Abstract
Patients with bipolar disorder and schizophrenia often suffer from severe cognitive impairment even during times of remission. This study investigated the pathomechanisms underlying their deficits in cognitive control. A combined oddball–incongruence fMRI task was applied to examine similarities and differences of neural activation patterns between patients and healthy controls. Bipolar and schizophrenia patients demonstrated hyperactivations in the intraparietal cortex during the oddball condition. Furthermore, bipolar patients revealed diagnosis-specific hyperactivation in the left middle frontal gyrus, precentral gyrus, anteroventral prefrontal cortex and orbitofrontal cortex regions compared to schizophrenia patients and healthy individuals. In comparison to healthy controls the patients showed hypoactivations in the inferior frontal junction and ventral pathway during the cognitively more demanding incongruence. Taken together, bipolar patients seem to recruit frontal and parietal areas during the oddball condition to compensate for potential deficits in their attentional network. During more challenging tasks, i.e., the incongruence condition, their compensatory mechanisms seem to collapse leading to hypoactivations in the same frontal areas as well as the ventral pathway.
Similar content being viewed by others
Introduction
Attention can be defined as the frail balance between concentration on task-relevant information and a continuous unconscious scanning of the environment for stimuli that demand behavioral responses (background monitoring). Selective attention processes underlie cognitive control, which is the ability to focus on a specific stimulus while other stimuli might be present. A possible way to examine cognitive control is through stimulus–response compatibility tasks such as Stroop or incongruence tasks. The Stroop task induces interference effects, so-called response conflicts, by requesting the participants to label a color word’s color, but not its meaning (e.g., the word “green” printed in red) [1]. The resulting decrease in accuracy and reaction time is called “Stroop effect” [2]. On a neurofunctional level, activation differences in anterior cingulate, prefrontal, posterior medial frontal, inferior lateral prefrontal, intraparietal and inferior parietal cortices, as well as occipito-temporal areas have been reported to be associated with cognitive control processes dealing with incongruence [3,4].
Whereas the incongruence effect is elicited by response conflicts, oddball tasks have been related to a series of cognitive processes including categorization, response selection, execution of response, etc. and do not simply map one particular course of action [5]. However, involvement of the ventral attention network in these tasks has been demonstrated multiple times. Studies involving detection of unattended, but salient and behaviorally relevant stimuli indicate an impact of functional properties of frontoparietal regions (in particular the temporoparietal junction). Both tasks require a shielding of task-relevant processing from task-irrelevant stimulus information. Incongruence and oddball tasks share activation patterns in similar frontoparietal networks proposing a similar underlying network for cognitive control processes [4].
Attentional deficits and their connection to psychiatric disorders have a long history of intense research. In particular schizophrenia has been extensively studied regarding difficulties and dysfunctions in cognition and information processing [6], for example processing speed [7], attention [8] and cognitive inhibition [9]. Furthermore, studies reported deficits in all aspects of cognitive performance in acute as well as remitted patients [10,11]. Similar results could be found in bipolar disorder [12]. It is important to note that cognitive impairment not only occurs during acute episodes but can also be present in euthymic patients. Two different meta-analytic reviews showed that neuropsychological and -cognitive function across various tasks (e.g., executive functioning, verbal learning, etc.) was impaired in euthymic bipolar patients compared to healthy controls [13,14]. Deficits in cognitive function might be influenced by following factors: prior experience of psychosis, duration of illness, frequency of manic and depressive episodes and age of onset [15,16]. Comparisons between the two disorders report comparable difficulties in executive function of bipolar patients and schizophrenia patients [17,18].
These results are further supported by functional magnetic resonance imaging (fMRI) studies, which investigated neural correlates of underlying cognitive impairments that have been observed during several neurocognitive tasks. For instance, Wolter et al. [19] have shown that in the same combined oddball–incongruence task, schizophrenia patients demonstrated hyperactivity in the intraparietal cortex during the oddball and incongruence task. Furthermore, there are multiple fMRI studies investigating cognitive control processes in schizophrenia or bipolar patients compared to healthy controls. However, there are almost no studies comparing between-diagnoses effects. Seok Jeong et al. found activation in the right precentral gyrus in schizophrenia patients but not in the healthy control group during a Stroop task [20]. Furthermore, Wagner et al. and Laurens et al. presented hypoactivations in the fronto-thalamic network as well as cingulate regions in schizophrenia patients [21,22]. These findings were confirmed by two meta-analyses [23,24]. Moreover, hypoactivation was shown consistently in bipolar patients in the right inferior frontal gyrus across various cognitive control studies including two meta-analyses [23,25,26,27]. Additionally, hyperactivation was found in bipolar patients compared to healthy controls in the inferior thalamus and left putamen [28]. To summarize, functional abnormalities have been demonstrated in both disorders during executive function paradigms but need further validation to elucidate potential pathomechanisms underlying cognitive control deficits.
In the present study, a combined oddball–incongruence paradigm [4,19] was employed to investigate the potential differences in cognitive control processes of bipolar disorder and schizophrenia patients. By comparing behavioral and fMRI data of both diagnoses and healthy individuals, it was aimed to gain a deeper understanding of the pathophysiology of bipolar disorder and schizophrenia.
Method
Participants
A total of 90 subjects—20 bipolar, 30 schizophrenia patients and 40 healthy controls—took part in this study. Patients were recruited from the Department of Psychiatry and Psychotherapy, University Medical Center Göttingen. All patients met the criteria of schizophrenia or bipolar disorder according to International Statistical Classification of Diseases and Related Health Problems 10 (ICD-10) classification standards. Both acute and partly remitted patients were involved in the study depending on their overall cognitive state. All healthy controls were recruited from the local population and matched for age, education level and gender, refer to Table 1 for further details. For bipolar patients, symptom severity was assessed using the Montgomery–Asberg Depression Rating Scale (MADRS) and the Young Mania Rating Scale (YMRS); while for schizophrenia patients, the MADRS and Positive and Negative Symptom Scale (PANSS) was used.
Exclusion criteria included lifetime diagnoses of substance dependence, substance abuse during the last month, cannabis abuse within the last two weeks, mental retardation, dementia and neurological illnesses. Secondary psychiatric lifetime comorbidities such as anxiety or personality disorders were no exclusion criteria and were present in a few patients. However, only patients treated for the primary diagnoses of schizophrenia or bipolar disorder were included in the study.
The study protocol was reviewed and approved by the local ethics committee. Informed consent was obtained from all individual participants included in the study. The study was carried out in accordance with the latest version of the Declaration of Helsinki. Participants received an expense allowance.
