurg 122:e940–e946. https://doi.org/10.1016/j.wneu.2018.10.178
Albanese A, Bhatia K, Bressman SB et al (2013) Phenomenology and classification of dystonia: a consensus update. Mov Disord 28:863–873. https://doi.org/10.1002/mds.25475
Comella CL, Stebbins GT, Goetz CG et al (1997) Teaching tape for the motor section of the Toronto Western Spasmodic Torticollis Scale. Mov Disord 12:570–575. https://doi.org/10.1002/mds.870120414
Ostrem JL, San Luciano M, Dodenhoff KA et al (2017) Subthalamic nucleus deep brain stimulation in isolated dystonia: a 3-year follow-up study. Neurology 88:25–35. https://doi.org/10.1212/WNL.0000000000003451
Misra VP, Ehler E, Zakine B et al (2012) Factors influencing response to Botulinum toxin type A in patients with idiopathic cervical dystonia: results from an international observational study. BMJ Open. https://doi.org/10.1136/bmjopen-2012-000881
Andaluz N, Taha JM, Dalvi A (2001) Bilateral pallidal deep brain stimulation for cervical and truncal dystonia. Neurology 57:557–558. https://doi.org/10.1212/wnl.57.3.557
Berman BD, Starr PA, Marks WJ, Ostrem JL (2009) Induction of bradykinesia with pallidal deep brain stimulation in patients with cranial-cervical dystonia. Stereotact Funct Neurosurg 87:37–44. https://doi.org/10.1159/000195718
Boček V, Štětkářová I, Fečíková A et al (2016) Pallidal stimulation in dystonia affects cortical but not spinal inhibitory mechanisms. J Neurol Sci 369:19–26. https://doi.org/10.1016/j.jns.2016.07.053
Cacciola F, Farah JO, Eldridge PR et al (2010) Bilateral deep brain stimulation for cervical dystonia: long-term outcome in a series of 10 patients. Neurosurgery 67:957–963. https://doi.org/10.1227/NEU.0b013e3181ec49c7
Calheiros-Trigo F, Linhares P (2014) Evaluation of the efficacy of deep brain stimulation in the surgical treatment of cervical dystonia. Neurocirugia (Astur) 25:49–55. https://doi.org/10.1016/j.neucir.2013.10.004
Dinkelbach L, Mueller J, Poewe W et al (2015) Cognitive outcome of pallidal deep brain stimulation for primary cervical dystonia: one year follow up results of a prospective multicenter trial. Park Relat Disord 21:976–980. https://doi.org/10.1016/j.parkreldis.2015.06.002
Eltahawy HA, Saint-Cyr J, Poon YY et al (2004) Pallidal deep brain stimulation in cervical dystonia: clinical outcome in four cases. Can J Neurol Sci 31:328–332. https://doi.org/10.1017/S0317167100003401
Eltahawy HA, Saint-Cyr J, Giladi N et al (2004) Primary dystonia is more responsive than secondary dystonia to pallidal interventions: outcome after pallidotomy or pallidal deep brain stimulation. Neurosurgery 54:613–619. https://doi.org/10.1227/01.NEU.0000108643.94730.21 (discussion 619-621)
Goto S, Yamada K (2004) Long term continuous bilateral pallidal stimulation produces stimulation independent relief of cervical dystonia. J Neurol Neurosurg Psychiatry 75:1506–1507. https://doi.org/10.1136/jnnp.2003.031104
Goto S, Mita S, Ushio Y (2002) Bilateral pallidal stimulation for cervical dystonia. An optimal paradigm from our experiences. Stereotact Funct Neurosurg 79:221–227. https://doi.org/10.1159/000070835
Hamani C, Moro E, Zadikoff C et al (2008) Location of active contacts in patients with primary dystonia treated with globus pallidus deep brain stimulation. Neurosurgery 62:217–223. https://doi.org/10.1227/01.neu.0000317396.16089.bc (discussion 223-225)
Huebl J, Brücke C, Schneider GH et al (2015) Bradykinesia induced by frequency-specific pallidal stimulation in patients with cervical and segmental dystonia. Parkinsonism Relat Disord 21:800–803. https://doi.org/10.1016/j.parkreldis.2015.04.023
Huh R, Song IU, Chung M (2018) Neuropsychological consequences of pallidal deep brain stimulation altering brain networks. J Clin Neurosci 54:50–56. https://doi.org/10.1016/j.jocn.2018.05.004
