Abstract
Background
Despite the consensus on the necessity of revascularizing surgery in Moyamoya angiopathy in Asia, the indication in Caucasian Moyamoya patients is discussed controversially.
Objective
The safety of revascularizing surgery in Europe should be clarified.
Methods
This study retrospectively analyzed the rate of complications as well as clinical symptoms within the first 3 months after bypass surgery between superficial temporal artery and middle cerebral artery (STA–MCA).
Results
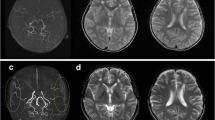
64 direct bypass procedures in 45 patients (95.5% Caucasians) were analyzed. The magnetic resonance imaging at day 6 showed subdural hematoma in 60.3%. The mean diameter of these hematomas on magnetic resonance imaging was 5.1 mm (SD 3.4 mm) and increased in 25% at follow-up. No difference was found between those patients with early (day 1) or late (day 7) restarts of antiplatelet therapy. Magnetic resonance imaging at day 6 revealed hyperperfusion syndrome after six of 64 procedures (9.3%). Three of these six had clinical symptoms; two-thirds were transient within seconds. Magnetic resonance imaging depicted stroke after seven procedures (10.9%). Five of these seven patients had no new symptoms. Altogether, after ten procedures (15%), patients complained about clinical symptoms. These were all transient. No new transient ischemic attacks occurred during the 3 month follow-up and no new lesions were detected in magnetic resonance imaging. Only two patients underwent surgery for asymptomatic subdural hematoma. All other subdural hematomas resolved spontaneously.
Conclusion
Revasculating surgery is a safe procedure in Caucasian patients with Moyamoya angiopathy. The observed complications have a good prognosis.




Similar content being viewed by others

References
Kraemer M, Heienbrok W, Berlit P (2008) Moyamoya disease in Europeans. Stroke 39(12):3193–3200
EC/IC Bypass Study Group (1985) Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. The EC/IC Bypass Study Group. N Engl J Med 313(19):1191–1200
Powers WJ, Clarke WR, Grubb RL Jr et al (2011) Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. Jama 306(18):1983–1992
Powers WJ, Grubb RL Jr, Raichle ME (1989) Clinical results of extracranial-intracranial bypass surgery in patients with hemodynamic cerebrovascular disease. J Neurosurg 70(1):61–67
Miyamoto S, Yoshimoto T, Hashimoto N et al (2014) Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: results of the Japan Adult Moyamoya Trial. Stroke 45(5):1415–1421
Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis; Health Labour Sciences Research Grant for Research on Measures for Infractable Diseases (2012) Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo) 52(5):245–266
Jeon JP, Kim JE, Cho WS, Bang JS, Son YJ, Oh CW (2018) Meta-analysis of the surgical outcomes of symptomatic moyamoya disease in adults. J Neurosurg 128(3):793–799
Yao Z, You C (2018) Effect of surgery on the long-term functional outcome of moyamoya disease: a meta-analysis. Turk Neurosurg. https://doi.org/10.5137/1019-5149.JTN.22598-18.3
Qian C, Yu X, Li J, Chen J, Wang L, Chen G (2015) The efficacy of surgical treatment for the secondary prevention of stroke in symptomatic moyamoya disease: a meta-analysis. Medicine 94(49):e2218
Herve D, Kossorotoff M, Bresson D et al (2018) French clinical practice guidelines for Moyamoya angiopathy. Rev Neurol (Paris) 174(5):292–303
Hanggi D, Steiger HJ, Vajkoczy P (2014) The role of MCA-STA bypass surgery after COSS and JET: the European point of view. Acta Neurochir Suppl 119:77–78
Hanggi D, Steiger HJ, Vajkoczy P (2012) Cerebrovascular Section of the European Association of Neurological Surgeons. EC-IC bypass for stroke: is there a future perspective? Acta Neurochir (Wien) 154(10):1943–1944
Yu J, Shi L, Guo Y, Xu B, Xu K (2016) Progress on complications of direct bypass for Moyamoya disease. Int J Med Sci 13(8):578–587
Fujimura M, Tominaga T (2012) Lessons learned from moyamoya disease: outcome of direct/indirect revascularization surgery for 150 affected hemispheres. Neurol Med Chir (Tokyo) 52(5):327–332
Fujimura M, Mugikura S, Kaneta T, Shimizu H, Tominaga T (2009) Incidence and risk factors for symptomatic cerebral hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in patients with moyamoya disease. Surg Neurol 71(4):442–447
Kazumata K, Ito M, Tokairin K et al (2014) The frequency of postoperative stroke in moyamoya disease following combined revascularization: a single-university series and systematic review. J Neurosurg 121(2):432–440
Jin SC, Oh CW, Kwon OK et al (2011) Epilepsy after bypass surgery in adult moyamoya disease. Neurosurgery 68(5):1227–1232 discussion 1232.