Experimental protocol
Subjects were trained on the combined oddball–incongruence paradigm (described in [4, 19]) prior to being scanned and later performed the task inside a 3 T Siemens TrioTim scanner. First, all participants were instructed to categorize geometric objects by their respective shape or color via a button press as fast and as accurately as possible. The paradigm presented five experimental conditions implemented with stimuli of two different shapes (A or B) and three colors (red, blue or white). A task cue specified whether the shape or color had to be identified in the following trial. All stimuli embodied two dimensions—a relevant and an irrelevant one. The relevant dimension was the task asked for (e.g., shape); whereas the irrelevant one was to be ignored/ neglected (e.g., color). The tasks consisted of a congruent and incongruent color condition, a congruent and incongruent shape condition and the oddball condition. The stimuli were presented in a trial-by-trial manner. Task conditions were arranged pseudo-randomly, ensuring that participants were not able to predict a task switch for the subsequent trial.
Each trial started with a demonstration of the relevant task cue for 500 ms. After a 250-ms cue-stimulus interval, the stimulus was presented for 750 ms. Participants had 1000 ms to react to the stimulus (750-ms stimulus presentation + 250-ms stimulus-cue interval). During the shape task, subjects had to press the left button with their index finger for object A and the right button with their middle finger for object B—independent of their color. In the color task, participants had to press the left button with their index finger when the object was red and the right button with their middle finger when the object was blue—independent of their shape. All participants had to respond with their right hand.
Congruent stimuli were mapped on the same response button, i.e., red and object A or blue and object B. The incongruent stimuli led to a mismatch because the two stimuli dimensions were mapped on two different response buttons, (i.e., red and object B or blue and object A). In the shape task, a white object represented the so-called “oddball” stimulus, which appeared much less frequently than the congruent and incongruent stimuli. For more information see Fig. 1.
This illustration depicts an example of three of the five possible conditions. On the left, participants have to respond to the color of the object. The color and shape of the object match the same button press, which corresponds to a congruent condition. In the middle, subjects have to respond to the shape of the object. The color and shape do not match the same button press resulting in an incongruent condition. On the right, participants have to respond to the shape of the object. The presentation of a rare white object is called the oddball condition. The figure was created with Inkscape 0.92.3
Behavioral data analysis
Behavioral data were analyzed with IBM SPSS (SPSS Versions 25, Chicago, IL, USA). The Shapiro–Wilk test was used to check normal distribution of performance and mean reaction times of correct trials of all subjects during the oddball and incongruence tasks. Performance differences between patients and healthy controls were further analyzed with the non-parametric Kruskal–Wallis test. A one-way ANOVA was applied for the analysis of the deltas between both task conditions and mean reaction times.
fMRI data acquisition and analyses
The experiment was performed on a 3-T MRI Scanner (Magnetom TrioTim syngo; Siemens Healthcare, Erlangen, Germany). A high-resolution T1-weighted anatomical scan (3D-MPRAGE, voxel size 1 × 1 × 1 mm3) was obtained for each subject. 251 functional images were acquired using a T2*-sensitive echo planar imaging (EPI) sequence (voxel size, 3 × 3 × 3 mm3; 20% gap; TR = 2000 ms; echo time, 30 ms; flipangle, 70°; field-of-view, 192 mm), with 33 axial slices parallel to the anterior commissure–posterior commissure plane in ascending direction.
Stimuli were presented with Presentation Software (Neurobehavioral Systems, Albany, USA) through MR-compatible LCD goggles. A button box recorded the participants’ response.
Statistical Parametric Mapping SPM8 (Wellcome Trust Centre for Neuroimaging, London, UK) was used to preprocess and analyze the functional imaging data. The EPI images were corrected for head movement by realigning them to the first image. A cutoff value of 3 mm was determined for the three planes of translation and 3° for the three planes of rotation. If this value was exceeded at any time during the paradigm, subjects were excluded from the analysis. Slice time correction was applied to the realigned and unwarped functional images. They were subsequently normalized to the MNI space and saved with a spatial resolution of 3 × 3 × 3 mm3. A 9-mm full-width at half-maximum (FWHM) isotropic Gaussian kernel was used for smoothing. Segmentation and co-registration of the high-resolution anatomical image was utilized with the mean EPI image. Statistical analyses applied a general linear model (GLM), which comprised five regressors (i.e., the congruent and incongruent conditions for shape and color and oddball condition). Only correct trials were included in the analyses. Linear t-contrasts were defined for measuring differential effects elicited by the experimental conditions. SPM 12 was used for the comparison of bipolar and schizophrenia patients as well as both patient groups and healthy controls during the incongruence and oddball condition. Single-subject contrast images of the oddball condition against implicit baseline and incongruence condition against implicit baseline (shape task) were taken to the second level to assess group effects. A one-way ANOVA with three groups (bipolar patients, schizophrenia patients and healthy controls) was used to determine the differences between the diagnoses as well as between the individual patient and healthy control group. Statistical effects were determined at a search criterion of p < 0.005, uncorrected. For brain regions with a priori hypotheses, i.e., for the left intraparietal cortex, small volume corrections (SVC) were used (left intraparietal cortex: − 36 − 60 40; coordinate taken from Gruber et al. [4].
Results
Behavioral data
First, a comparison of correct response rates and mean reaction times was conducted between bipolar and schizophrenia patients as well as healthy controls during the incongruence and oddball condition (Table 2).
Performance, defined as correct response rates, during the oddball condition was significantly affected by diagnosis (H(2) = 14.841, p = 0.001). Follow-up analyses resulted in significant differences between schizophrenia patients and healthy controls (p = 0.001, r = − 0.422) as well as bipolar patients and healthy controls (p = 0.017, r = − 0.356), but not between the patient groups (p = 1.000, r = 0.047), indicating worse performance of both patient groups compared to healthy controls. Furthermore, significant differences in the performance during the incongruent condition could be revealed (H(2) = 12.247, p = 0.002). Schizophrenia patients presented significantly worse performance compared to healthy controls (p = 0.002, r = − 0.408). There was no significant difference in the performance between bipolar and schizophrenia patients (p = 1.000, r = 0.136) as well as bipolar disorder and healthy individuals (p = 0.138, r = − 0.258). Performance data show the impairments of schizophrenia patients during both conditions. Bipolar patients displayed deficits compared to healthy controls during the oddball but not incongruent condition. The deltas between the congruence versus incongruence and congruence versus oddball condition in the performance data did not reveal any significant variations between patients or healthy controls (Δ congruence vs incongruence: F(2, 89) = 1.731, p = 0.183, r = 0.196, ω2 = 0.016; Δ congruence vs oddball: F(2, 89) = 1.335, p = 0.269, r = 0.173, ω2 = 0.007).
