Abstract
Background
Following a doctor’s prescribed medication regimen is the key to prevent recurrent stroke and adverse outcomes. Many studies have investigated post-stroke drug adherence and persistence in patients. However, a comprehensive analysis of the data is lacking.
Objectives
A meta-analysis of published literature was conducted to summarize the ratio of medication adherence and persistence in patients after stroke.
Methods
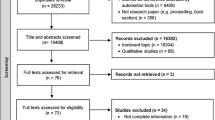
Relevant studies were identified by conducting a literature search using PubMed, EMBASE and Web of Science up to April 2019. We also reviewed the reference list of the retrieved articles to identify additional studies. We included observational studies that reported data on patients’ medication adherence or persistence status, or the rate of medication adherence or persistence among patients with stroke could be calculated based on the information provided.
Results
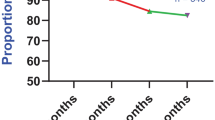
The overall high medication adherence rate of patients with stroke was 64.1% (95% CI: 57.4%–70.8%), and the persistence rate of patients with stroke was 72.2% (95% CI: 69.1%–75.3%). The highest persistence rate was observed in cohort studies which was 80.1% (95% CI: 76.7%–83.4%). The medication adherence rate was the highest in cases where the rates were assessed through interviews or self-reports (77.7% (95% CI: 71.3%–84.1%)).
Conclusions
Medication adherence and persistence rates are low in patients after suffering a stroke. Patient medication adherence or persistence and their influencing factors should be considered for the treatment of stroke patients. More detailed disease prevention and management strategies need to be developed for stroke patients with different comorbidities.




Similar content being viewed by others
References
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N et al (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159):1789–1858
Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N et al (2018) Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159):1859–1922
Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016. Geneva, World Health Organization;2018. https://www.who.int/healthinfo/global_burden_disease/estimates/en/.
Arima H, Tzourio C, Butcher K, Anderson C, Bousser MG, Lees KR et al (2006) Prior events predict cerebrovascular and coronary outcomes in the PROGRESS trial. Stroke 37(6):1497–1502
Hankey GJ (2014) Secondary stroke prevention. Lancet Neurol 13(2):178–194
Wang P, Wang Y, Zhao X, Du W, Wang A, Liu G et al (2016) In-hospital medical complications associated with stroke recurrence after initial ischemic stroke: a prospective cohort study from the China National Stroke Registry. Medicine. 95(37):e4929
Mi D, Jia Q, Zheng H, Hoff K, Zhao X, Wang C et al (2012) Metabolic syndrome and stroke recurrence in Chinese ischemic stroke patients–the ACROSS-China study. PLoS ONE 7(12):e51406
Coull AJ, Rothwell PM (2004) Underestimation of the early risk of recurrent stroke: evidence of the need for a standard definition. Stroke 35(8):1925–1929
Rothwell PM, Coull AJ, Giles MF, Howard SC, Silver LE, Bull LM et al (2004) Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study). Lancet 363(9425):1925–1933
Hardie K, Hankey GJ, Jamrozik K, Broadhurst RJ, Anderson C (2004) Ten-year risk of first recurrent stroke and disability after first-ever stroke in the Perth Community Stroke Study. Stroke 35(3):731–735
