Abstract
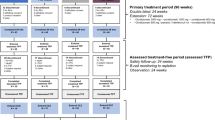
The phase III placebo-controlled BRAVO study assessed laquinimod effects in patients with relapsing-remitting MS (RRMS), and descriptively compared laquinimod with interferon beta (IFNβ)-1a (Avonex® reference arm). RRMS patients age 18–55 years with Expanded Disability Status Scale (EDSS) scores of 0–5.5 and documented pre-study relapse (≥ 1 in previous year, 2 in previous 2 years, or 1 in previous 1–2 years and ≥ 1 GdE lesion in the previous year) were randomized (1:1:1) to laquinimod 0.6 mg once-daily, matching oral placebo, or IFNβ-1a IM 30 μg once-weekly (rater-blinded design), for 24 months. The primary endpoint was annualized relapse rate (ARR); secondary endpoints included percent brain volume change (PBVC) and 3-month confirmed disability worsening. In all, 1,331 patients were randomized: laquinimod (n = 434), placebo (n = 450), and IFNβ-1a (n = 447). ARR was not significantly reduced with laquinimod [−18 %, risk ratio (RR) = 0.82, 95 % CI 0.66–1.02; p = 0.075] vs. placebo. Laquinimod significantly reduced PBVC (28 %, p < 0.001). Confirmed disability worsening was infrequent (10 % laquinimod, 13 % placebo). The change in confirmed disability worsening with laquinimod measured using EDSS was −31 % [hazard ratio (HR) 0.69, p = 0.063], and using Multiple Sclerosis Functional Composite (MSFC) z-score was −77 % (p = 0.150), vs. placebo. IFNβ-1a reduced ARR 26 % (RR = 0.74, 95 % CI 0.60–0.92, p = 0.007), showed no effect on PBVC loss (+11 %, p = 0.14), and changes in disability worsening were −26 and −66 % as measured using the EDSS (HR 0.742, p = 0.13) and MSFC (p = 0.208), respectively. Adverse events occurred in 75, 82, and 70 % of laquinimod, IFNβ-1a, and placebo patients, respectively. Once-daily oral laquinimod 0.6 mg resulted in statistically nonsignificant reductions in ARR and disability progression, but significant reductions in brain atrophy vs. placebo. Laquinimod was well-tolerated.



Similar content being viewed by others
References
Avonex® (interferon beta-1a) prescribing information (2013) Biogen Idec, Inc, Cambridge, MA, USA. Rev 03/2013
Agosta F, Rovaris M, Pagani E, Sormani MP, Comi G, Filippi M (2006) Magnetization transfer MRI metrics predict the accumulation of disability 8 years later in patients with multiple sclerosis. Brain 129:2620–2627
Bruck W, Pfortner R, Pham T, Zhang J, Hayardeny L, Piryatinsky V, Hanisch UK, Regen T, van Rossum D, Brakelmann L, Hagemeier K, Kuhlmann T, Stadelmann C, John GR, Kramann N, Wegner C (2012) Reduced astrocytic NF-kappaB activation by laquinimod protects from cuprizone-induced demyelination. Acta Neuropathol 124:411–424
Bruck W, Wegner C (2011) Insight into the mechanism of laquinimod action. J Neurol Sci 306:173–179
Cohen BA, Rieckmann P (2007) Emerging oral therapies for multiple sclerosis. Int J Clin Pract 61:1922–1930
Cohen JA, Reingold SC, Polman CH, Wolinsky JS (2012) Disability outcome measures in multiple sclerosis clinical trials: current status and future prospects. Lancet Neurol 11:467–476
Comi G, Jeffery D, Kappos L, Montalban X, Boyko A, Rocca M, Filippi M, ALLEGRO Study Group (2012) Placebo-controlled trial of oral laquinimod in multiple sclerosis. N Engl J Med 366:1000–1009
Comi G, Obramsky O, Arbizu T, Boyko AN, Gold R, Havrdova E, Komoly S, Mesaros S, Selmaj K, Sharrack B, Filippi M (2009) Long-term open extension of oral laquinimod in patients with relapsing multiple sclerosis shows favourable safety and sustained low relapse rate and MRI activity. Mult Scler 15(suppl2):S127. Abstract P443
Comi G, Pulizzi A, Rovaris M, Abramsky O, Arbizu T, Boiko A, Gold R, Havrdova E, Komoly S, Selmaj K, Sharrack B, Filippi M (2008) Effect of laquinimod on MRI-monitored disease activity in patients with relapsing-remitting multiple sclerosis: a multicentre, randomised, double-blind, placebo-controlled phase IIb study. Lancet 371:2085–2092
Cutter GR, Baier ML, Rudick RA, Cookfair DL, Fischer JS, Petkau J, Syndulko K, Weinshenker BG, Antel JP, Confavreux C, Ellison GW, Lublin F, Miller AE, Rao SM, Reingold S, Thompson A, Willoughby E (1999) Development of a multiple sclerosis functional composite as a clinical trial outcome measure. Brain 122(Pt 5):871–882
European Medicines Agency-Committee for Medicinal Products for Human Use (CHMP) (2006) Guideline on clinical investigation of medicinal products for the treatment of multiple sclerosis. London
Fisher E, Lee JC, Nakamura K, Rudick RA (2008) Gray matter atrophy in multiple sclerosis: a longitudinal study. Ann Neurol 64:255–265
Fox RJ, Miller DH, Phillips JT, Hutchinson M, Havrdova E, Kita M, Yang M, Raghupathi K, Novas M, Sweetser MT, Viglietta V, Dawson KT (2012) Placebo-controlled phase 3 study of oral BG-12 or glatiramer in multiple sclerosis. N Engl J Med 367:1087–1097