A one-way ANOVA reported significant modulation of the groups’ mean reaction time by diagnosis during the oddball condition (F(2, 89) = 7.155, p = 0.001, r = 0.376, ω2 = 0.120). Pairwise comparisons with adjusted p-values revealed significantly slower reaction times of the schizophrenia group compared to healthy individuals (p = 0.002). Furthermore, increased reaction times of bipolar patients compared to healthy controls reached significance (p = 0.031). Mean reaction times between the two patient groups did not differ. In the incongruence condition, a between-group effect could be found (F(2, 89) = 6.681, p = 0.002, r = 0.369, ω2 = 0.115). The processing speed of the two patient groups appeared significantly slower than in the control group (SCZ vs. HC: p = 0.003; BD vs HC: p = 0.021) and there was no significant difference between the patient groups. The difference between congruence versus incongruence as well as congruence versus oddball condition did not reveal any significant variations in the reaction times of the groups (Δ congruence vs incongruence: F(2, 89) = 0.399, p = 0.672, r = 0.095, ω2 = − 0.014; Δ congruence vs oddball: F(2, 89) = 1.273, p = 0.285, r = 0.169, ω2 = 0.006).
fMRI results—oddball condition
At first, the comparison between bipolar disorder patients and healthy controls revealed hyperactivation of the bipolar group in the left hemisphere, in regions such as the middle frontal gyrus (MFG), precentral gyrus, orbitofrontal cortex (OFC) and anteroventral prefrontal cortex (avPFC) (Table 3). All of these areas were also found to be hyperactivated in bipolar patients in comparison to schizophrenia patients (Fig. 2). These results indicate a diagnosis-specific increase of activation in frontal brain areas of bipolar disorder patients, i.e., a qualitative difference in activation patterns between bipolar disorder and schizophrenia. In addition, purely quantitative differences of activation between bipolar and schizophrenia patients, i.e., diagnosis-unspecific hyperactivations, were found in the intraparietal cortex. Bipolar patients presented enhanced activation in the intraparietal cortex bilaterally compared to healthy controls and schizophrenia patients. In addition, and in line with previous results from Wolter et al. [19], hyperactivation in the right intraparietal cortex of schizophrenia patients compared to healthy controls could be replicated.
Bipolar patients compared to schizophrenia patients revealed diagnosis-specific hyperactivation evoked by the oddball condition in the left middle frontal gyrus (− 36 33 30; p = 0.005, uncorrected), left orbitofrontal cortex (− 24 39 − 12; p = 0.005, uncorrected), left precentral gyrus (− 45 6 51; p = 0.005, uncorrected) and left anteroventral prefrontal cortex (− 21 48 6; p = 0.005, uncorrected). The figure was created with MRIcroGL and Inkscape 0.92.3. MFG middle frontal gyrus, OFC orbitofrontal cortex, avPFC anteroventral prefrontal cortex
Among the changes of brain activity found in bipolar and schizophrenia patients, some were related to deactivations instead of activations elicited by the experimental paradigm. More specifically, the outcomes showed decreased activation in the inferior frontal junction bilaterally, left ventral pathway and right pars triangularis (Fig. 3). These hypoactivations of the patients occurred independent of their exact diagnosis, i.e., they were diagnosis-unspecific (see Table 4).
Bipolar (red) and schizophrenia (yellow) patients demonstrated diagnosis-unspecific hypoactivations in a the ventral pathway (BD: − 33 − 66 − 3, p < 0.005, uncorrected; SCZ: − 36 − 69 9, p < 0.005, uncorrected) and b the inferior frontal junction (BD: 54 0 18, p < 0.005, uncorrected; SCZ: 42 6 27, p < 0.005, uncorrected) and inferior frontal gyrus (BD: 48 36 6, p < 0.005, uncorrected; SCZ: 42 42 6, p < 0.005, uncorrected) in comparison to healthy controls. The figure was created with MRIcroGL and Inkscape 0.92.3
fMRI results—incongruence condition
Brain areas that were found to be hypoactivated in schizophrenia and bipolar patients compared to healthy controls during the oddball condition, also showed hypoactivations in the incongruence condition. These regions comprise the inferior frontal junction, ventral pathway and pars triangularis.
Furthermore, previous detected hyperactivations in the left prefrontal gyrus, intraparietal cortex, MFG and avPFC during the oddball condition of the patient groups compared to healthy controls, could not be found in the incongruence condition. In fact, patients demonstrated hypoactivations in the avPFC, MFG, intraparietal cortex and prefrontal gyrus in the incongruence condition (Table 5).
Discussion
This fMRI study aimed to shed light on pathophysiological similarities and differences of neural correlates of cognitive control processes in bipolar related to schizophrenia patients and healthy controls by examining an oddball and incongruence task. It was of special interest to examine: (i) diagnosis-specific and (ii) diagnosis-overlapping cognitive processing effects. Both, response conflict (incongruence condition) and contextual mismatch (oddball condition), induced activation in superior frontal and parietal, central and occipital regions that have been shown to be associated with cognitive control processes [29,30,31,32,33,34]. In the current study, diagnosis-specific hyperactivation of the bipolar disorder group in comparison to healthy controls and schizophrenia patients could be found in frontal regions such as the left avPFC, OFC, precentral gyrus and MFG during the oddball condition. Increased activations in those brain areas were all specific to the bipolar patients and, hence, represent a qualitative difference in relation to schizophrenia. Enhanced activation in the intraparietal cortex, on the other hand, could be found not only in the bipolar, but also in the schizophrenia group. In addition, significant hypoactivations in both patient groups were found in frontal areas and in the ventral pathway. Results of the incongruence task demonstrated hypoactivations of schizophrenia and bipolar patients compared to healthy individuals in the ventral pathway and inferior frontal junction. However, in contrast to the oddball condition, patients revealed hypoactivations in the intraparietal cortex, MFG, avPFC and left precentral gyrus during the incongruence condition.
Hyperactivations found in frontal areas during the oddball condition were specific for the bipolar disorder group. Additionally, the behavioral data results revealed a significantly reduced accuracy of bipolar patients compared to healthy controls. Together this might indicate a malfunction of bipolar patients in cognitive control processing leading to a compensatory increase in frontal brain activation. Previous studies examining cognitive control have already shown increased activation in frontal areas of bipolar disorder compared to healthy controls [35,36]. These results suggest overall disturbed attention mechanisms in bipolar patients, resulting in potential hyperactivations of selective brain regions to maintain their performance. Additionally, it has been shown that patients with obsessive–compulsive disorder exhibited enhanced frontal activation compensating for their impaired performance on a working memory task [37].