Lekoubou A, Nkoke C, Dzudie A, Kengne AP (2017) Recurrent stroke and early mortality in an urban medical Unit in Cameroon. J Stroke Cerebrovasc Dis 26(8):1689–1694
Pendlebury ST, Rothwell PM (2009) Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol 8(11):1006–1018
Luengo-Fernandez R, Gray AM, Rothwell PM (2012) A population-based study of hospital care costs during 5 years after transient ischemic attack and stroke. Stroke 43(12):3343–3351
Kim J, Lee HS, Nam CM, Heo JH (2017) Effects of statin intensity and adherence on the long-term prognosis after acute ischemic stroke. Stroke 48(10):2723–2730
Perreault S, Yu AY, Cote R, Dragomir A, White-Guay B, Dumas S (2012) Adherence to antihypertensive agents after ischemic stroke and risk of cardiovascular outcomes. Neurology 79(20):2037–2043
Rijkmans M, de Jong G, van den Berg JSP (2018) Non-persistence in ischaemic stroke: risk of recurrent vascular events. Acta Neurol 137(3):288–292
Boehme A (2017) Smoking cessation and secondary stroke prevention. Neurology 89(16):1656–1657
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD et al (2014) Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45(7):2160–2236
Algra A, Wermer MJ (2017) Stroke in 2016: Stroke is treatable, but prevention is the key. Nat Rev Neurol 13(2):78–79
Xu J, Wang CX, Wang YL, Zhao XQ, Liu LP, Wang AX et al (2013) Persistence with antihypertensive agents for 12 months after ischemic stroke reduces the rates of death and dependency. CNS Neurosci Ther 19(2):142–144
Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K et al (2006) Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Circulation 113(10):e409–e449
Rothwell PM, Algra A, Amarenco P (2011) Medical treatment in acute and long-term secondary prevention after transient ischaemic attack and ischaemic stroke. Lancet 377(9778):1681–1692
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA et al (2008) Medication compliance and persistence: terminology and definitions. Value Health 11(1):44–47
Kronish IM, Diefenbach MA, Edmondson DE, Phillips LA, Fei K, Horowitz CR (2013) Key barriers to medication adherence in survivors of strokes and transient ischemic attacks. J Gen Intern Med 28(5):675–682
Ostergaard K, Hallas J, Bak S, Christensen R, Gaist D (2012) Long-term use of antiplatelet drugs by stroke patients: a follow-up study based on prescription register data. Eur J Clin Pharmacol 68(12):1631–1637
Jiang Y, Yang X, Li Z, Pan Y, Wang Y, Wang Y et al (2017) Persistence of secondary prevention medication and related factors for acute ischemic stroke and transient ischemic attack in China. Neurol Res 39(6):492–497
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama. 2000;283(15):2008–12.
Rostom A, Dubé C, Cranney A, et al. Celiac Disease. Rockville (MD): Agency for Healthcare Research and Quality (US); 2004 Sep. (Evidence Reports/Technology Assessments, No. 104.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK35149/.
Mathew MC, Ervin AM, Tao J, Davis RM. Antioxidant vitamin supplementation for preventing and slowing the progression of age-related cataract. Cochrane Database Syst Rev 2012(6):Cd004567.
Zeng Y, Tang Y, Tang J, Shi J, Zhang L, Zhu T, et al. Association between the different duration of breastfeeding and attention deficit/hyperactivity disorder in children: a systematic review and meta-analysis. Nutr Neurosci 2018:1–13.
Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, ON: Ottawa Health Research Institute, 2009 https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Gan Y, Yang C, Tong X, Sun H, Cong Y, Yin X et al (2015) Shift work and diabetes mellitus: a meta-analysis of observational studies. Occup Environ Med 72(1):72–78
Hess LM, Raebel MA, Conner DA, Malone DC (2006) Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. Ann Pharmacother 40(7–8):1280–1288
Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J (2002) Long-term persistence in use of statin therapy in elderly patients. JAMA 288(4):455–461
Khan NA, Yun L, Humphries K, Kapral M (2010) Antihypertensive drug use and adherence after stroke: are there sex differences? Stroke 41(7):1445–1449
Skaer TL, Sclar DA, Robison LM, Markowski DJ, Won JK (1993) Effect of pharmaceutical formulation for diltiazem on health care expenditures for hypertension. Clin Ther 15(5):905–911
Morisky DE, Ang A, Krousel-Wood M, Ward HJ (2008) Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich, Conn). 10(5):348–354
Morisky DE, Green LW, Levine DM (1986) Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 24(1):67–74
Mefford M, Safford MM, Muntner P, Durant RW, Brown TM, Levitan EB (2017) Insurance, self-reported medication adherence and LDL cholesterol: the REasons for Geographic And Racial Differences in Stroke study. Int J Cardiol 236:462–465
Lam WY, Fresco P (2015) Medication adherence measures: an overview. Biomed Res Int 2015:217047
Polymeris AA, Traenka C, Hert L, Seiffge DJ, Peters N, De Marchis GM et al (2016) Frequency and determinants of adherence to oral anticoagulants in stroke patients with atrial fibrillation in clinical practice. Eur Neurol 76(3–4):187–193
Horne R, Weinman J (1999) Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res 47(6):555–567
Wei L, Champman S, Li X, Li X, Li S, Chen R et al (2017) Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: a cross-sectional study in China. BMJ Open 7(10):e017293
Lank RJ, Lisabeth LD, Levine DA, Zahuranec DB, Kerber KA, Shafie-Khorassani F et al (2019) Ethnic differences in 90-day poststroke medication adherence. Stroke 50(6):1519–1524
Bushnell CD, Olson DM, Zhao X, Pan W, Zimmer LO, Goldstein LB et al (2011) Secondary preventive medication persistence and adherence 1 year after stroke. Neurology 77(12):1182–1190
De Schryver EL, van Gijn J, Kappelle LJ, Koudstaal PJ, Algra A (2005) Non-adherence to aspirin or oral anticoagulants in secondary prevention after ischaemic stroke. J Neurol 252(11):1316–1321
Arif H, Aijaz B, Islam M, Aftab U, Kumar S, Shafqat S (2007) Drug compliance after stroke and myocardial infarction: a comparative study. Neurol India 55(2):130–135
Kohok DD, Sico JJ, Baye F, Myers L, Coffing J, Kamalesh M et al (2018) Post-stroke hypertension control and receipt of health care services among veterans. J Clin Hypertens (Greenwich, Conn) 20(2):382–387
Dahlgren C, Geary L, Hasselstrom J, Rehnberg C, Schenck-Gustafsson K, Wandell P et al (2017) Recording a diagnosis of stroke, transient ischaemic attack or myocardial infarction in primary healthcare and the association with dispensation of secondary preventive medication: a registry-based prospective cohort study. BMJ Open 7(9):e015723
Mechtouff L, Haesebaert J, Viprey M, Tainturier V, Termoz A, Porthault-Chatard S et al (2018) Secondary prevention three and six years after stroke using the french national insurance healthcare system database. Eur Neurol 79(5–6):272–280
Thiebaud P, Patel BV, Nichol MB, Berenbeim DM (2005) The effect of switching on compliance and persistence: the case of statin treatment. Am J Manag Care 11(11):670–674
Rothwell PM, Algra A, Chen Z, Diener HC, Norrving B, Mehta Z (2016) Effects of aspirin on risk and severity of early recurrent stroke after transient ischaemic attack and ischaemic stroke: time-course analysis of randomised trials. Lancet 388(10042):365–375
Hackam DG, Spence JD (2007) Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study. Stroke 38(6):1881–1885
Acknowledgements
JZ and XY conceived the study. JZ and YG conducted the literature search. YG identified potentially relevant research based on the title and abstract of the article. JZ and YZ reviewed these potential studies and determined the final included studies according to the inclusion and exclusion criteria. JZ and YG extracted data from the included studies and assessed the quality of the studies. NJ and JW checked the extracted data. JZ and YG analyzed the data and prepared the draft of the manuscript. XY and YG criticized and revised the manuscript. All authors reviewed the study findings and read and approved the final manuscript. XY is the guarantor of this study.
Funding
This study was a part of our routine work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There were no conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, J., Gong, Y., Zhao, Y. et al. Post-stroke medication adherence and persistence rates: a meta-analysis of observational studies. J Neurol 268, 2090–2098 (2021). https://doi.org/10.1007/s00415-019-09660-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09660-y