Abstract
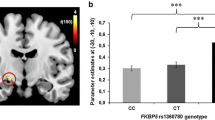
Childhood trauma is a risk factor for psychotic and mood disorders that is associated with abnormal hypothalamic–pituitary–adrenal (HPA) axis function in response to stress and abnormal social brain function. Here, we aimed to determine whether childhood trauma exposure would differently moderate associations between cortisol reactivity and social brain function, among cases with schizophrenia (SZ), bipolar disorder (BD) and in healthy individuals (HC). Forty cases with SZ, 35 with BD and 34 HCs underwent functional magnetic resonance imaging while performing an emotional face-matching task. Participants completed the Childhood Trauma Questionnaire and cortisol reactivity (i.e. the slope indexing the within-subject difference between pre- and post-imaging salivary cortisol levels) was determined. The severity of childhood trauma moderated the relationship between cortisol reactivity and brain activation in the bilateral temporo-parieto-insular junctions, right middle cingulum, right pre/postcentral gyri, left cerebellum and right lingual gyrus, differently depending on the clinical group. When exposed to high levels of trauma, the cortisol slope was negatively associated with activation in these regions in HC, while the cortisol slope was positively associated with activation in these regions in SZ cases. Similarly, there were differences between the groups in how trauma severity moderated the relationship between cortisol reactivity and functional connectivity between the amygdala and dorsolateral prefrontal cortex. In addition to reflecting typical associations between cortisol reactivity and emotional brain function when not exposed to childhood trauma, these findings provide new evidence that trauma exposure disrupts these relationships in both healthy individuals and in cases with SZ or BD.




Similar content being viewed by others
References
Green MJ, Girshkin L, Teroganova N, Quidé Y (2014) Stress, schizophrenia and bipolar disorder. Curr Top Behav Neurosci 18:217–235. https://doi.org/10.1007/7854_2014_290
Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Read J, van Os J, Bentall RP (2012) Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull 38(4):661–671. https://doi.org/10.1093/schbul/sbs050
Dannlowski U, Stuhrmann A, Beutelmann V, Zwanzger P, Lenzen T, Grotegerd D, Domschke K, Hohoff C, Ohrmann P, Bauer J, Lindner C, Postert C, Konrad C, Arolt V, Heindel W, Suslow T, Kugel H (2012) Limbic scars: long-term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biol Psychiatr 71(4):286–293. https://doi.org/10.1016/j.biopsych.2011.10.021
van Harmelen AL, van Tol MJ, Dalgleish T, van der Wee NJ, Veltman DJ, Aleman A, Spinhoven P, Penninx BW, Elzinga BM (2014) Hypoactive medial prefrontal cortex functioning in adults reporting childhood emotional maltreatment. Soc Cogn Affect Neurosci 9(12):2026–2033. https://doi.org/10.1093/scan/nsu008
Barker V, Gumley A, Schwannauer M, Lawrie SM (2015) An integrated biopsychosocial model of childhood maltreatment and psychosis. Br J Psychiatry 206(3):177–180. https://doi.org/10.1192/bjp.bp.113.143578
Myin-Germeys I, van Os J (2007) Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev 27(4):409–424. https://doi.org/10.1016/j.cpr.2006.09.005
Lardinois M, Lataster T, Mengelers R, Van Os J, Myin-Germeys I (2011) Childhood trauma and increased stress sensitivity in psychosis. Acta Psychiatr Scand 123(1):28–35. https://doi.org/10.1111/j.1600-0447.2010.01594.x
Liu Y, Zhang D, Zhao Y, Tan S, Luo Y (2016) Deficits in attentional processing of fearful facial expressions in schizophrenic patients. Sci Rep 6:32594. https://doi.org/10.1038/srep32594
Girshkin L, Matheson SL, Shepherd AM, Green MJ (2014) Morning cortisol levels in schizophrenia and bipolar disorder: a meta-analysis. Psychoneuroendocrino 49:187–206. https://doi.org/10.1016/j.psyneuen.2014.07.013