Andoh T, Sakai N, Yamada H et al (1992) Chronic subdural hematoma following bypass surgery—report of three cases. Neurol Med Chir (Tokyo) 32(9):684–689
Czabanka M, Boschi A, Acker G et al (2016) Grading of moyamoya disease allows stratification for postoperative ischemia in bilateral revascularization surgery. Acta Neurochir (Wien) 158(10):1895–1900
Pena-Tapia PG, Kemmling A, Czabanka M, Vajkoczy P, Schmiedek P (2008) Identification of the optimal cortical target point for extracranial-intracranial bypass surgery in patients with hemodynamic cerebrovascular insufficiency. J Neurosurg 108(4):655–661
Horn P, Scharf J, Pena-Tapia P, Vajkoczy P (2008) Risk of intraoperative ischemia due to temporary vessel occlusion during standard extracranial-intracranial arterial bypass surgery. J Neurosurg 108(3):464–469
Hori S, Acker G, Vajkoczy P (2016) Radial artery grafts as rescue strategy for patients with Moyamoya disease for whom conventional revascularization failed. World Neurosurg 85:77–84
Kuhn FP, Warnock G, Schweingruber T, Sommerauer M, Buck A, Khan N (2015) Quantitative H2[(15)O]-PET in pediatric moyamoya disease: evaluating perfusion before and after cerebral revascularization. J Stroke Cerebrovasc Dis 24(5):965–971
Khan N, Yonekawa Y (2008) Moyamoya angiopathy in Europe: the beginnings in Zurich, practical lessons learned, increasing awareness and future perspectives. Acta Neurochir Suppl 103:127–130
Khan N, Yonekawa Y (2005) Moyamoya angiopathy in Europe. Acta Neurochir Suppl 94:149–152
Khan N, Schuknecht B, Boltshauser E et al (2003) Moyamoya disease and Moyamoya syndrome: experience in Europe; choice of revascularisation procedures. Acta Neurochir (Wien) 145(12):1061–1071 discussion 1071.
Yonekawa Y, Ogata N, Kaku Y, Taub E, Imhof HG (1997) Moyamoya disease in Europe, past and present status. Clin Neurol Neurosurg 99(Suppl 2):S58–S60
Thines L, Petyt G, Aguettaz P et al (2015) Surgical management of Moyamoya disease and syndrome: current concepts and personal experience. Rev Neurol (Paris) 171(1):31–44
Hanggi D, Mehrkens JH, Schmid-Elsaesser R, Steiger HJ (2008) Results of direct and indirect revascularisation for adult European patients with Moyamoya angiopathy. Acta Neurochir Suppl 103:119–122
Ulrich PT, Januschek E (2011) Revascularisation surgery and long-term follow-up in juvenile Moyamoya syndrome: a retrospective analysis. Acta Neurochir Suppl 112:39–43
Lanterna LA, Brembilla C, Gritti P, Bernucci C (2016) Universal bypass for treatment of symptomatic moyamoya disease or Moyamoya syndrome. Analysis of a personal case series on Behalf of the Italian Moyamoya Association. Acta Neurochir Suppl 123:129–132
Guzman R, Lee M, Achrol A et al (2009) Clinical outcome after 450 revascularization procedures for moyamoya disease. Clinical article. J Neurosurg 111(5):927–935
Teo M, Johnson J, Steinberg GK (2017) Strategies for and outcome of repeat revascularization surgery for Moyamoya disease: an American Institutional Series. Neurosurgery 81(5):852–859
Schubert GA, Biermann P, Weiss C et al (2014) Risk profile in extracranial/intracranial bypass surgery—the role of antiplatelet agents, disease pathology, and surgical technique in 168 direct revascularization procedures. World Neurosurg 82(5):672–677
Uchino H, Kuroda S, Hirata K, Shiga T, Houkin K, Tamaki N (2012) Predictors and clinical features of postoperative hyperperfusion after surgical revascularization for moyamoya disease: a serial single photon emission CT/positron emission tomography study. Stroke 43(10):2610–2616
Narisawa A, Fujimura M, Shimizu H, Tominaga T (2007) Seizure following superficial temporal-middle cerebral artery anastomosis in patients with moyamoya disease: possible contribution of postoperative cerebral hyperperfusion. No Shinkei Geka 35(5):467–474
Takanari K, Araki Y, Okamoto S et al (2015) Operative wound-related complications after cranial revascularization surgeries. J Neurosurg 123(5):1145–1150
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standards
This study was approved by local ethics-committee.
Rights and permissions
About this article
Cite this article
Kraemer, M., Sassen, J., Karakaya, R. et al. Moyamoya angiopathy: early postoperative course within 3 months after STA–MCA–bypass surgery in Europe—a retrospective analysis of 64 procedures. J Neurol 265, 2370–2378 (2018). https://doi.org/10.1007/s00415-018-8997-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8997-2