Huh R, Han IB, Chung M, Chung S (2010) Comparison of treatment results between selective peripheral denervation and deep brain stimulation in patients with cervical dystonia. Stereotact Funct Neurosurg 88:234–238. https://doi.org/10.1159/000314359
Hung SW, Hamani C, Lozano AM et al (2007) Long-term outcome of bilateral pallidal deep brain stimulation for primary cervical dystonia. Neurology 68:457–459. https://doi.org/10.1212/01.wnl.0000252932.71306.89
Jeong SG, Lee MK, Kang JY et al (2009) Pallidal deep brain stimulation in primary cervical dystonia with phasic type : clinical outcome and postoperative course. J Korean Neurosurg Soc 46:346–350. https://doi.org/10.3340/jkns.2009.46.4.346
Kang DW, Kim HY, Chang JW (2011) Cerebral ischemia related to globus pallidus internus stimulation for cervical dystonia. Stereotact Funct Neurosurg 89:201–204. https://doi.org/10.1159/000325655
Kiss ZH, Doig K, Eliasziw M et al (2004) The Canadian multicenter trial of pallidal deep brain stimulation for cervical dystonia: preliminary results in three patients. Neurosurg Focus 17:E5. https://doi.org/10.3171/foc.2004.17.1.5
Kroneberg D, Plettig P, Schneider GH, Kühn AA (2018) Motor cortical plasticity relates to symptom severity and clinical benefit from deep brain stimulation in cervical dystonia. Neuromodulation 21:735–740. https://doi.org/10.1111/ner.12690
Lee JR, Kiss ZH (2014) Interhemispheric difference of pallidal local field potential activity in cervical dystonia. J Neurol Neurosurg Psychiatry 85:306–310. https://doi.org/10.1136/jnnp-2013-305476
Liu X, Wang S, Yianni J et al (2008) The sensory and motor representation of synchronized oscillations in the globus pallidus in patients with primary dystonia. Brain 131:1562–1573. https://doi.org/10.1093/brain/awn083
Loher TJ, Capelle HH, Kaelin-Lang A et al (2008) Deep brain stimulation for dystonia: outcome at long-term follow-up. J Neurol 255:881–884. https://doi.org/10.1007/s00415-008-0798-6
Moro E, Piboolnurak P, Arenovich T et al (2009) Pallidal stimulation in cervical dystonia: clinical implications of acute changes in stimulation parameters. Eur J Neurol 16:506–512. https://doi.org/10.1111/j.1468-1331.2008.02520.x
Ostrem JL, Marks WJ, Volz MM et al (2007) Pallidal deep brain stimulation in patients with cranial-cervical dystonia (Meige syndrome). Mov Disord 22:1885–1891. https://doi.org/10.1002/mds.21580
Pinsker MO, Volkmann J, Falk D et al (2009) Deep brain stimulation of the internal globus pallidus in dystonia: target localisation under general anaesthesia. Acta Neurochir (Wien) 151:751–758. https://doi.org/10.1007/s00701-009-0375-5
Pinsker MO, Volkmann J, Falk D et al (2008) Electrode implantation for deep brain stimulation in dystonia: a fast spin-echo inversion-recovery sequence technique for direct stereotactic targeting of the GPI. Zentralbl Neurochir 69:71–75. https://doi.org/10.1055/s-2007-1004583
Romito LM, Elia AE, Franzini A et al (2010) Low-voltage bilateral pallidal stimulation for severe meige syndrome in a patient with primary segmental dystonia: case report. Neurosurgery 67:onsE308. https://doi.org/10.1227/01.NEU.0000381768.04640.46 (discussion onsE308)
Sadnicka A, Kimmich O, Pisarek C et al (2013) Pallidal stimulation for cervical dystonia does not correct abnormal temporal discrimination. Mov disord 28:1874–1877. https://doi.org/10.1002/mds.25581
Sakas DE, Panourias IG, Boviatsis EJ et al (2009) Treatment of idiopathic head drop (camptocephalia) by deep brain stimulation of the globus pallidus internus. J Neurosurg 110:1271–1273. https://doi.org/10.3171/2008.9.17659