Ciufolini S, Dazzan P, Kempton MJ, Pariante C, Mondelli V (2014) HPA axis response to social stress is attenuated in schizophrenia but normal in depression: evidence from a meta-analysis of existing studies. Neurosci Biobehav Rev 47:359–368. https://doi.org/10.1016/j.neubiorev.2014.09.004
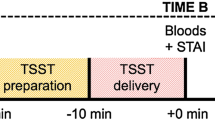
Girshkin L, O’Reilly N, Quidé Y, Teroganova N, Rowland JE, Schofield PR, Green MJ (2016) Diurnal cortisol variation and cortisol response to an MRI stressor in schizophrenia and bipolar disorder. Psychoneuroendocrino 67:61–69. https://doi.org/10.1016/j.psyneuen.2016.01.021
Pruessner M, Cullen AE, Aas M, Walker EF (2017) The neural diathesis-stress model of schizophrenia revisited: an update on recent findings considering illness stage and neurobiological and methodological complexities. Neurosci Biobehav Rev 73:191–218. https://doi.org/10.1016/j.neubiorev.2016.12.013
Berger M, Kraeuter AK, Romanik D, Malouf P, Amminger GP, Sarnyai Z (2016) Cortisol awakening response in patients with psychosis: systematic review and meta-analysis. Neurosci Biobehav Rev 68:157–166. https://doi.org/10.1016/j.neubiorev.2016.05.027
Gil-Ad I, Dickerman Z, Amdursky S, Laron Z (1986) Diurnal rhythm of plasma beta endorphin, cortisol and growth hormone in schizophrenics as compared to control subjects. Psychopharmacology 88(4):496–499. https://doi.org/10.1007/bf00178514
Cervantes P, Gelber S, Kin FN, Nair VN, Schwartz G (2001) Circadian secretion of cortisol in bipolar disorder. J Psychiatry Neurosci 26(5):411–416
Kirschbaum C, Pirke KM, Hellhammer DH (1993) The ‘trier social stress test’–a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology 28(1–2):76–81. https://doi.org/10.1159/000119004
Brenner K, Liu A, Laplante DP, Lupien S, Pruessner JC, Ciampi A, Joober R, King S (2009) Cortisol response to a psychosocial stressor in schizophrenia: blunted, delayed, or normal? Psychoneuroendocrinology 34(6):859–868. https://doi.org/10.1016/j.psyneuen.2009.01.002
Muehlhan M, Lueken U, Wittchen HU, Kirschbaum C (2011) The scanner as a stressor: evidence from subjective and neuroendocrine stress parameters in the time course of a functional magnetic resonance imaging session. Int J Psychophysiol 79(2):118–126. https://doi.org/10.1016/j.ijpsycho.2010.09.009
Peters S, Cleare AJ, Papadopoulos A, Fu CH (2011) Cortisol responses to serial MRI scans in healthy adults and in depression. Psychoneuroendocrinology 36(5):737–741. https://doi.org/10.1016/j.psyneuen.2010.10.009
Tessner KD, Walker EF, Hochman K, Hamann S (2006) Cortisol responses of healthy volunteers undergoing magnetic resonance imaging. Hum Brain Mapp 27(11):889–895. https://doi.org/10.1002/hbm.20229
Braehler C, Holowka D, Brunet A, Beaulieu S, Baptista T, Debruille JB, Walker CD, King S (2005) Diurnal cortisol in schizophrenia patients with childhood trauma. Schizophr Res 79(2–3):353–354. https://doi.org/10.1016/j.schres.2004.07.007
Ruby E, Rothman K, Corcoran C, Goetz RR, Malaspina D (2017) Influence of early trauma on features of schizophrenia. Early Interv Psychiatry 11(4):322–333. https://doi.org/10.1111/eip.12239
Faravelli C, Mansueto G, Palmieri S, Lo Sauro C, Rotella F, Pietrini F, Fioravanti G (2017) Childhood adversity, cortisol levels, and psychosis: a retrospective investigation. J Nerv Ment Dis 205(7):574–579. https://doi.org/10.1097/NMD.0000000000000699
Seidenfaden D, Knorr U, Soendergaard MG, Poulsen HE, Fink-Jensen A, Jorgensen MB, Jorgensen A (2017) The relationship between self-reported childhood adversities, adulthood psychopathology and psychological stress markers in patients with schizophrenia. Compr Psychiatry 72:48–55. https://doi.org/10.1016/j.comppsych.2016.09.009
Lange C, Huber CG, Frohlich D, Borgwardt S, Lang UE, Walter M (2017) Modulation of HPA axis response to social stress in schizophrenia by childhood trauma. Psychoneuroendocrinology 82:126–132. https://doi.org/10.1016/j.psyneuen.2017.03.027
Schreuder MM, Vinkers CH, Mesman E, Claes S, Nolen WA, Hillegers MH (2016) Childhood trauma and HPA axis functionality in offspring of bipolar parents. Psychoneuroendocrinology 74:316–323. https://doi.org/10.1016/j.psyneuen.2016.09.017
