Abstract
Objectives
The outcome of aphasia at 3 months is variable in patients with moderate/severe stroke. The aim was to predict 3-month aphasia outcome using prediction models including initial severity in addition to the interaction between lesion size and location at the acute phase.
Methods
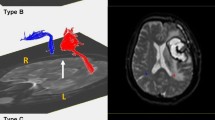
Patients with post-stroke aphasia (assessed by the Aphasia Rapid Test at day 7-ART D7) and MRI performed at day 1 were enrolled (n = 73). Good outcome at 3-months was defined by an Aphasia Handicap Score of 0–2. Each infarct lesion was overlapped with an area of interest in the left temporo-parietal region to compute an intersection index (proportion of the critical region damaged by the infarct). We tested ART D7, age, lesion volume, and intersection index as well as a combined variable lesion volume*intersection in a univariate analysis. Then, we performed a multivariate analysis to investigate which variables were independent predictors of good outcome.
Results
ART at D7, infarct volume, and the intersection index were univariate predictors of good outcome. In the multivariate analysis, ART D7 and “volume ≥ 50 ml or intersection index ≥ 20%” correctly classified 89% of the patients (p < 0.0001). When added to the model, the interaction between both variables was significant indicating that the impact of the size or site variable depends on the initial severity of aphasia.
Conclusion
In patients with initially severe aphasia, large infarct size or critical damage in left temporoparietal junction is associated with poor language outcome at 3 months.



Similar content being viewed by others
References
Kertesz A, McCabe P (1977) Recovery patterns and prognosis in aphasia. Brain 100(Pt 1):1–18
Wade DT, Hewer RL, David RM, Enderby PM (1986) Aphasia after stroke: natural history and associated deficits. J Neurol Neurosurg Psychiatry 49:11–16
Pedersen PM, Vinter K, Olsen TS (2004) Aphasia after stroke: type, severity and prognosis. The Copenhagen aphasia study. Cerebrovasc Dis 17:35–43. https://doi.org/10.1159/000073896
Pedersen PM, Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS (1995) Aphasia in acute stroke: incidence, determinants, and recovery. Ann Neurol 38:659–666
Laska AC, Hellblom A, Murray V et al (2001) Aphasia in acute stroke and relation to outcome. J Intern Med 249:413–422
Lazar RM, Speizer AE, Festa JR et al (2008) Variability in language recovery after first-time stroke. J Neurol Neurosurg Psychiatry 79:530–534. https://doi.org/10.1136/jnnp.2007.122457
Lazar RM, Minzer B, Antoniello D et al (2010) Improvement in aphasia scores after stroke is well predicted by initial severity. Stroke 41:1485–1488. https://doi.org/10.1161/STROKEAHA.109.577338
Azuar C, Leger A, Arbizu C et al (2013) The Aphasia Rapid Test: an NIHSS-like aphasia test. J Neurol 260:2110–2117. https://doi.org/10.1007/s00415-013-6943-x
El Hachioui H, Lingsma HF, Van de Sandt-Koenderman MW et al (2013) Long-term prognosis of aphasia after stroke. J Neurol Neurosurg Psychiatry 84:310–315. https://doi.org/10.1136/jnnp-2012-302596
Plowman E, Hentz B, Ellis C Jr (2012) Post-stroke aphasia prognosis: a review of patient-related and stroke-related factors. J Eval Clin Pract 18:689–694. https://doi.org/10.1111/j.1365-2753.2011.01650.x
Watila MM, Balarabe SA (2015) Factors predicting post-stroke aphasia recovery. J Neurol Sci 352:12–18. https://doi.org/10.1016/j.jns.2015.03.020
Krakauer JW, Marshall RS (2015) The proportional recovery rule revisited. Ann Neurol 78:845–847. https://doi.org/10.1002/ana.24537
Marchi NA, Ptak R, Di Pietro M, Schnider A, Guggisberg AG (2017) Principles of proportional recovery after stroke generalize to neglect and aphasia. Eur J Neurol 24:1084–1087. https://doi.org/10.1111/ene.13296
Hope TMH, Friston K, Price CJ, Leff AP, Rotshtein P, Bowman H (2019) Recovery after stroke: not so proportional after all? Brain 142:15–22. https://doi.org/10.1093/brain/awy302
Hawe RL, Scott SH, Dukelow SP (2019) Taking proportional out of stroke recovery. Stroke 50:204–211. https://doi.org/10.1161/STROKEAHA.118.023006
Samson Y, Belin P, Zilbovicius M et al (1999) Mechanisms of aphasia recovery and brain imaging. Rev Neurol (Paris) 155:725–730
Marchina S, Zhu LL, Norton A et al (2011) Impairment of speech production predicted by lesion load of the left arcuate fasciculus. Stroke 42:2251–2256. https://doi.org/10.1161/STROKEAHA.110.606103
Rosso C, Vargas P, Valabregue R et al (2015) Aphasia severity in chronic stroke patients: a combined disconnection in the dorsal and ventral language pathways. Neurorehabilit Neural Repair 29:287–295. https://doi.org/10.1177/1545968314543926