Shaikh AG, Mewes K, Jinnah HA et al (2014) Globus pallidus deep brain stimulation for adult-onset axial dystonia. Park Relat Disord 20:1279–1282. https://doi.org/10.1016/j.parkreldis.2014.09.005
Tsang EW, Hamani C, Moro E et al (2012) Movement related potentials and oscillatory activities in the human internal globus pallidus during voluntary movements. J Neurol Neurosurg Psychiatry 83:91–97. https://doi.org/10.1136/jnnp.2011.243857
Yianni J, Bain P, Giladi N et al (2003) Globus pallidus internus deep brain stimulation for dystonic conditions: a prospective audit. Mov disord 18:436–442. https://doi.org/10.1002/mds.10380
Yianni J, Bain PG, Gregory RP et al (2003) Post-operative progress of dystonia patients following globus pallidus internus deep brain stimulation. Eur J Neurol 10:239–247. https://doi.org/10.1046/j.1468-1331.2003.00592.x
Kleiner-Fisman G, Liang GS, Moberg PJ et al (2007) Subthalamic nucleus deep brain stimulation for severe idiopathic dystonia: impact on severity, neuropsychological status, and quality of life. J Neurosurg 107:29–36. https://doi.org/10.3171/JNS-07/07/0029
Ostrem JL, Markun LC, Glass GA et al (2014) Effect of frequency on subthalamic nucleus deep brain stimulation in primary dystonia. Parkinsonism Relat Disord 20:432–438. https://doi.org/10.1016/j.parkreldis.2013.12.012
Pahapill PA, O’Connell B (2010) Long-term follow-up study of chronic deep brain stimulation of the subthalamic nucleus for cervical dystonia. Neuromodulation 13:26–30. https://doi.org/10.1111/j.1525-1403.2009.00231.x
Volkmann J, Wolters A, Kupsch A et al (2012) Pallidal deep brain stimulation in patients with primary generalised or segmental dystonia: 5-year follow-up of a randomised trial. Lancet Neurol 11:1029–1038. https://doi.org/10.1016/S1474-4422(12)70257-0
Pauls KAM, Krauss JK, Kämpfer CE et al (2017) Causes of failure of pallidal deep brain stimulation in cases with pre-operative diagnosis of isolated dystonia. Parkinsonism Relat Disord 43:38–48. https://doi.org/10.1016/j.parkreldis.2017.06.023
Tsuboi T, Jabarkheel Z, Foote KD et al (2019) Importance of the initial response to GPi deep brain stimulation in dystonia: a nine year quality of life study. Parkinsonism Relat Disord 64:249–255. https://doi.org/10.1016/j.parkreldis.2019.04.024
Morishita T, Hilliard JD, Okun MS et al (2017) Postoperative lead migration in deep brain stimulation surgery: incidence, risk factors, and clinical impact. PLoS ONE 12:e0183711. https://doi.org/10.1371/journal.pone.0183711
Camargo CH, Cattai L, Teive HA (2015) Pain relief in cervical dystonia with botulinum toxin treatment. Toxins (Basel) 7:2321–2335. https://doi.org/10.3390/toxins7062321
Charles PD, Adler CH, Stacy M et al (2014) Cervical dystonia and pain: characteristics and treatment patterns from CD PROBE (Cervical Dystonia Patient Registry for Observation of OnabotulinumtoxinA Efficacy). J Neurol 261:1309–1319. https://doi.org/10.1007/s00415-014-7343-6
Kulisevsky J, Lleó A, Gironell A et al (2000) Bilateral pallidal stimulation for cervical dystonia: dissociated pain and motor improvement. Neurology 55:1754–1755. https://doi.org/10.1212/wnl.55.11.1754
Bittar RG, Yianni J, Wang S et al (2005) Deep brain stimulation for generalised dystonia and spasmodic torticollis. J Clin Neurosci 12:12–16. https://doi.org/10.1016/j.jocn.2004.03.025
Ni Z, Kim SJ, Phielipp N et al (2018) Pallidal deep brain stimulation modulates cortical excitability and plasticity. Ann Neurol 83:352–362. https://doi.org/10.1002/ana.25156
Ruge D, Cif L, Limousin P et al (2011) Shaping reversibility? Long-term deep brain stimulation in dystonia: the relationship between effects on electrophysiology and clinical symptoms. Brain 134:2106–2115. https://doi.org/10.1093/brain/awr122