Whereas bipolar patients recruited additional frontal areas such as the avPFC or OFC to counterbalance their deficits, schizophrenia patients might not be able to compensate for their reduced attentional capacity through hyperactivation of frontal regions in the oddball condition. Similar effects have already been shown in a study by McIntosh et al., who reported increased activation of bipolar patients compared to schizophrenia patients in the OFC during the Hayling Sentence Completion test [38]. Additionally, the middle frontal gyrus has already been reported to show decreased activation in ultra-high-risk, early and chronic schizophrenia patients during a visual oddball task [39]. The authors proposed that decreased activation in the middle frontal gyrus during the oddball condition might result from disrupted processing of and response to task-relevant stimuli due to the inability of consequently neglecting task-irrelevant inputs. While dopamine regulates contextually meaningful salience in healthy controls, a dysfunctional and uncontrolled dopamine release in schizophrenia might induce inappropriate salience to irrelevant inputs.
Furthermore, it has repeatedly been shown that schizophrenia patients suffer from greater cognitive impairment than bipolar disorder patients [40,41,42,43,44]. Consequently, their compensation mechanisms seem to be more limited than in affective disorders which may explain the missing compensatory activation in frontal brain areas observed in this study. This explanation might also be valid for the effects exhibited in the intraparietal cortex. Wolter et al. [19] reported hyperactivation of schizophrenia patients in comparison to healthy controls in the intraparietal cortex applying the same paradigm. In the current study, subjects with bipolar disorder displayed significant hyperactivation in the intraparietal cortex compared to healthy controls and schizophrenia patients, whereas subjects with schizophrenia showed low-threshold activation differences in comparison to healthy controls. It seems that bipolar and schizophrenia patients used similar compensation strategies, but significantly differed in the quantitative extent. The difference to the results of Wolter et al. [19] could result from the increased sample size of schizophrenia patients. Individual differences in the performance capacity of schizophrenia patients influence the outcome of the group comparison. Whereas the previous study detected hyperactivation in the oddball and incongruence condition of schizophrenia patients compared to healthy individuals, it seems as if more subjects of the present sample had deficits in response conflict processing. In consequence, these deficits might result in hypoactivation of the intraparietal cortex during the incongruence condition. It has repeatedly been shown that schizophrenia comprises a very heterogeneous group of symptoms or even level of cognitive performance [45]. These differences might potentially also affect the functional outcome quantitatively. Consequently, due to a potential shift of the overall performance during the oddball condition, the effects stated by Wolter et al. [19], could only be replicated in a low-threshold manner.
Taken together, the compensatory mechanisms of the bipolar patients led to hyperactivations in intraparietal as well as frontal regions in the oddball condition, whereas schizophrenia patients only exhibited hyperactivation in the intraparietal cortex. The results of Melcher et al. [40] concur with this outcome as they found in a study with similar versions of this neuropsychological task that overall, schizophrenia patients seem to have greater dysfunctions than bipolar patients in inhibitory control and attention maintenance. They described an increased conflict and oddball effect on the reaction times of schizophrenia patients in comparison to bipolar and healthy individuals. In this study, the diagnoses did not induce a conflict and oddball effect on the reaction times or accuracy. At the descriptive level, however, schizophrenia patients demonstrated a significant difference in performance scores between congruence and incongruence as well as congruence versus oddball condition indicating deficits in the processing of incongruence and oddball effects. Therefore, bipolar patients seem to be able to compensate for their behavioral deficits, whereas schizophrenia patients have limited compensation capacities resulting in less activation of frontal areas.
Hypoactivations of bipolar and schizophrenia patients were found in the ventral pathway. Associations between the visual cortex and the temporal lobe, or more specifically its respective connections to limbic and frontal areas, make it possible to process visual information. In particular, attention to and processing of feature dimensions (such as shape or color) has been reported to activate the ventral stream [46,47,48]. It can be hypothesized that healthy controls might process visual stimuli more efficiently. Patients, on the other hand, might have greater deficits in directing their attention to visual stimuli to the same extent as healthy controls. Furthermore, it might be possible that auditory distraction due to scanner noises caused interference with their stimuli processing leading to attentional deficits. The current literature presents a mixed picture regarding this hypothesis, i.e., not only hypoactivation of schizophrenia patients in the ventral stream during visual perception [49,50,51,52], but also hyperactivation in the lateral occipital complex in a task involving object recognition and mapping of visual-spatial attention [53]. There seem to be no studies examining visual perception of bipolar patients with fMRI. However, neurocognitive object perception tasks demonstrated deficits in bipolar patients [54,55]. It can be concluded that the specific neural mechanisms have not yet been fully elucidated, however, object processing seems to be aberrant in bipolar disorder and schizophrenia.
In addition, diagnosis-unspecific hypoactivations of the patient groups in the inferior frontal junction might represent difficulties in shifting attention from novel to the relevant stimulus dimension. Healthy controls activate the inferior frontal junction during goal-directed and stimulus-driven attention [56,57],whereas, bipolar and schizophrenia patients exhibit impaired ability in shifting attention to the target stimulus [40,58,59].
The second task in this experiment, i.e., the incongruence condition, focused on activations in the brain responsible for response conflict and executive control. Previous studies demonstrated activation in similar brain regions, i.e., the frontoparietal network during incongruence and oddball conditions [19,31,60]. Therefore, it is no surprise that the activation patterns of healthy controls were constant across both conditions, i.e., comparable regions were activated to a similar extent. Comparable results have already been demonstrated in numerous studies, repeatedly reporting activation of the inferior frontal junction, precentral gyrus, ventral pathway, intraparietal cortex and occipital regions during oddball and incongruence tasks [32,33,61,62,63,64,65]. These results suggest the involvement of partly overlapping brain regions in the processing of oddball effects as well as response conflict during incongruence tasks.
Results from the comparison between the two patient groups and healthy controls in the incongruence condition revealed hypoactivations of the patient groups in areas such as the inferior frontal junction, avPFC, MFG, intraparietal cortex and superior frontal gyrus. Thereby, overlapping hypoactivations in regions such as the inferior frontal junction, ventral pathway and right pars triangularis can be observed in both conditions. These results indicate a partly shared pathophysiological decrease in activation in bipolar and schizophrenia patients during the processing of the oddball and incongruence stimuli.
