Abstract
Purpose
Northern Territory (NT)-based clinical service data suggest substantial lung function impairment amongst First Nations adults as young as 18–40 years. Our objectives were to describe the burden of disease and lung function of adults living in regional-remote Queensland, identify determinants of lung function, and evaluate the impact of a specialist respiratory outreach service on lung function.
Methods
Retrospective 8-year cohort study (February 2012–March 2020) of 1113 First Nations Australian adults (and 648 non-First Nations adults) referred to respiratory outreach clinics in regional-remote Queensland.
Results
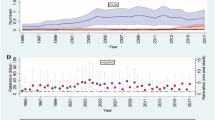
In the combined cohort, the forced expiratory volume in 1 s (FEV1) was clinically abnormal for 54% of First Nations patients (51% of non-First Nations patients), forced vital capacity (FVC) for 46% (36%), FEV1/FVC% for 30% (36%), and gas diffusing capacity (DLCO) for 44% (37%). A respiratory diagnosis was assigned by a respiratory physician in 78% of First Nations (76% non-First Nations) patients. Smoking, household smoke exposure, underweight BMI, and respiratory disease were associated with reduced lung function. In the 40% of patients (709/1765) followed up, FEV1 and FVC significantly improved (mean change: zFEV1 = 0.15 [95% CI 0.10–0.20]; zFVC = 0.25 [0.20, 0.31]), and FEV1/FVC% significantly reduced (mean = − 0.10 [95%CI − 0.07 to − 0.03]), with no significant change in DLCO. Patients with COPD had lower FEV1 improvement, whilst underweight and obese patients had lower FVC improvement.
Conclusion
Regional-remote First Nations adult Queenslanders have higher lung function than previously reported, with no lung function decline observed at follow-up visit, including for those with respiratory disease.

Similar content being viewed by others
References
Australian Institute of Health and Welfare. Australia’s health 2018. Canberra; 2018.
Australian Institute of Health and Welfare. Rural & remote health. Canberra; 2017.
Australian Health Ministers’ Advisory Council. Aboriginal and Torres Strait Islander Health Performance Framework 2017 Report. Canberra; 2017.
O’Grady KA, Hall KK, Bell A et al (2018) Review of respiratory disease among Aboriginal and Torres Strait Islander children. Austral Indigenous HealthBull 18(2):1–32
Bailey EJ, Kruske SG, Morris PS et al (2008) Culture-specific programs for children and adults from minority groups who have asthma. Cochrane Database Syst Rev. 2:CD006580. https://doi.org/10.1002/14651858.CD006580.pub2
Medlin LG, Chang AB, Fong K et al (2014) Indigenous Respiratory Outreach Care: the first 18 months of a specialist respiratory outreach service to rural and remote Indigenous communities in Queensland. Australia Aust Health Rev 38(4):447–453. https://doi.org/10.1071/AH13136
Collaro AJ, Chang AB, Marchant JM et al (2020) Culturally appropriate outreach specialist respiratory medical care improves the lung function of children in regional and remote Queensland. Lung 198(2):361–369. https://doi.org/10.1007/s00408-020-00332-7
Collaro AJ, Chang AB, Marchant JM et al (2020) Pediatric patients of outreach specialist Queensland clinics have lung function improvement comparable to that of tertiary pediatric patients. Chest 158(4):1566–1575. https://doi.org/10.1016/j.chest.2020.03.084
Australian Housing and Urban Research Institute (2006) Indigenous mobility in rural and remote Australia. Queensland Research Centre: Australian Housing and Urban Research Institute, Weipa
Thompson BR, Stanojevic S, Abramson MJ et al (2011) The all-age spirometry reference ranges reflect contemporary Australasian spirometry. Respirology 16(6):912–917. https://doi.org/10.1111/j.1440-1843.2011.01970.x
Graham BL, Steenbruggen I, Miller MR et al (2019) Standardization of spirometry 2019 update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 200(8):e70–e88. https://doi.org/10.1164/rccm.201908-1590ST
