Abstract
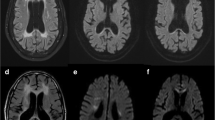
Vanishing white matter disease (VWM) is one of the most prevalent inherited leukoencephalopathies in childhood. Infantile VWM is more severe but less understood than the classic early childhood type. We performed a follow-up study on 14 infantile and 26 childhood patients to delineate the natural history and neuroimaging features of VWM. Infantile and childhood patients shared similarities in the incidence of epileptic seizure (35.7 vs. 38.5%) and episodic aggravation (92.9 vs. 84.6%). Developmental delay before disease onset was more common in infantile patients. Motor disability was earlier and more severe in infantile VWM. In survivors with disease durations of 1–3 years, the Gross Motor Function Classification System (GMFCS) was classified as IV–V in 66.7% of infantile and only 29.4% of childhood patients. Kaplan–Meier survival curve analysis indicated that the 5-year survival rates were 21.6 and 91.3% in infantile and childhood VWM, respectively. In terms of MRI, infantile patients showed more extensive involvement and earlier rarefaction, with more common involvement of subcortical white matter, internal capsule, brain stem and dentate nuclei of the cerebellum. Restricted diffusion was more diffuse or extensive in infantile patients. In addition, four novel mutations were identified. In conclusion, we identified some similarities and differences in the natural history and neuroimaging features between infantile and early childhood VWM.




Similar content being viewed by others
References
van der Knaap MS, Pronk JC, Scheper GC (2006) Vanishing white matter disease. Lancet Neurol 5(5):413–423. https://doi.org/10.1016/S1474-4422(06)70440-9
Bugiani M et al (2010) Leukoencephalopathy with vanishing white matter: a review. J Neuropathol Exp Neurol 69(10):987–996. https://doi.org/10.1097/NEN.0b013e3181f2eafa
Leegwater PA et al (2001) Subunits of the translation initiation factor eIF2B are mutant in leukoencephalopathy with vanishing white matter. Nat Genet 29(4):383–388. https://doi.org/10.1038/ng764
van der Knaap MS et al (2002) Mutations in each of the five subunits of translation initiation factor eIF2B can cause leukoencephalopathy with vanishing white matter. Ann Neurol 51(2):264–270
Scheper GC, Proud CG, van der Knaap MS (2006) Defective translation initiation causes vanishing of cerebral white matter. Trends Mol Med 12(4):159–166. https://doi.org/10.1016/j.molmed.2006.02.006
Pan YX et al (2009) Eukaryotic translation initiation factor 2B and leukoencephalopathy with vanishing white matter. Beijing Da Xue Xue Bao 41(5):608–610
van der Knaap MS et al (1998) Phenotypic variation in leukoencephalopathy with vanishing white matter. Neurology 51(2):540–547
Fogli A et al (2002) A severe variant of childhood ataxia with central hypomyelination/vanishing white matter leukoencephalopathy related to EIF21B5 mutation. Neurology 59(12):1966–1968
Richards S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424. https://doi.org/10.1038/gim.2015.30
Shevell MI et al (2009) Comorbidities in cerebral palsy and their relationship to neurologic subtype and GMFCS level. Neurology 72(24):2090–2096. https://doi.org/10.1212/WNL.0b013e3181aa537b
Malt MA et al (2016) Correlation between the Gait Deviation Index and gross motor function (GMFCS level) in children with cerebral palsy. J Child Orthop 10(3):261–266. https://doi.org/10.1007/s11832-016-0738-4
Gunel MK et al (2009) Relationship among the Manual Ability Classification System (MACS), the Gross Motor Function Classification System (GMFCS), and the functional status (WeeFIM) in children with spastic cerebral palsy. Eur J Pediatr 168(4):477–485. https://doi.org/10.1007/s00431-008-0775-1
Loes DJ et al (2003) Analysis of MRI patterns aids prediction of progression in X-linked adrenoleukodystrophy. Neurology 61(3):369–374
Zhang H et al (2015) Fifteen novel EIF2B1-5 mutations identified in Chinese children with leukoencephalopathy with vanishing white matter and a long term follow-up. PLoS One 10(3):e0118001. https://doi.org/10.1371/journal.pone.0118001
Jansen AC et al (2008) Leucoencephalopathy with vanishing white matter may cause progressive myoclonus epilepsy. Epilepsia 49(5):910–913. https://doi.org/10.1111/j.1528-1167.2008.01542.x
Sharma S et al (2011) Vanishing white matter disease associated with ptosis and myoclonic seizures. J Child Neurol 26(3):366–368. https://doi.org/10.1177/0883073810381529