However, there seem to be additionally diagnosis-specific differences in the functional responses to the oddball and incongruence stimuli. This effect might result from a variance in difficulty of the two conditions. Whereas the incongruence condition seems to be more difficult due to its stimulus–response mapping dimension, the oddball condition does not entail this dimension. As a result, the oddball task seems to be easier, which is also supported by the fact that the correct response rates in the healthy control group were significantly greater compared to the incongruence condition. In consequence, bipolar patients might exhibit more deficits in the incongruence condition than in the oddball condition resulting in hypoactivation of the left prefrontal gyrus and intraparietal cortex compared to healthy controls. A possible explanation for this effect results from a model described multiple times in the last decade [66,67,68,69]. It states that in general, the neurophysiological response curve of each individual increases with enhanced task difficulty. After exceeding an individual tipping point, the functional response decreases with further difficulty resulting in an inverted U-shaped curve. As psychiatric patients have performance deficits, their neurofunctional response increases and decreases earlier, i.e., already in easier tasks, leading to a left-shifted U-shaped curve. This means, more precisely, that during easier tasks (in this case the oddball condition) patients overcompensate with stronger activations in various brain regions. However, as soon as a certain/individual attention capacity is exceeded (i.e., the incongruence condition), they demonstrate hypoactivations as compared to healthy individuals. Following this hypothesis, it is possible that bipolar patients had difficulties with both conditions but were able to recruit frontal and parietal brain regions to support task accomplishment in the oddball condition. The incongruence condition, however, might require too much cognitive capacity so that they fail to involve assisting networks and respond with decreased activation. In the schizophrenia group, hyperactivation was found in the intraparietal cortex in the oddball condition, but shifted to hypoactivation in the incongruence condition. In consequence, it can be hypothesized that this group has greater deficits per se but struggled even more in the incongruence condition.
It is important to note that the two patient groups varied in the distribution of females and males, i.e., the bipolar group included 12 females and 8 males; whereas the schizophrenia group consisted of 4 females and 26 males. As a consequence, the analyses was repeated with gender as a covariate. Overall, the results remained consistent suggesting that the gender of the subjects did not influence the outcomes of this study. However, it has to be mentioned that the literature provides inconsistent results regarding the influence of gender on cognitive control processes. Some studies presented activation differences in the frontoparietal network during cognitive control tasks between women and men [70,71], whereas other authors ruled out sex differences in functional or resting-state connectivity networks related to cognitive control processes [72,73]. One potential interpretation of sex differences is suggested to be the influence of estradiol on cognitive control processes [74]. It can be concluded that effects of gender or sex hormones have not been fully resolved, yet. In the current study, gender does not seem to be a driving force between differences found in cognitive control processing of bipolar and schizophrenia patients as well as healthy controls.
Taken together, this study provided new insights into the functional responses underlying attentional processes induced by oddball and incongruence stimuli in bipolar and schizophrenia patients. The current results revealed the involvement of shared brain areas in the processing of oddball and incongruence stimuli, yet pathophysiological differences between bipolar and schizophrenia patients as well as healthy controls. Bipolar patients presented greater activation in frontal as well parietal brain regions during the oddball condition compared to schizophrenia and healthy individuals. Schizophrenia patients revealed low-threshold hyperactivation in the right intraparietal cortex compared to healthy controls. Additionally, both patient groups exhibited hypoactivations in the ventral pathway and frontal areas compared to healthy controls. The incongruence condition seemed to require greater cognitive capacities resulting in a collapse of compensatory mechanisms and hence hypoactivations of both patient groups compared to healthy controls in frontal and intraparietal regions. As a result, the activation levels of both psychiatric disorders seem to greatly depend on the task difficulty. However, additional studies with greater or evenly distributed sample sizes will be necessary to avoid group size effects. As it was not controlled for medication, psychopharmacological effects on brain activation cannot be excluded and might have led to variance in the results. Prospective studies might, therefore, need to solely examine medication-naïve patients to prevent psychopharmacological effects. All in all, both psychiatric disorders presented activation differences during the processing of oddball and incongruence effects compared to healthy controls. Bipolar patients seem to accomplish intermediate performance by recruiting frontal and parietal brain regions. However, as soon as the task difficulty exceeded their cognitive performance spectrum, their compensation strategies collapsed resulting in hypoactivations of corresponding brain areas.
Change history
09 June 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00406-021-01276-6
References
Stroop JR (1935) Studies of Interference in Serial Verbal Reactions. J Exp Psychol 18(643)
Fitts PM, Seeger CM (1953) S-R compatibility: spatial characteristics of stimulus and response codes. J Exp Psychol 46(3):199–210
Durston S, Davidson MC, Thomas KM, Worden MS, Tottenham N, Martinez A, Watts R, Ulug AM, Casey BJ (2003) Parametric manipulation of conflict and response competition using rapid mixed-trial event-related fMRI. Neuroimage 20(4):2135–2141