Chin WW (1998) The partial least squares approach for structural equation. Modeling. In: Marcoulides GA (ed) Methodology for business and management. Modern methods for business research. Lawrence Erlbaum Associates Publishers, London, pp 295–336
Cheung T, Noecker AM, Alterman RL et al (2014) Defining a therapeutic target for pallidal deep brain stimulation for dystonia. Ann Neurol 76:22–30. https://doi.org/10.1002/ana.24187
Starr PA, Turner RS, Rau G et al (2006) Microelectrode-guided implantation of deep brain stimulators into the globus pallidus internus for dystonia: techniques, electrode locations, and outcomes. J Neurosurg 104:488–501. https://doi.org/10.3171/jns.2006.104.4.488
Pauls KAM, Bröckelmann PJ, Hammesfahr S et al (2018) Dysarthria in pallidal deep brain stimulation in dystonia depends on the posterior location of active electrode contacts: a pilot study. Parkinsonism Relat Disord 47:71–75. https://doi.org/10.1016/j.parkreldis.2017.11.002
Reich MM, Horn A, Lange F et al (2019) Probabilistic mapping of the antidystonic effect of pallidal neurostimulation: a multicentre imaging study. Brain 142:1386–1398. https://doi.org/10.1093/brain/awz046
Rozanski VE, Vollmar C, Cunha JP et al (2014) Connectivity patterns of pallidal DBS electrodes in focal dystonia: a diffusion tensor tractography study. Neuroimage 84:435–442. https://doi.org/10.1016/j.neuroimage.2013.09.009
Tsuboi T, Watanabe H, Tanaka Y et al (2015) Distinct phenotypes of speech and voice disorders in Parkinson’s disease after subthalamic nucleus deep brain stimulation. J Neurol Neurosurg Psychiatry 86:856–864. https://doi.org/10.1136/jnnp-2014-308043
Mahlknecht P, Georgiev D, Akram H et al (2018) Parkinsonian signs in patients with cervical dystonia treated with pallidal deep brain stimulation. Brain 141:3023–3034. https://doi.org/10.1093/brain/awy217
Wolf ME, Capelle HH, Bäzner H et al (2016) Hypokinetic gait changes induced by bilateral pallidal deep brain stimulation for segmental dystonia. Gait Posture 49:358–363. https://doi.org/10.1016/j.gaitpost.2016.07.301
Schrader C, Capelle HH, Kinfe TM et al (2011) GPi-DBS may induce a hypokinetic gait disorder with freezing of gait in patients with dystonia. Neurology 77:483–488. https://doi.org/10.1212/WNL.0b013e318227b19e
Eggink H, Szlufik S, Coenen MA et al (2018) Non-motor effects of deep brain stimulation in dystonia: a systematic review. Parkinsonism Relat Disord 55:26–44. https://doi.org/10.1016/j.parkreldis.2018.06.024
Accolla EA, Herrojo Ruiz M, Horn A et al (2016) Brain networks modulated by subthalamic nucleus deep brain stimulation. Brain 139:2503–2515. https://doi.org/10.1093/brain/aww182
Steinhardt J, Münte TF, Schmid SM et al (2019) A systematic review of body mass gain after deep brain stimulation of the subthalamic nucleus in patients with Parkinson’s disease. Obes Rev. https://doi.org/10.1111/obr.12955(Epub ahead of print)
Alterman RL, Miravite J, Weisz D et al (2007) Sixty hertz pallidal deep brain stimulation for primary torsion dystonia. Neurology 69:681–688. https://doi.org/10.1212/01.wnl.0000267430.95106.ff
Kim JP, Chang WS, Park YS, Chang JW (2012) Effects of relative low-frequency bilateral globus pallidus internus stimulation for treatment of cervical dystonia. Stereotact Funct Neurosurg 90:30–36. https://doi.org/10.1159/000333839
Alterman RL, Filippidis AS (2018) Genetic subtypes and deep brain stimulation in dystonia. Mov Disord Clin Pract 5:357–360. https://doi.org/10.1002/mdc3.12660
Acknowledgements
We would like to acknowledge Tyler’s Hope Foundation for dystonia cure. TT sincerely appreciates the Uehara Memorial Foundation for a research fellowship program.