Graham BL, Brusasco V, Burgos F et al (2017) 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J. https://doi.org/10.1183/13993003.00016-2016
Duong M, Islam S, Rangarajan S et al (2019) Mortality and cardiovascular and respiratory morbidity in individuals with impaired FEV1 (PURE): an international, community-based cohort study. Lancet Glob Health 7(5):e613–e623. https://doi.org/10.1016/S2214-109X(19)30070-1
Schubert J, Kruavit A, Mehra S et al (2019) Prevalence and nature of lung function abnormalities among Indigenous Australians referred to specialist respiratory outreach clinics in the Northern Territory. Intern Med J 49(2):217–224. https://doi.org/10.1111/imj.14112
Blackall SR, Hong JB, King P et al (2018) Bronchiectasis in indigenous and non-indigenous residents of Australia and New Zealand. Respirology 23(8):743–749. https://doi.org/10.1111/resp.13280
Heraganahally SS, Wasgewatta SL, McNamara K et al (2019) Chronic obstructive pulmonary disease in aboriginal patients of the Northern Territory of Australia: a landscape perspective. Int J Chron Obstruct Pulmon Dis 14:2205–2217. https://doi.org/10.2147/COPD.S213947
Quanjer PH, Stanojevic S, Cole TJ et al (2012) Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 40(6):1324–1343. https://doi.org/10.1183/09031936.00080312
Stanojevic S, Graham BL, Cooper BG et al (2017) Official ERS technical standards: Global Lung Function Initiative reference values for the carbon monoxide transfer factor for Caucasians. Eur Respir J. https://doi.org/10.1183/13993003.00010-2017
"Official ERS technical standards: Global Lung Function Initiative reference values for the carbon monoxide transfer factor for Caucasians." Sanja Stanojevic, Brian L. Graham, Brendan G. Cooper, Bruce R. Thompson, Kim W. Carter, Richard W. Francis and Graham L. Hall on behalf of the Global Lung Function Initiative T LCO working group. Eur Respir J 2017; 50: 1700010. Eur Respir J. 2020;56(4). https://doi.org/10.1183/13993003.50010-2017
Miller A, Thornton JC, Warshaw R et al (1983) Single breath diffusing capacity in a representative sample of the population of Michigan, a large industrial state. Predicted values, lower limits of normal, and frequencies of abnormality by smoking history. Am Rev Respir Dis. 127(3):270–277. https://doi.org/10.1164/arrd.1983.127.3.270
Blake TL, Chang AB, Chatfield MD et al (2020) Global Lung Function Initiative-2012 “other/mixed” spirometry reference equation provides the best overall fit for Australian Aboriginal and/or Torres Strait Islander children and young adults. Respirology 25(3):281–288. https://doi.org/10.1111/resp.13649
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of COPD (2020 report). 2020.
Hankinson JL, Odencrantz JR, Fedan KB (1999) Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med 159(1):179–187. https://doi.org/10.1164/ajrccm.159.1.9712108
Sin DD, Wu L, Man SF (2005) The relationship between reduced lung function and cardiovascular mortality: a population-based study and a systematic review of the literature. Chest 127(6):1952–1959. https://doi.org/10.1378/chest.127.6.1952
Acknowledgements
We acknowledge and thank the First Nations Health Workers, First Nations project officers, doctors, nurses, and clinical measurements scientists on the IROC program for their tireless efforts. AJC is supported by a National Health and Medical Research Council (NHMRC) Postgraduate Scholarship (APP2003334). JM is supported by a Queensland Children’s Hospital Foundation (CHF) Fellowship (RPC0772019). AC is supported by a (NHMRC) Senior Practitioner Fellowship (APP1154302) and CHF top-up (#50286).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Collaro, A.J., Chang, A.B., Marchant, J.M. et al. Determinants and Follow-up of Lung Function Data from a Predominantly First Nations Cohort of Adults Referred to Specialist Respiratory Outreach Clinics in Regional and Remote Queensland. Lung 199, 417–425 (2021). https://doi.org/10.1007/s00408-021-00453-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-021-00453-7