Gold R, Kappos L, Arnold DL, Bar-Or A, Giovannoni G, Selmaj K, Tornatore C, Sweetser MT, Yang M, Sheikh SI, Dawson KT (2012) Placebo-controlled phase 3 study of oral BG-12 for relapsing multiple sclerosis. N Engl J Med 367:1098–1107
Jacobs LD, Cookfair DL, Rudick RA, Herndon RM, Richert JR, Salazar AM, Fischer JS, Goodkin DE, Granger CV, Simon JH, Alam JJ, Bartoszak DM, Bourdette DN, Braiman J, Brownscheidle CM, Coats ME, Cohan SL, Dougherty DS, Kinkel RP, Mass MK, Munschauer FE III, Priore RL, Pullicino PM, Scherokman BJ, Whitham RH (1996) Intramuscular interferon beta-1a for disease progression in relapsing multiple sclerosis. The multiple sclerosis collaborative research group (MSCRG). Ann Neurol 39:285–294
Johnson KP (2010) Risks vs benefits of glatiramer acetate: a changing perspective as new therapies emerge for multiple sclerosis. Ther Clin Risk Manag 6:153–172
Kappos L, Radue EW, O’Connor P, Polman C, Hohlfeld R, Calabresi P, Selmaj K, Agoropoulou C, Leyk M, Zhang-Auberson L, Burtin P (2010) A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N Engl J Med 362:387–401
Kieseier BC (2011) The mechanism of action of interferon-beta in relapsing multiple sclerosis. CNS Drugs 25:491–502
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33:1444–1452
Mishra MK, Wang J, Silva C, Mack M, Yong VW (2012) Kinetics of proinflammatory monocytes in a model of multiple sclerosis and its perturbation by laquinimod. Am J Pathol 181:642–651
O’Connor P, Filippi M, Arnason B, Comi G, Cook S, Goodin D, Hartung HP, Jeffery D, Kappos L, Boateng F, Filippov V, Groth M, Knappertz V, Kraus C, Sandbrink R, Pohl C, Bogumil T, O’Connor P, Filippi M, Arnason B, Cook S, Goodin D, Harung HP, Kappos L, Jeffery D, Comi G (2009) 250 microg or 500 microg interferon beta-1b versus 20 mg glatiramer acetate in relapsing-remitting multiple sclerosis: a prospective, randomised, multicentre study. Lancet Neurol 8:889–897
O’Connor P, Wolinsky JS, Confavreux C, Comi G, Kappos L, Olsson TP, Benzerdjeb H, Truffinet P, Wang L, Miller A, Freedman MS (2011) Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N Engl J Med 365:1293–1303
Polman C, Barkhof F, Sandberg-Wollheim M, Linde A, Nordle O, Nederman T (2005) Treatment with laquinimod reduces development of active MRI lesions in relapsing MS. Neurology 64:987–991
Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, Lublin FD, Metz LM, McFarland HF, O’Connor PW, Sandberg-Wollheim M, Thompson AJ, Weinshenker BG, Wolinsky JS (2005) Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol 58:840–846
Popescu BF, Lucchinetti CF (2012) Pathology of demyelinating diseases. Annu Rev Pathol 7:185–217
Reuben A (2004) Hy’s law. Hepatology 39:574–578
Rudick RAM, Fisher EP, Lee J-CM, Simon JMP, Jacobs LM, the Multiple Sclerosis Collaborative Research Group (1999) Use of the brain parenchymal fraction to measure whole brain atrophy in relapsing-remitting MS. Neurology 53:1698–1704
Schulze-Topphoff U, Shetty A, Varrin-Doyer M, Molnarfi N, Sagan SA, Sobel RA, Nelson PA, Zamvil SS (2012) Laquinimod, a quinoline-3-carboxamide, induces type II myeloid cells that modulate central nervous system autoimmunity. PLoS One 7:e33797
Thone J, Gold R (2011) Laquinimod: a promising oral medication for the treatment of relapsing-remitting multiple sclerosis. Expert Opin Drug Metab Toxicol 7:365–370
Wegner C, Stadelmann C, Pfortner R, Raymond E, Feigelson S, Alon R, Timan B, Hayardeny L, Bruck W (2010) Laquinimod interferes with migratory capacity of T cells and reduces IL-17 levels, inflammatory demyelination and acute axonal damage in mice with experimental autoimmune encephalomyelitis. J Neuroimmunol 227:133–143
Wei L, Zhang J (2001) Analysis of data with imbalance in the baseline outcome variable for randomized clinical trials. Drug Inf J 35:1201–1214
Whitaker JN, McFarland HF, Rudge P, Reingold SC (1995) Outcomes assessment in multiple sclerosis clinical trials: a critical analysis. Mult Scler 1:37–47
Zipp F, Aktas O (2006) The brain as a target of inflammation: common pathways link inflammatory and neurodegenerative diseases. Trends Neurosci 29:518–527
Acknowledgments
We thank the Independent Data Monitoring Committee, the staff of NeuroRx Research, the MRI Analysis Center, and the Principal Investigators for each country; Yulia Sidi, M.A. of the Teva Statistical Data Management Team (Netanya, Israel) managed the statistical analyses; Pippa Loupe, Ph.D. of Medical Affairs, Teva Pharmaceuticals (Kansas City, MO), and two independent medical writers, paid by the sponsor, James D. Bergstrom, Ph.D. of Mountain Stream Communications, LLC (Hillsborough, NJ), and Sheila Truten, B.S. of Medical Communication Company (Wynnewood, PA) collaborated with the authors on the first draft of the paper, copyedited the manuscript and prepared figures and tables.