Peters AT, Van Meter A, Pruitt PJ, Briceno EM, Ryan KA, Hagan M, Weldon AL, Kassel MT, Vederman A, Zubieta JK, McInnis M, Weisenbach SL, Langenecker SA (2016) Acute cortisol reactivity attenuates engagement of fronto-parietal and striatal regions during emotion processing in negative mood disorders. Psychoneuroendocrinology 73:67–78. https://doi.org/10.1016/j.psyneuen.2016.07.215
McCrory EJ, Gerin MI, Viding E (2017) Annual Research Review: childhood maltreatment, latent vulnerability and the shift to preventative psychiatry - the contribution of functional brain imaging. J Child Psychol Psychiatry 58(4):338–357. https://doi.org/10.1111/jcpp.12713
Berens AE, Jensen SKG, Nelson CA 3rd (2017) Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Med 15(1):135. https://doi.org/10.1186/s12916-017-0895-4
Cassiers LLM, Sabbe BGC, Schmaal L, Veltman DJ, Penninx B, Van Den Eede F (2018) Structural and functional brain abnormalities associated with exposure to different childhood trauma subtypes: a systematic review of neuroimaging findings. Front Psychiatry 9:329. https://doi.org/10.3389/fpsyt.2018.00329
Herzberg MP, Gunnar MR (2020) Early life stress and brain function: activity and connectivity associated with processing emotion and reward. NeuriImage 209:116493. https://doi.org/10.1016/j.neuroimage.2019.116493
Aas M, Kauppi K, Brandt CL, Tesli M, Kaufmann T, Steen NE, Agartz I, Westlye LT, Andreassen OA, Melle I (2017) Childhood trauma is associated with increased brain responses to emotionally negative as compared with positive faces in patients with psychotic disorders. Psychol Med 47(4):669–679. https://doi.org/10.1017/S0033291716002762
Cancel A, Comte M, Boutet C, Schneider FC, Rousseau PF, Boukezzi S, Gay A, Sigaud T, Massoubre C, Berna F, Zendjidjian XY, Azorin JM, Blin O, Fakra E (2017) Childhood trauma and emotional processing circuits in schizophrenia: a functional connectivity study. Schizophr Res 184:69–72. https://doi.org/10.1016/j.schres.2016.12.003
Delvecchio G, Sugranyes G, Frangou S (2013) Evidence of diagnostic specificity in the neural correlates of facial affect processing in bipolar disorder and schizophrenia: a meta-analysis of functional imaging studies. Psychol Med 43(3):553–569. https://doi.org/10.1017/S0033291712001432
W.H.O. (2008) ICD-10: International statistical classification of diseases and related health problems, 10th edn. World Health Organization, New York
Mitchell PB, Johnston AK, Corry J, Ball JR, Malhi GS (2009) Characteristics of bipolar disorder in an Australian specialist outpatient clinic: comparison across large datasets. Aust N Z J Psychiatry 43(2):1009–1017
Loughland C, Draganic D, McCabe K, Richards J, Nasir A, Allen J, Catts S, Jablensky A, Henskens F, Michie P, Mowry B, Pantelis C, Schall U, Scott R, Tooney P, Carr V (2010) Australian Schizophrenia Research Bank: a database of comprehensive clinical, endophenotypic and genetic data for aetiological studies of schizophrenia. Aust N Z J Psychiatry 44(11):1029–1035. https://doi.org/10.3109/00048674.2010.501758
McGuffin P, Farmer A (1991) A polydiagnostic application of operational criteria in studies of psychotic illness: development and validation of the OPCRIT system. Arch Gen Psychiatry 48:764–770
Castle DJ, Jablensky A, McGrath JJ, Carr V, Morgan V, Waterreus A, Valuri G, Stain H, McGuffin P, Farmer A (2006) The diagnostic interview for psychoses (DIP): development, reliability and applications. Psychol Med 36(1):69–80
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janvas J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The mini-international neuropsychiatric interview (MINI): the development and validation of a structured diagnostic interview for DSM-IV and ICD-10. J Clin Psychiatry 59(Suppl 20):22–33
Kay SR, Opler LA, Lindenmayer J-P (1989) The positive and negative syndrome scale (PANSS): rationale and standardisation. Br J Psychiatry 155(Suppl 7):59–65