Vermeulen G et al (2005) Fright is a provoking factor in vanishing white matter disease. Ann Neurol 57(4):560–563. https://doi.org/10.1002/ana.20418
Prange H, Weber T (2011) Vanishing white matter disease: a stress-related leukodystrophy. Nervenarzt 82(10):1330–1334. https://doi.org/10.1007/s00115-011-3284-9
Kaczorowska M et al (2006) Acute fright induces onset of symptoms in vanishing white matter disease-case report. Eur J Paediatr Neurol 10(4):192–193. https://doi.org/10.1016/j.ejpn.2006.05.008
Fogli A et al (2004) The effect of genotype on the natural history of eIF2B-related leukodystrophies. Neurology 62(9):1509–1517
Alorainy IA et al (1999) Cree leukoencephalopathy: neuroimaging findings. Radiology 213(2):400–406. https://doi.org/10.1148/radiology.213.2.r99oc28400
Fogli A et al (2002) Cree leukoencephalopathy and CACH/VWM disease are allelic at the EIF2B5 locus. Ann Neurol 52(4):506–510. https://doi.org/10.1002/ana.10339
Labauge P et al (2007) CACH/VWM syndrome and leucodystrophies related to EIF2B mutations. Rev Neurol (Paris) 163(8–9):793–799
van der Lei HD et al (2012) Characteristics of early MRI in children and adolescents with vanishing white matter. Neuropediatrics 43(1):22–26. https://doi.org/10.1055/s-0032-1307456
Bugiani M et al (2011) Defective glial maturation in vanishing white matter disease. J Neuropathol Exp Neurol 70(1):69–82. https://doi.org/10.1097/NEN.0b013e318203ae74
Wong K et al (2000) Foamy cells with oligodendroglial phenotype in childhood ataxia with diffuse central nervous system hypomyelination syndrome. Acta Neuropathol 100(6):635–646
Van Haren K et al (2004) The life and death of oligodendrocytes in vanishing white matter disease. J Neuropathol Exp Neurol 63(6):618–630
Huber T et al (2017) Automated segmentation reveals silent radiographic progression in adult-onset vanishing white-matter disease. Neuroradiol J 30(1):5–9. https://doi.org/10.1177/1971400916678222
Lutsep HL et al (1997) Clinical utility of diffusion-weighted magnetic resonance imaging in the assessment of ischemic stroke. Ann Neurol 41(5):574–580. https://doi.org/10.1002/ana.410410505
Schaefer PW (2001) Applications of DWI in clinical neurology. J Neurol Sci 186(Suppl 1):S25–S35
Romano A et al (2003) Diffusion-weighted MR imaging: clinical applications in neuroradiology. Radiol Med 106(5–6):521–548
Karaarslan E, Arslan A (2008) Diffusion weighted MR imaging in non-infarct lesions of the brain. Eur J Radiol 65(3):402–416. https://doi.org/10.1016/j.ejrad.2007.04.023
Bhatt A et al (2009) Diffusion-weighted imaging: not all that glitters is gold. South Med J 102(9):923–928. https://doi.org/10.1097/SMJ.0b013e3181a9142a
Le Bihan D et al (1986) MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 161(2):401–407. https://doi.org/10.1148/radiology.161.2.3763909
Patay Z (2005) Diffusion-weighted MR imaging in leukodystrophies. Eur Radiol 15(11):2284–2303. https://doi.org/10.1007/s00330-005-2846-2
Hanefeld F et al (1993) Diffuse white matter disease in three children: an encephalopathy with unique features on magnetic resonance imaging and proton magnetic resonance spectroscopy. Neuropediatrics 24(5):244–248. https://doi.org/10.1055/s-2008-1071551
Sijens PE et al (2005) 1H chemical shift imaging, MRI, and diffusion-weighted imaging in vanishing white matter disease. Eur Radiol 15(11):2377–2379. https://doi.org/10.1007/s00330-005-2783-0
van der Lei HD et al (2012) Restricted diffusion in vanishing white matter. Arch Neurol 69(6):723–727. https://doi.org/10.1001/archneurol.2011.1658
Ding XQ et al (2012) Imaging evidence of early brain tissue degeneration in patients with vanishing white matter disease: a multimodal MR study. J Magn Reson Imaging 35(4):926–932. https://doi.org/10.1002/jmri.23517
Acknowledgements
This study was supported by Beijing key laboratory (BZ0317), the National Key Research and Development Program of China (Nos. 2016YFC0901505, 2016YFC1306201), and the Public Foundation of Beijing Center of Neural Regeneration and Repair.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no financial or other conflicts of interest.
Ethical standards
This study was approved by the clinical research ethics committee of Peking University First Hospital, and informed consent forms were signed by the parents.
Rights and permissions
About this article
Cite this article
Zhou, L., Zhang, H., Chen, N. et al. Similarities and differences between infantile and early childhood onset vanishing white matter disease. J Neurol 265, 1410–1418 (2018). https://doi.org/10.1007/s00415-018-8851-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8851-6