Hillis AE, Beh YY, Sebastian R et al (2018) Predicting recovery in acute poststroke aphasia. Ann Neurol 83:612–622. https://doi.org/10.1002/ana.25184
Ivanova MV, Isaev DY, Dragoy OV et al (2016) Diffusion-tensor imaging of major white matter tracts and their role in language processing in aphasia. Cortex 85:165–181. https://doi.org/10.1016/j.cortex.2016.04.019
Hope TMH, Leff AP, Price CJ (2018) Predicting language outcomes after stroke: is structural disconnection a useful predictor? Neuroimage Clin 19:22–29. https://doi.org/10.1016/j.nicl.2018.03.037
Hope TMH, Seghier M, Leff AP, Price CJ (2013) Predicting outcome and recovery after stroke with lesions extracted from MRI images. Neuroimage Clin 2:424–433
Ramsey LE, Siegel JS, Lang CE et al (2017) Behavioural clusters and predictors of performance during recovery from stroke. Nat Hum Behav 1:0038. https://doi.org/10.1038/s41562-016-0038
Tabuas-Pereira M, Freitas S, Beato-Coelho J et al (2018) Aphasia rapid test: translation, adaptation and validation studies for the Potuguese population. Acta Med Port 31:265–271. https://doi.org/10.20344/amp.9090
Flamand-Roze C, Falissard B, Roze E et al (2011) Validation of a new language screening tool for patients with acute stroke: the language screening test (LAST). Stroke 42:1224–1229. https://doi.org/10.1161/STROKEAHA.110.609503
Jayakumar H, Samivel B, Janarthanam M et al (2018) Aphasia rapid test—quantification and assessment of aphasia in stroke (P3.320). Neurology 90(15 supplement). http://n.neurology.org/content/90/15_Supplement/P3.230 (Abstract)
Goodglass H, Kaplan E (1983) The assessment of aphasia and related disorders, second edition 1983 ed. Lea & Febiger 600 South Washington Square, Philadelphia
Laska AC, Bartfai A, hellblom A, Murray V, Kahan T (2007) Clinical and prognostic properties of standardized and functional aphasia assessments. J Rehabil Med 39:387–392
Weimar C, König IR, Kraywinkel K, Ziegler A, Diener HC (2004) Age and National Institute of Health Stroke Scale Score within 6 hours after onset are accurate predictors of outcome after cerebral ischemia: development and external validation of prognostic models. Stroke 35:158–162
Park CH, Kou N, Boudrias MH, Playford ED, Ward NS (2013) Assessing a standardised approach to measuring corticospinal integrity after stroke with DTI. Neuroimage Clin 2:521–533. https://doi.org/10.1016/j.nicl.2013.04.002
Rosso C, Colliot O, Valabregue R et al (2011) Tissue at risk in the deep middle cerebral artery territory is critical to stroke outcome. Neuroradiology 53:763–771. https://doi.org/10.1007/s00234-011-0916-5
El Hachioui H, Visch-Brink EG, de Lau LM et al (2017) Screening tests for aphasia in patients with stroke: a systematic review. J Neurol 264:211–220. https://doi.org/10.1007/s00415-016-8170-8
Glize B, Villain M, Richert L et al (2017) Language features in the acute phase of poststroke severe aphasia could predict the outcome. Eur J Phys Rehabil Med 53:249–255. https://doi.org/10.23736/S1973-9087.16.04255-6
Knopman DS, Selnes OA, Niccum N, Rubens AB (1984) Recovery of naming in aphasia: relationship to fluency, comprehension and CT findings. Neurology 34:1461–1470
Saur D, Ronneberger O, Kummerer D et al (2010) Early functional magnetic resonance imaging activations predict language outcome after stroke. Brain 133:1252–1264. https://doi.org/10.1093/brain/awq021
Lyden P (2017) Using the National Institutes of Health Stroke Scale: a cautionary tale. Stroke 48:513–519. https://doi.org/10.1161/STROKEAHA.116.015434
Acknowledgements
The Pitié-Salpêtrière registry was supported by the French Ministry of Health grant EVALUSINV PHRC AOM 03 008. The research leading to these results has received funding from “Investissements d’avenir” ANR-10-IAIHU-06.
Funding
No grant was provided for this analysis and this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have none.
Patient consent and ethics
The Pitié-Salpêtrière registry has approval by an ethics committee (Paris VI ethic committee). However and in accordance with French legislation, written informed consent from patients was waived, as it is a retrospective database implying only analysis of anonymized data collected prospectively as part of routine clinical care.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Benghanem, S., Rosso, C., Arbizu, C. et al. Aphasia outcome: the interactions between initial severity, lesion size and location. J Neurol 266, 1303–1309 (2019). https://doi.org/10.1007/s00415-019-09259-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09259-3