Gruber O, Melcher T, Diekhof EK, Karch S, Falkai P, Goschke T (2009) Brain mechanisms associated with background monitoring of the environment for potentially significant sensory events. Brain Cogn 69(3):559–564. https://doi.org/10.1016/j.bandc.2008.11.008
Corbetta M, Patel G, Shulman GL (2008) The reorienting system of the human brain: from environment to theory of mind. Neuron 58(3):306–324. https://doi.org/10.1016/j.neuron.2008.04.017
Barch DM, Ceaser A (2012) Cognition in schizophrenia: core psychological and neural mechanisms. Trends Cogn Sci 16(1):27–34. https://doi.org/10.1016/j.tics.2011.11.015
Andersen R, Fagerlund B, Rasmussen H, Ebdrup BH, Aggernaes B, Gade A, Oranje B, Glenthoj B (2013) The influence of impaired processing speed on cognition in first-episode antipsychotic-naive schizophrenic patients. Eur Psychiatry 28(6):332–339. https://doi.org/10.1016/j.eurpsy.2012.06.003
Mohn C, Torgalsboen AK (2018) Details of attention and learning change in first-episode schizophrenia. Psychiatry Res 260:324–330. https://doi.org/10.1016/j.psychres.2017.12.001
Gigaux J, Le Gall D, Jollant F, Lhuillier JP, Richard-Devantoy S (2013) Cognitive inhibition and quality of life in schizophrenia: a pilot study. Schizophr Res 143(2–3):297–300. https://doi.org/10.1016/j.schres.2012.11.019
Keefe RS, Bilder RM, Harvey PD, Davis SM, Palmer BW, Gold JM, Meltzer HY, Green MF, Miller DD, Canive JM, Adler LW, Manschreck TC, Swartz M, Rosenheck R, Perkins DO, Walker TM, Stroup TS, McEvoy JP, Lieberman JA (2006) Baseline neurocognitive deficits in the CATIE schizophrenia trial. Neuropsychopharmacology 31(9):2033–2046. https://doi.org/10.1038/sj.npp.1301072
Saykin AJ, Shtasel DL, Gur RE, Kester DB, Mozley LH, Stafiniak P, Gur RC (1994) Neuropsychological deficits in neuroleptic naive patients with first-episode schizophrenia. Arch Gen Psychiatry 51(2):124–131
Martinez-Aran A, Vieta E, Reinares M, Colom F, Torrent C, Sanchez-Moreno J, Benabarre A, Goikolea JM, Comes M, Salamero M (2004) Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry 161(2):262–270. https://doi.org/10.1176/appi.ajp.161.2.262
Robinson LJ, Thompson JM, Gallagher P, Goswami U, Young AH, Ferrier IN, Moore PB (2006) A meta-analysis of cognitive deficits in euthymic patients with bipolar disorder. J Affect Disord 93(1–3):105–115. https://doi.org/10.1016/j.jad.2006.02.016
Torres IJ, Boudreau VG, Yatham LN (2007) Neuropsychological functioning in euthymic bipolar disorder: a meta-analysis. Acta Psychiatr Scand Suppl 434:17–26. https://doi.org/10.1111/j.1600-0447.2007.01055.x
Martinez-Aran A, Vieta E, Colom F, Torrent C, Sanchez-Moreno J, Reinares M, Benabarre A, Goikolea JM, Brugue E, Daban C, Salamero M (2004) Cognitive impairment in euthymic bipolar patients: implications for clinical and functional outcome. Bipolar Disord 6(3):224–232. https://doi.org/10.1111/j.1399-5618.2004.00111.x
Zubieta JK, Huguelet P, Lajiness-O'Neill R, Giordani BJ (2001) Cognitive function in euthymic bipolar I disorder. Psychiatry Res 102(1):9–20
Martinez-Aran A, Penades R, Vieta E, Colom F, Reinares M, Benabarre A, Salamero M, Gasto C (2002) Executive function in patients with remitted bipolar disorder and schizophrenia and its relationship with functional outcome. Psychother Psychosom 71(1):39–46. https://doi.org/10.1159/000049342
Balanza-Martinez V, Tabares-Seisdedos R, Selva-Vera G, Martinez-Aran A, Torrent C, Salazar-Fraile J, Leal-Cercos C, Vieta E, Gomez-Beneyto M (2005) Persistent cognitive dysfunctions in bipolar I disorder and schizophrenic patients: a 3-year follow-up study. Psychother Psychosom 74(2):113–119. https://doi.org/10.1159/000083170
Wolter SP, Vieker H, Melcher T, Trost S, Diekhof E, Richter A, Zilles D, Gruber O (2016) Dysregulation within the prefronto-parietal background-monitoring network in schizophrenia. J Behav Brain Sci 6:364–376. https://doi.org/10.4236/jbbs.2016.69035
Seok Jeong B, Soo Kwon J, Yoon Kim S, Lee C, Youn T, Moon C-H, Yoon Kim C (2005) Functional imaging evidence of the relationship between recurrent psychotic episodes and neurodegenerative course in schizophrenia. Psychiatry Res Neuroimaging 139(3):219–228. https://doi.org/10.1016/j.pscychresns.2004.01.008
Wagner G, Koch K, Schachtzabel C, Schultz CC, Gaser C, Reichenbach JR, Sauer H, Bar KJ, Schlosser RG (2013) Structural basis of the fronto-thalamic dysconnectivity in schizophrenia: a combined DCM-VBM study. NeuroImage Clin 3:95–105. https://doi.org/10.1016/j.nicl.2013.07.010
Laurens KR, Kiehl KA, Ngan ETC, Liddle PF (2005) Attention orienting dysfunction during salient novel stimulus processing in schizophrenia. Schizophr Res 75(2–3):159–171. https://doi.org/10.1016/j.schres.2004.12.010
Alustiza I, Radua J, Pla M, Martin R, Ortuno F (2017) Meta-analysis of functional magnetic resonance imaging studies of timing and cognitive control in schizophrenia and bipolar disorder: evidence of a primary time deficit. Schizophr Res 188:21–32. https://doi.org/10.1016/j.schres.2017.01.039
Minzenberg MJ, Laird AR, Thelen S, Carter CS, Glahn DC (2009) Meta-analysis of 41 functional neuroimaging studies of executive function in schizophrenia. Arch Gen Psychiatry 66(8):811–822. https://doi.org/10.1001/archgenpsychiatry.2009.91
Frangou S (2011) Brain structural and functional correlates of resilience to bipolar disorder. Front Hum Neurosci 5:184. https://doi.org/10.3389/fnhum.2011.00184
Pompei F, Jogia J, Tatarelli R, Girardi P, Rubia K, Kumari V, Frangou S (2011) Familial and disease specific abnormalities in the neural correlates of the stroop task in bipolar disorder. Neuroimage 56(3):1677–1684. https://doi.org/10.1016/j.neuroimage.2011.02.052
Hajek T, Alda M, Hajek E, Ivanoff J (2013) Functional neuroanatomy of response inhibition in bipolar disorders–combined voxel based and cognitive performance meta-analysis. J Psychiatr Res 47(12):1955–1966. https://doi.org/10.1016/j.jpsychires.2013.08.015
Blumberg HP, Martin A, Kaufman J, Leung HC, Skudlarski P, Lacadie C, Fulbright RK, Gore JC, Charney DS, Krystal JH, Peterson BS (2003) Frontostriatal abnormalities in adolescents with bipolar disorder: preliminary observations from functional MRI. Am J Psychiatry 160(7):1345–1347. https://doi.org/10.1176/appi.ajp.160.7.1345