Montgomery P, Asberg B (1979) A new depression scale designed to be sensitive to change. Br J Psychiatry 134:382–389
Berk M, Malhi GS, Cahill C, Carman AC, Hadzi-Pavlovic D, Hawkins MT, Tohen M, Mitchell PB (2007) The bipolar depression rating scale (BDRS): its development, validation and utility. Bipolar Disord 9(6):571–579
Lovibond SH, Lovibond PF (1995) The DASS: manual for the depression, anxiety stress scales, 2nd edn. Psychology Foundation of Australia, Sydney
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978) A rating scale for mania: reliability, validity, and sensitivity. Br J Psychiatry 133:429–435
Bauer MS, Crits-Christoph P, Ball WA, Dewees E et al (1991) Independent assessment of manic and depressive symptoms by self-rating: scale characteristics and implications for the study of mania. Arch Gen Psychiatry 48(9):807–812
Leucht S, Wahlbeck K, Hamann J, Kissling W (2003) New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet 361(9369):1581–1589. https://doi.org/10.1016/S0140-6736(03)13306-5
Woods SW (2003) Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry 64(6):663–667
Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W (2003) Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl 27(2):169–190
Whitfield-Gabrieli S, Nieto-Castanon A (2012) Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect 2(3):125–141. https://doi.org/10.1089/brain.2012.0073
McLaren DG, Ries ML, Xu G, Johnson SC (2012) A generalized form of context-dependent psychophysiological interactions (gPPI): a comparison to standard approaches. NeuriImage 61(4):1277–1286. https://doi.org/10.1016/j.neuroimage.2012.03.068
Nashiro K, Sakaki M, Mather M (2012) Age differences in brain activity during emotion processing: reflections of age-related decline or increased emotion regulation? Gerontology 58(2):156–163. https://doi.org/10.1159/000328465
Fusar-Poli P, Placentino A, Carletti F, Landi P, Allen P, Surguladze S, Benedetti F, Abbamonte M, Gasparotti R, Barale F, Perez J, McGuire P, Politi P (2009) Functional atlas of emotional faces processing: a voxel-based meta-analysis of 105 functional magnetic resonance imaging studies. J Psychiatry Neurosci 34(6):418–432
Whittle S, Yucel M, Yap MB, Allen NB (2011) Sex differences in the neural correlates of emotion: evidence from neuroimaging. Biol Psychol 87(3):319–333. https://doi.org/10.1016/j.biopsycho.2011.05.003
Hayes AF (2017) Introduction to Mediation, Moderation, and Conditional Process Analysis, 2nd edn. Guilford Publications, A Regression-Based Approach
Craig AD (2005) Forebrain emotional asymmetry: a neuroanatomical basis? Trends Cogn Sci 9(12):566–571. https://doi.org/10.1016/j.tics.2005.10.005
Craig AD (2009) How do you feel–now? The anterior insula and human awareness. Nat Rev Neurosci 10(1):59–70. https://doi.org/10.1038/nrn2555
Berret E, Kintscher M, Palchaudhuri S, Tang W, Osypenko D, Kochubey O, Schneggenburger R (2019) Insular cortex processes aversive somatosensory information and is crucial for threat learning. Science. https://doi.org/10.1126/science.aaw0474
Livneh Y, Ramesh RN, Burgess CR, Levandowski KM, Madara JC, Fenselau H, Goldey GJ, Diaz VE, Jikomes N, Resch JM, Lowell BB, Andermann ML (2017) Homeostatic circuits selectively gate food cue responses in insular cortex. Nature 546(7660):611–616. https://doi.org/10.1038/nature22375
Torta DM, Cauda F (2011) Different functions in the cingulate cortex, a meta-analytic connectivity modeling study. NeuriImage 56(4):2157–2172. https://doi.org/10.1016/j.neuroimage.2011.03.066
De Bellis MD, Zisk A (2014) The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am 23(2):185–222. https://doi.org/10.1016/j.chc.2014.01.002
Schulz A, Vogele C (2015) Interoception and stress. Front Psychol 6:993. https://doi.org/10.3389/fpsyg.2015.00993
Schaan VK, Schulz A, Rubel JA, Bernstein M, Domes G, Schachinger H, Vogele C (2019) Childhood trauma affects stress-related interoceptive accuracy. Front Psychiatry 10:750. https://doi.org/10.3389/fpsyt.2019.00750