Supported by Teva Pharmaceutical Industries, Ltd., Petach Tikva, Israel.
Conflicts of interest
TL Vollmer has received consulting fees, and his institution has received a grant and consulting fee for his participation in the BRAVO study; he is a board member of Rocky Mountain MS Center; his institution has received consultancy fees from Biogen Idec, Teva, Elan, Hoffman-LaRoche, Accelerated Cure Project, Genzyme, Bristol-Myers Squibb, Acorda, Novartis, Questor, Medscape, Xenoport, and Sanofi; his institution received fees for expert testimony from Ham VS Bennett and Wagner VS Strand; his institution received grants/grants pending from Teva, Biogen Idec, Genzyme, Ono, Eli Lilly, Novartis, BioMS, Orasi, Sanofi-Aventis, NIH, EMD Sorono, Acorda, Accelerated Cure Project, Hoffmann-LaRoche, Jensen Research, Daiichi Sankyo, Elan, Janssen Pharmaceutical, Avanir Pharmaceutical, MedImmune, Delta Quest, Biosite Inc., University of Alabama, and Genentech.
PS Sorensen has received payment as co-principal investigator and for travel support for the BRAVO study from Teva; he has received consultancy fees from Merck Serono, Teva, Novartis, Sanofi-Aventis, and Biogen Idec; his institution has received research support grants/grants pending from Biogen Idec, Novartis, and Sanofi-Aventis; and he is on the speaker’s bureau of Merck Serono, Novartis, Bayer Schering, Teva, Sanofi-Aventis, Biogen Idec, and Genzyme.
K Selmaj has received compensation for consulting and speaking from Biogen Idec, Genzyme, Novartis, Merck Serono, Roche, and Teva.
F Zipp’s institution received a grant from Teva for participation in BRAVO and has received grants/grants pending from Novartis and Merck Serono; she has received fees for consultancy with Merck-Serono, Ono, Sanofi-Aventis, and Biogen; she is a board member of Octapharma; and serves on the speaker’s bureau of Novartis, Merck-Serono, Biogen, Genzyme, and Sanofi-Aventis.
E Havrdova’s institution received funding for clinical trial participation, she has received compensation for consultancy from Biogen Idec, Genzyme, Merck Serono, and Novartis; serves on the speaker’s bureaus of Biogen Idec, Merck Serono, Novartis, and Teva; her institution has received a grant/grant pending from Biogen Idec.
JA Cohen received, in the previous 2 years, compensation for consulting from Teva and Vaccinex; his institution received research support from Biogen Idec, Novartis, Receptos, Synthon, Teva, US Department of Defense, National Institutes of Health, and National MS Society.
N Sasson is employed by Teva; owns stock in and receives travel/meeting expenses from Teva.
Y Gilgun-Sherki is employed by Teva; owns stock in and receives travel/meeting expenses from Teva; and is a co-holder of patents with Teva.
D Arnold has received fees for consulting, travel support, and research related to the BRAVO study; has received consultancy fees from Biogen Idec, EMD Serono, Genentech, Glaxo Smith Kline, Merck Serono, Mitsubishi, Novartis, and Roche; his institution has received grants/grants pending from Bayer Healthcare, CIHR, and MSSC and owns US patent No. 6,347,239.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
T. L. Vollmer and P. S. Sorensen were co-principal investigators for the BRAVO trial, contributed equally to the manuscript, and should be considered equal lead authors on this publication.
N. Sasson of Teva Pharmaceutical Industries provided statistical support for the manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vollmer, T.L., Sorensen, P.S., Selmaj, K. et al. A randomized placebo-controlled phase III trial of oral laquinimod for multiple sclerosis. J Neurol 261, 773–783 (2014). https://doi.org/10.1007/s00415-014-7264-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7264-4