Melcher T, Gruber O (2006) Oddball and incongruity effects during Stroop task performance: a comparative fMRI study on selective attention. Brain Res 1121(1):136–149. https://doi.org/10.1016/j.brainres.2006.08.120
Li Q, Yang G, Li Z, Qi Y, Cole MW, Liu X (2017) Conflict detection and resolution rely on a combination of common and distinct cognitive control networks. Neurosci Biobehav Rev 83:123–131. https://doi.org/10.1016/j.neubiorev.2017.09.032
Bledowski C, Prvulovic D, Goebel R, Zanella FE, Linden DE (2004) Attentional systems in target and distractor processing: a combined ERP and fMRI study. Neuroimage 22(2):530–540. https://doi.org/10.1016/j.neuroimage.2003.12.034
Rusiniak M, Lewandowska M, Wolak T, Pluta A, Milner R, Ganc M, Wlodarczyk A, Senderski A, Sliwa L, Skarzynski H (2013) A modified oddball paradigm for investigation of neural correlates of attention: a simultaneous ERP-fMRI study. MAGMA 26(6):511–526. https://doi.org/10.1007/s10334-013-0374-7
Strobel A, Debener S, Sorger B, Peters JC, Kranczioch C, Hoechstetter K, Engel AK, Brocke B, Goebel R (2008) Novelty and target processing during an auditory novelty oddball: a simultaneous event-related potential and functional magnetic resonance imaging study. Neuroimage 40(2):869–883. https://doi.org/10.1016/j.neuroimage.2007.10.065
Kiehl KA, Laurens KR, Duty TL, Forster BB, Liddle PF (2001) Neural sources involved in auditory target detection and novelty processing: an event-related fMRI study. Psychophysiology 38(1):133–142
Fleck DE, Kotwal R, Eliassen JC, Lamy M, Delbello MP, Adler CM, Durling M, Cerullo MA, Strakowski SM (2011) Preliminary evidence for increased frontosubcortical activation on a motor impulsivity task in mixed episode bipolar disorder. J Affect Disord 133(1–2):333–339. https://doi.org/10.1016/j.jad.2011.03.053
Gruber SA, Dahlgren MK, Sagar KA, Gonenc A, Norris L, Cohen BM, Ongur D, Lewandowski KE (2017) Decreased cingulate cortex activation during cognitive control processing in bipolar disorder. J Affect Disord 213:86–95. https://doi.org/10.1016/j.jad.2017.02.003
Henseler I, Gruber O, Kraft S, Krick C, Reith W, Falkai P (2008) Compensatory hyperactivations as markers of latent working memory dysfunctions in patients with obsessive-compulsive disorder: an fMRI study. J Psychiatry Neurosci 33(3):209–215
McIntosh AM, Whalley HC, McKirdy J, Hall J, Sussmann JE, Shankar P, Johnstone EC, Lawrie SM (2008) Prefrontal function and activation in bipolar disorder and schizophrenia. Am J Psychiatry 165(3):378–384. https://doi.org/10.1176/appi.ajp.2007.07020365
Morey RA, Inan S, Mitchell TV, Perkins DO, Lieberman JA, Belger A (2005) Imaging frontostriatal function in ultra-high-risk, early, and chronic schizophrenia during executive processing. Arch Gen Psychiatry 62(3):254–262. https://doi.org/10.1001/archpsyc.62.3.254
Melcher T, Wolter S, Falck S, Wild E, Wild F, Gruber E, Falkai P, Gruber O (2014) Common and disease-specific dysfunctions of brain systems underlying attentional and executive control in schizophrenia and bipolar disorder. Eur Arch Psychiatry Clin Neurosci 264(6):517–532. https://doi.org/10.1007/s00406-013-0445-9
Altshuler LL, Ventura J, van Gorp WG, Green MF, Theberge DC, Mintz J (2004) Neurocognitive function in clinically stable men with bipolar I disorder or schizophrenia and normal control subjects. Biol Psychiatry 56(8):560–569. https://doi.org/10.1016/j.biopsych.2004.08.002
Krabbendam L, Arts B, van Os J, Aleman A (2005) Cognitive functioning in patients with schizophrenia and bipolar disorder: a quantitative review. Schizophr Res 80(2–3):137–149. https://doi.org/10.1016/j.schres.2005.08.004
Stefanopoulou E, Manoharan A, Landau S, Geddes JR, Goodwin G, Frangou S (2009) Cognitive functioning in patients with affective disorders and schizophrenia: a meta-analysis. Int Rev Psychiatry 21(4):336–356. https://doi.org/10.1080/09540260902962149
Lynham AJ, Hubbard L, Tansey KE, Hamshere ML, Legge SE, Owen MJ, Jones IR, Walters JTR (2018) Examining cognition across the bipolar/schizophrenia diagnostic spectrum. J Psychiatry Neurosci 43(4):245–253
Carruthers SP, Gurvich CT, Meyer D, Australian Schizophrenia Research B, Bousman C, Everall IP, Neill E, Pantelis C, Sumner PJ, Tan EJ, Thomas EHX, Van Rheenen TE, Rossell SL (2019) Exploring heterogeneity on the Wisconsin card sorting test in schizophrenia spectrum disorders: a cluster analytical investigation. J Int Neuropsychol Soc 25(7):750–760. https://doi.org/10.1017/S1355617719000420
Haxby JV, Grady CL, Horwitz B, Ungerleider LG, Mishkin M, Carson RE, Herscovitch P, Schapiro MB, Rapoport SI (1991) Dissociation of object and spatial visual processing pathways in human extrastriate cortex. Proc Natl Acad Sci USA 88(5):1621–1625. https://doi.org/10.1073/pnas.88.5.1621
Reed CL, Klatzky RL, Halgren E (2005) What vs where in touch: an fMRI study. Neuroimage 25(3):718–726. https://doi.org/10.1016/j.neuroimage.2004.11.044
Arrington CM, Carr TH, Mayer AR, Rao SM (2000) Neural mechanisms of visual attention: object-based selection of a region in space. J Cogn Neurosci 12(Suppl 2):106–117. https://doi.org/10.1162/089892900563975
Sehatpour P, Dias EC, Butler PD, Revheim N, Guilfoyle DN, Foxe JJ, Javitt DC (2010) Impaired visual object processing across an occipital-frontal-hippocampal brain network in schizophrenia: an integrated neuroimaging study. Arch Gen Psychiatry 67(8):772–782. https://doi.org/10.1001/archgenpsychiatry.2010.85
Green MF, Lee J, Cohen MS, Engel SA, Korb AS, Nuechterlein KH, Wynn JK, Glahn DC (2009) Functional neuroanatomy of visual masking deficits in schizophrenia. Arch Gen Psychiatry 66(12):1295–1303. https://doi.org/10.1001/archgenpsychiatry.2009.132
Wynn JK, Green MF, Engel S, Korb A, Lee J, Glahn D, Nuechterlein KH, Cohen MS (2008) Increased extent of object-selective cortex in schizophrenia. Psychiatry Res 164(2):97–105. https://doi.org/10.1016/j.pscychresns.2008.01.005
Lee J, Reavis EA, Engel SA, Altshuler LL, Cohen MS, Glahn DC, Nuechterlein KH, Wynn JK, Green MF (2019) fMRI evidence of aberrant neural adaptation for objects in schizophrenia and bipolar disorder. Hum Brain Mapp 40(5):1608–1617. https://doi.org/10.1002/hbm.24472