Hartley CA, Phelps EA (2010) Changing fear: the neurocircuitry of emotion regulation. Neuropsychopharmacology 35(1):136–146. https://doi.org/10.1038/npp.2009.121
Marusak HA, Martin KR, Etkin A, Thomason ME (2015) Childhood trauma exposure disrupts the automatic regulation of emotional processing. Neuropsychopharmacology 40(5):1250–1258. https://doi.org/10.1038/npp.2014.311
Dinkelacker V, Gruter M, Klaver P, Gruter T, Specht K, Weis S, Kennerknecht I, Elger CE, Fernandez G (2011) Congenital prosopagnosia: multistage anatomical and functional deficits in face processing circuitry. J Neurol 258(5):770–782. https://doi.org/10.1007/s00415-010-5828-5
Uddin LQ (2015) Salience processing and insular cortical function and dysfunction. Nat Rev Neurosci 16(1):55–61. https://doi.org/10.1038/nrn3857
Fox MD, Snyder AZ, Vincent JL, Corbetta M, Van Essen DC, Raichle ME (2005) The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc Natl Acad Sci USA 102(27):9673–9678. https://doi.org/10.1073/pnas.0504136102
Shirer WR, Ryali S, Rykhlevskaia E, Menon V, Greicius MD (2012) Decoding subject-driven cognitive states with whole-brain connectivity patterns. Cereb Cortex 22(1):158–165. https://doi.org/10.1093/cercor/bhr099
Fisher HL, Craig TK, Fearon P, Morgan K, Dazzan P, Lappin J, Hutchinson G, Doody GA, Jones PB, McGuffin P, Murray RM, Leff J, Morgan C (2011) Reliability and comparability of psychosis patients’ retrospective reports of childhood abuse. Schizophr Bull 37(3):546–553. https://doi.org/10.1093/schbul/sbp103
Boller B, Mellah S, Ducharme-Laliberte G, Belleville S (2017) Relationships between years of education, regional grey matter volumes, and working memory-related brain activity in healthy older adults. Brain Imaging Behav 11(2):304–317. https://doi.org/10.1007/s11682-016-9621-7
Dedovic K, Renwick R, Mahani NK, Engert V, Lupien SJ, Pruessner JC (2005) The Montreal Imaging Stress Task: using functional imaging to investigate the effects of perceiving and processing psychosocial stress in the human brain. J Psychiatry Neurosci 30(5):319–325
Acknowledgements
We would like to thank the volunteers who participated in this study. We would like to acknowledge Meelah Hamilton (now deceased) Jesseca Rowland, Nicholas Vella Inika Gillis and Nicole O’Reilly for assistance with data collection and entry. We acknowledge recruitment assistance from the Australian Schizophrenia Research Bank (ASRB), which was supported by the National Health and Medical Research Council of Australia (NHMRC) Enabling Grant (No. 386500), the Pratt Foundation, Ramsay Health Care, the Viertel Charitable Foundation and the Schizophrenia Research Institute.
Funding
This study was funded by Project Grants from the NHMRC (APP630471 and APP1081603), and the Macquarie University’s Australian Research Council (ARC) Centre of Excellence in Cognition and its Disorders (CE110001021). MJG was supported by the NMHRC’s R.D. Wright Biomedical Career Development Fellowship (APP1061875; 2014-17). OJW was supported by an Australian Government Research Training Program (RTP) Scholarship (administered by the University of New South Wales) and the Edward C Dunn Foundation Postgraduate Scholarship (administered by Neuroscience Research Australia; NeuRA). The funding bodies had no role in the decision to publish these results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Human Research Ethics committees of the University of New South Wales (HC12384), the South East Sydney and Illawarra Area Health Service (HREC 09/081) and St Vincent’s Hospital (HREC/10/SVH/9).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Quidé, Y., Girshkin, L., Watkeys, O.J. et al. The relationship between cortisol reactivity and emotional brain function is differently moderated by childhood trauma, in bipolar disorder, schizophrenia and healthy individuals. Eur Arch Psychiatry Clin Neurosci 271, 1089–1109 (2021). https://doi.org/10.1007/s00406-020-01190-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-020-01190-3