Funding
Nothing to report.
Author information
Authors and Affiliations
Contributions
(1) Research project: A. conception, B. organization, C. execution; (2) statistical analysis: A. design, B. execution, C. review and critique; (3) manuscript: A. writing of the first draft, B. review and critique. TT: 1A, 1B, 1C, 2A, 2B, 3A. JKW: 1C, 2C, 3B. LA, CWH, AWS, KDF, MSO: 1A, 2C, 3B. ARZ: 1A, 1B, 2C, 3B.
Corresponding author
Ethics declarations
Conflicts of interest
TT was supported by a research fellowship program of the Uehara Memorial Foundation. JKW has nothing to report. LA works as a consultant and participates in advisory boards for Boston Scientific and Medtronic, and has received honoraria for these services. LA has no conflicts of interest pertaining the scope of this manuscript to be declared. CWH has served as a site investigator or co-investigator for research projects funded by the Parkinson’s Foundation and has served as a research committee member for the Michael J. Fox Foundation. CWH has served as a speaker for the National Parkinson Foundation, the Parkinson’s Disease Foundation, and the Davis Phinney Foundation. CWH has participated in CME and educational activities on movement disorders sponsored by Allergan, Ipsen, Mertz Pharmaceuticals, Peerview Online, UptoDate, and QuantiaMD. AWS reports grants from the NIH and has received grant support from Benign Essential Blepharospasm Research foundation, Dystonia coalition, Dystonia Medical Research foundation, National Organization for Rare Disorders and grant support from NIH (KL2 and K23 NS092957-01A1). KDF reports grants from NIH, and other funding from Donnellan/Einstein/Merz Chair, during this study; grants and non-financial support from Medtronic, grants from St Jude, Functional Neuromodulation, and Boston Scientific, and grants and other funding from Neuropace. Additionally, KDF has a patent US 8295935 B2 issued for a DBS cranial lead fixation device. MSO serves as consultant for the National Parkinson’s Foundation, and has received research grants from the National Institutes of Health, National Parkinson’s Foundation, Michael J. Fox Foundation, Parkinson Alliance, Smallwood Foundation, Bachmann-Strauss Foundation, Tourette Syndrome Association, and UF Foundation. MSO has previously received honoraria, but in the past > 60 months has received no support from industry. MSO has received royalties for publications with Demos, Manson, Amazon, Smashwords, Books4Patients, and Cambridge (movement disorders books). MSO is an associate editor for New England Journal of Medicine Journal Watch Neurology. MSO has participated in CME and educational activities on movement disorders (in the last 36 months) sponsored by PeerView, Prime, Quantia, Henry Stewart, and the Vanderbilt University. The institution and not MSO receives grants from Medtronic, Abbvie, and ANS/St. Jude, and the PI has no financial interest in these grants. MSO has participated as a site PI and/or co-I for several NIH, foundation, and industry sponsored trials over the years but has not received honoraria. AWS reports grants from the NIH and has received grant support from Benign Essential Blepharospasm Research foundation, Dystonia coalition, Dystonia Medical Research foundation, National Organization for Rare Disorders and grant support from NIH (KL2 and K23 NS092957-01A1). ARZ acknowledges research grants from the Parkinson’s Foundation and has received consulting honoraria from Medtronic, Boston Scientific, Bracket, Stealth, Rho Inc in the past 24 months.
Ethical standards
This pooled meta-analysis used only the published data.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tsuboi, T., Wong, J.K., Almeida, L. et al. A pooled meta-analysis of GPi and STN deep brain stimulation outcomes for cervical dystonia. J Neurol 267, 1278–1290 (2020). https://doi.org/10.1007/s00415-020-09703-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09703-9