Silverstein SM, Harms MP, Carter CS, Gold JM, Keane BP, MacDonald A 3rd, Ragland JD, Barch DM (2015) Cortical contributions to impaired contour integration in schizophrenia. Neuropsychologia 75:469–480. https://doi.org/10.1016/j.neuropsychologia.2015.07.003
MacQueen GM, Young LT, Galway TM, Joffe RT (2001) Backward masking task performance in stable, euthymic out-patients with bipolar disorder. Psychol Med 31(7):1269–1277
Jahshan C, Wynn JK, McCleery A, Glahn DC, Altshuler LL, Green MF (2014) Cross-diagnostic comparison of visual processing in bipolar disorder and schizophrenia. J Psychiatr Res 51:42–48. https://doi.org/10.1016/j.jpsychires.2013.12.014
Asplund CL, Todd JJ, Snyder AP, Marois R (2010) A central role for the lateral prefrontal cortex in goal-directed and stimulus-driven attention. Nat Neurosci 13(4):507–512. https://doi.org/10.1038/nn.2509
Tamber-Rosenau BJ, Asplund CL, Marois R (2018) Functional dissociation of the inferior frontal junction from the dorsal attention network in top-down attentional control. J Neurophysiol 120(5):2498–2512. https://doi.org/10.1152/jn.00506.2018
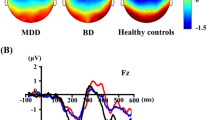
Di Giorgio Silva LW, Cartier C, Cheniaux E, Novis F, Silveira LA, Cavaco PA, de Assis da Silva R, Batista WA, Tanaka GK, Gongora M, Bittencourt J, Teixeira S, Basile LF, Budde H, Cagy M, Ribeiro P, Velasques B (2016) Electrical mapping in bipolar disorder patients during the oddball paradigm. J Psychiatr Res 72:64–71. https://doi.org/10.1016/j.jpsychires.2015.10.012
Bozikas VP, Kosmidis MH, Giannakou M, Kechayas P, Tsotsi S, Kiosseoglou G, Fokas K, Garyfallos G (2014) Controlled shifting of attention in schizophrenia and bipolar disorder through a dichotic listening paradigm. Compr Psychiatry 55(5):1212–1219. https://doi.org/10.1016/j.comppsych.2014.02.014
Huettel SA, Mack PB, McCarthy G (2002) Perceiving patterns in random series: dynamic processing of sequence in prefrontal cortex. Nat Neurosci 5(5):485–490. https://doi.org/10.1038/nn841
Falkenberg LE, Specht K, Westerhausen R (2011) Attention and cognitive control networks assessed in a dichotic listening fMRI study. Brain Cogn 76(2):276–285. https://doi.org/10.1016/j.bandc.2011.02.006
van Veen V, Carter CS (2005) Separating semantic conflict and response conflict in the Stroop task: a functional MRI study. Neuroimage 27(3):497–504. https://doi.org/10.1016/j.neuroimage.2005.04.042
Zysset S, Muller K, Lohmann G, von Cramon DY (2001) Color-word matching stroop task: separating interference and response conflict. Neuroimage 13(1):29–36. https://doi.org/10.1006/nimg.2000.0665
Corbetta M, Kincade JM, Ollinger JM, McAvoy MP, Shulman GL (2000) Voluntary orienting is dissociated from target detection in human posterior parietal cortex. Nat Neurosci 3(3):292–297. https://doi.org/10.1038/73009
Hopfinger JB, Buonocore MH, Mangun GR (2000) The neural mechanisms of top-down attentional control. Nat Neurosci 3(3):284–291. https://doi.org/10.1038/72999
Karlsgodt KH, Glahn DC, van Erp TG, Therman S, Huttunen M, Manninen M, Kaprio J, Cohen MS, Lonnqvist J, Cannon TD (2007) The relationship between performance and fMRI signal during working memory in patients with schizophrenia, unaffected co-twins, and control subjects. Schizophr Res 89(1–3):191–197. https://doi.org/10.1016/j.schres.2006.08.016
Mendrek A, Laurens KR, Kiehl KA, Ngan ET, Stip E, Liddle PF (2004) Changes in distributed neural circuitry function in patients with first-episode schizophrenia. Br J Psychiatry 185:205–214. https://doi.org/10.1192/bjp.185.3.205
Manoach DS (2003) Prefrontal cortex dysfunction during working memory performance in schizophrenia: reconciling discrepant findings. Schizophr Res 60(2–3):285–298
Jansma JM, Ramsey NF, van der Wee NJ, Kahn RS (2004) Working memory capacity in schizophrenia: a parametric fMRI study. Schizophr Res 68(2–3):159–171. https://doi.org/10.1016/S0920-9964(03)00127-0
Christakou A, Halari R, Smith AB, Ifkovits E, Brammer M, Rubia K (2009) Sex-dependent age modulation of frontostriatal and temporo-parietal activation during cognitive control. Neuroimage 48(1):223–236. https://doi.org/10.1016/j.neuroimage.2009.06.070
Li T, Luo Q, Gong H (2010) Gender-specific hemodynamics in prefrontal cortex during a verbal working memory task by near-infrared spectroscopy. Behav Brain Res 209(1):148–153. https://doi.org/10.1016/j.bbr.2010.01.033
Schmidt H, Jogia J, Fast K, Christodoulou T, Haldane M, Kumari V, Frangou S (2009) No gender differences in brain activation during the N-back task: an fMRI study in healthy individuals. Hum Brain Mapp 30(11):3609–3615. https://doi.org/10.1002/hbm.20783
Weissman-Fogel I, Moayedi M, Taylor KS, Pope G, Davis KD (2010) Cognitive and default-mode resting state networks: do male and female brains "rest" differently? Hum Brain Mapp 31(11):1713–1726. https://doi.org/10.1002/hbm.20968
Hjelmervik H, Westerhausen R, Osnes B, Endresen CB, Hugdahl K, Hausmann M, Specht K (2012) Language lateralization and cognitive control across the menstrual cycle assessed with a dichotic-listening paradigm. Psychoneuroendocrinology 37(11):1866–1875. https://doi.org/10.1016/j.psyneuen.2012.03.021
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was partially supported by the Deutsche Forschungsgemeinschaft (DFG) via the Clinical Research Group 241 ‘Genotype–phenotype relationships and neurobiology of the longitudinal course of psychosis’, TP2 (https://www.kfo241.de; grant number GR 1950/5-1 and GR 1950/10-1) and by a further DFG grant to Oliver Gruber (GR 1950/8-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments. The study was approved by the Ethics Committee of the Universitätsmedizin Göttingen.
Informed consent
Informed consent was obtained from all individual participants included in the study. Patients signed informed consent regarding publishing their data.
Additional information
Communicated by Andrea Schmitt.
The original online version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rauer, L., Trost, S., Petrovic, A. et al. Cortical activation abnormalities in bipolar and schizophrenia patients in a combined oddball–incongruence paradigm. Eur Arch Psychiatry Clin Neurosci 271, 1487–1499 (2021). https://doi.org/10.1007/s00406-020-01168-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-020-01168-1