Abstract
Background
Bilateral pallidal lesions induce a range of cognitive and motor disorders, principally a parkinsonian syndrome in which severe disturbances of gait and gait initiation are frequently reported. However, the precise clinical features of these disorders (and the role of the pallidum therein) remain to be established.
Objectives
The goal of this study was to characterise gait and gait initiation disorders within the context of a parkinsonian syndrome in patients with acquired, bilateral, pallidal lesions (PAL patients), to compare these disorders to those seen in Parkinson’s disease (PD), and to assess the corresponding physiopathological implications.
Patients and methods
By using a video motion analysis system (VICON), we studied gait kinematic parameters in two patients presenting with bilateral, pallidal lesions. Kinematic and kinetic parameters were also determined during gait initiation. The two patients were compared with a group of 17 PD patients and to 20 healthy controls.
Results
In both PAL and PD patients, kinematic parameters (gait and gait initiation) and kinetic parameters (gait initiation) were similarly impaired, evidenced by akinesia (difficulty in initiating gait characterized by impairment of anticipatory postural adjustments). Hypokinesia and bradykinesia (respectively reduced stride length and reduced speed during gait) were also noted.
Conclusion
The gait and gait initiation disorders seen in cases of bilateral pallidal lesions (namely akinesia, hypokinesia and bradykinesia) are similar to those observed in PD. Subject to confirmation in more extensive studies, we hypothesize that bipallidal patients may present higher level gait disorders,with potential mediation by cognitive impairment.
Similar content being viewed by others
References
Jellinger K (1986) Exogenous lesion of the pallidum in Handbook of Clinical Neurology. In:Vinken GWBPJ, Klawans, HL (eds) Elsevier science publishers: Amsterdam, pp 465–491
Klawans HL, Stein RW, Tanner CM, Goetz CG (1982) A pure Parkinsonian syndrome following acute carbon monoxide intoxicatin. Arch Neurol 39:302–304
Carella F, Grassi MP, Savoiardo M, Contri P, Rapuzzi B, Mangoni A (1988) Dystonic–parkinsonian syndrome after cyanide poisoning: clinical and MRI findings. J Neurol Neurosurg Psychiatry 51:1345–1348
Fève AP, Fénelon G, Wallays C, Rémy P, Guillard A (1993) Axial motor disturbances after hypoxic lesions of the globus pallidus. Mov Disord 8:321–326
Benassi G, Rinaldi R, Azzimondi G, Stracciari A, D’Allessandro R, Pazzaglia P (1996) Acute generalized dystonia due to bilateral lesion of basal ganglia mainly affecting the nuclei pallidi. Ital J Neurol Sci 17:71–73
Schoser BGH, Groden C (1999) Subacute onset of oculogyric crises and generalized dystonia following intranasal administration of heroin. Addiction 94:431–434
Hawker K, Lang AE (1990) Hypotoxicischemic damage of the basal ganglia. Mov Disord 5:219–224
Haaxma R, Van Boxtel A, Brouwer WH, et al. (1995) Motor function in patient with bilateral lesions of the globus pallidus. Mov Disord 10:761–777
Laplane D, Baulac M, Pillon B, Panayotopoulou– Achimastos (1982) Perte de l’auto–activation psychique, activité compulsive d’allure obsessionnelle. Lésion lenticulaire bilatérale. Rev Neurol (Paris) 138:173–141
Laplane D, Dubois B (1998) Les troubles affectifs de la perte d’auto–activation psychique. comparaison avec ceux de l’athymhormie. Rev Neurol (Paris) 154:35–39
Ali–Cherif A, Royere ML, Gosset A, Poncet M, Salamon G, Khalil R (1984) Behavior and mental activity disorders after carbon monoxide poisoning. Bilateral pallidal lesions. Rev Neurol (Paris) 140:401–405
Stuss DT, Van Reekum R, Murphy KJ (2000) Differentiation of states and causes of apathy. In: Borod J (ed) The neuropsychology of emotion. New York, Oxford University Press, pp 340–363
Knutsson E (1972) An analysis of parkinsonian gait. Brain 95:475–486
Stern GM, Franklyn SE, Imms FJ, Prestidge SP (1983) Quantitative assessments of gait and mobility in Parkinson’s disease. J Neural Trans 19:202–214
Blin O, Fernandez AM, Serratrice G (1990) Quantitative analysis of gait in Parkinson’s patients: increased variability of stride lenght. Neurol Sci 98:91–97
Burleigh–Jacobs A, Horak FB, Nutt GJ, Obeso JA (1997) Step Initiation in Parkinson’s Disease: Influence of Levodopa and External Sensory Triggers. Mov Disord 12:206–215
Krystkowiak P, Blatt JL, Bourriez JL, Duhamel A, Perina M, Kemoun G, Blond S, Guieu JD, Destée A, Defebvre L (2001) Chronic bilateral pallidal stimulation and levodopa do not improve gait in the same way in Parkinson’s disease: a study using a video motion analysis system. J Neurol 248:944–949
Krystkowiak P, Blatt JL, Bourriez JL, Duhamel A, Perina M, Blond S, Guieu JD, Destée A, Defebvre L (2003) Effects of subthalamic nucleus stimulation and levodopa treatment on gait troubles in Parkinson’s disease. Arch Neurol 60:80–84
Fahn S, Elton RL, and members of the UPDRS Development Committee (1987) Unified Idiopathic Parkinson’s Disease Rating Scale. In: Fahn S, Marsden CD, Calne D, Goldstein M (eds) Recent Developments in Parkinson’s Disease. Florham Park, NJ: MacMillan Healthcare Information 2: pp 153–164
Folstein MF, Folstein SE, McHugh PR (1975) Mini–Mental State: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Mattis S Mental status examination for organic mental syndrome in the ederly patient (1976) In: Bellack L, Karasu TB (eds) Geriatric Psychiatry. New York: Grune and Stratton, pp 77–121
Dubois B, Slachevsky A, Litvan I, Pillon B (2000) The FAB: A frontal Assessment Battery at bedside. Neurology 55:1621–1626
Montgomery SA, Åsberg M (1979) A new depression scale designed to be sensitive to change. Br J Psychiatry 134:322–389
Gibb WRG, Lees AJ (1988) The prevalence of the lewy body to the pathogenesis of idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry 51:745–752
Elble R, Moody C, Leffler K, Sinha R (1994) The initiation of normal walking. Mov Disord 9:139–146
Shik ML (1986) An hypothesis on the bulbospinal locomotor column. Wenner–Gren International Symposium Series 45:39–49
Garcia–Rill E (1986) The basal ganglia and the locomotor region. Brain Res Rev 11:47–63
Pahapill PA, Lozano AM (2000) The pedunculopontine nucleus and Parkinson’s disease. Brain 123:1767–1783
Nutt JG, Marsden CD, Thompson PD (1993) Human walking and higherlevel gait disorders, particularly in the elderly. Neurology 43:268–279
Nakamura T, Meguro K, Yamazaki H, Okuzumi H, Tanaka A, Horikawa A, Yamaguchi K, Katsuyama N, Nakano M, Arai H, Sasaki H (1997) Postural and gait disturbance correlated with decreased frontal cerebral blood flow in Alzheimer disease. Alzheimer Dis Assoc Disord 11:132–139
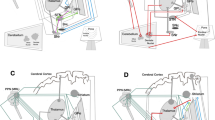
Alexander GE, Crutcher MD (1990) Functional architecture of basal ganglia circuits: neural substrates of parallel processing. TINS 13:266–271
Joël D (2001) Open interconnected model of basal ganglia–thalamocortical circuitry and its relevance to the clinical syndrome of Huntington’s disease. Mov Disord 16:407–423
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krystkowiak, P., Delval, A., Dujardin, K. et al. Gait abnormalities induced by acquired bilateral pallidal lesions. J Neurol 253, 594–600 (2006). https://doi.org/10.1007/s00415-006-0066-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-006-0066-6