Abstract
Objective
Sublingual immunotherapy (SLIT) has been considered as an effective and safe alternative to the subcutaneous route. However, different modalities and administration methods may lead to significant changes in their adherence and clinical outcomes. The purpose of this study was to compare the adherence, efficacy, and side effects of SLIT medicines: SLITone®, Lais®, and Staloral®.
Subjects and methods
Eighty-two patients suffering from AR symptoms and sensitized only to house dust mite allergens were included. The patients were treated with SLITone®, Lais®, or Staloral®. Treatment outcomes related to efficacy, dropout rate, and adverse events were evaluated. The visual analogue scale (VAS) including sneezing, rhinorrhea, nasal obstruction, and itching was scored from 0 (normal) to 10 (severe), before and after SLIT. Dropout rate was defined as the number of patients who discontinue SLIT of oneself compared to the number of patients who receive SLIT.
Results
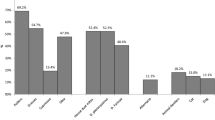
All of the nasal symptoms and total symptom scores were significantly decreased in SLITone®, Lais®, and Staloral®. Furthermore, there were significant difference in the improvement of rhinorrhea and TNSS between SLITone® and Staloral® group (p = 0.011 and p = 0.001, respectively). Four patients out of 26 in SLITone® group, 4 patients out of 30 in Lais® group, and 11 patients out of 26 in Staloral® group have stopped SLIT of themselves. The dropout rate was significantly higher in the Staloral® group than other two groups (p = 0.024). Only one patient complained adverse reaction such as swelling of mouth floor in the Staloral® group.
Conclusion
Although all three SLIT medicines are effective in improving AR symptoms, the adherence to SLIT assessed in accordance with dropout rate was the lowest in the Staloral®.


Similar content being viewed by others
References
Meltzer EO, Blaiss MS, Derebery MJ, Mahr TA, Gordon BR, Sheth KK et al (2009) Burden of allergic rhinitis: results from the pediatric allergies in American survey. J Allergy Clin Immunol 124:S43–S70
Bousquet J, Van Cauwenberge P, Khaltaev N (2001) Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol 108:S147–S334
Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A et al (2008) Allergic rhinitis and its impact on asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 63:8–160
Wheatley LM, Togias A (2015) Clinical practice: allergic rhinitis. N Engl J Med 372:456–463
Greiner AN, Hellings PW, Rotiroti G, Scadding GK (2011) Allergic rhinitis. Lancet 378:2112–2122
Larsen JN, Broge L, Jacobi H (2016) Allergy immunotherapy: the future of allergy treatment. Drug Discov Today 21:26–37
Akdis CA, Barlan IB, Bahceciler N, Akdis M (2006) Immunological mechanisms of sublingual immunotherapy. Allergy 61:11–14
Calderon MA, Alves B, Jacobson M, Hurwitz B, Sheikh A, Durham S (2007) Allergen injection immunotherapy for seasonal allergic rhinitis. Cochrane Database Syst Rev 1:CD001936
Bozek A, Kolodziejczyk K, Kozlowska R, Canonica GW (2017) Evidence of the efficacy and safety of house dust mite subcutaneous immunotherapy in elderly allergic rhinitis patients: a randomized, double-blind placebo-controlled trial. Clin Transl Allergy 7:43
Masuyama K, Goto M, Takeno S, Ohta N, Okano M, Kamijo A et al (2016) Guiding principles of sublingual immunotherapy for allergic rhinitis in Japanese patients. Auris Nasus Larynx 43:1–9
Passalacqua G, Guerra L, Pasquali M, Lombardi C, Canonica GW (2004) Efficacy and safety of sublingual immunotherapy. Ann Allergy Asthma Immunol 93:3–12
Moral A, Moreno V, Giron F, El-Qutob D, Moure JD, Alcantara M et al (2016) Adverse reactions and tolerability of high-dose sublingual allergen immunotherapy. J Asthma Allergy 9:129–133
Mosges R, Ritter B, Kayoko G, Allekotte S (2010) Carbamylated monomeric allergoids as a therapeutic option for sublingual immunotherapy of dust mite- and grass pollen-induced allergic rhinoconjunctivitis: a systematic review of published trials with a meta-analysis of treatment using Lais® tablets. Acta Dermatovenerol Alp Pannonica Adriat 19:3–10
Frati F, Scurati S, Puccinelli P, Justicia JL, Adamec T, Sieber HJ et al (2009) Development of an allergen extract for sublingual immunotherapy-evolution of Staloral. Expert Opin Biol Ther 9:1207–1215
Morjaria JB, Caruso M, Rosalia E, Russo C, Polosa R (2014) Preventing progression of allergic rhinitis to asthma. Curr Allergy Asthma Rep 14:412
Durham SR, Emminger W, Kapp A, de Monchy JG, Rak S, Scadding GK et al (2012) SQ-standardized sublingual grass immunotherapy: confirmation of disease modification 2 years after 3 years of treatment in a randomized trial. J Allergy Clin Immunol 129:717–725
Durham SR, Penagos M (2016) Sublingual or subcutaneous immunotherapy for allergic rhinitis? J Allergy Clin Immunol 137:339–349
Tabatabaian F, Casale TB (2015) Selection of patients for sublingual immunotherapy (SLIT) versus subcutaneous immunotherapy (SCIT). Allergy Asthma Proc 36:100–104
Lee S, Nolte H, Benninger MS (2015) Clinical considerations in the use of sublingual immunotherapy for allergic rhinitis. Am J Rhinol Allergy 29:106–114
Dretzke J, Meadows A, Novielli N, Huissoon A, Fry-Smith A, Meads C (2013) Subcutaneous and sublingual immunotherapy for seasonal allergic rhinitis: a systematic review and indirect comparison. J Allergy Clin Immunol 131:1361–1366
Di Bona D, Plaia A, Leto-Barone MS, La Piana S, Di Lorenzo G (2012) Efficacy of subcutaneous and sublingual immunotherapy with grass allergens for seasonal allergic rhinitis: a meta-analysis-based comparison. J Allergy Clin Immunol 130:1097–1107
Bergmann KC, Demoly P, Worm M, Fokkens WJ, Carrillo T, Tabar AI et al (2014) Efficacy and safety of sublingual tablets of house dust mite allergen extracts in adults with allergic rhinitis. J Allergy Clin Immunol 133:1608–1614
Okamoto Y, Okubo K, Yonekura S, Hashiguchi K, Goto M, Otsuka T et al (2015) Efficacy and safety of sublingual immunotherapy for two seasons in patients with Japanese cedar pollinosis. Int Arch Allergy Immunol 166:177–188
Maloney J, Bernstein DI, Nelson H, Creticos P, Hebert J, Noonan M et al (2014) Efficacy and safety of grass sublingual immunology tablet, MK-7243: a large randomized controlled trial. Ann Allergy Asthma Immunol 112:146–153
Allam JP, Novak N (2014) Immunological mechanisms of sublingual immunotherapy. Curr Opin Allergy Clin Immunol 14:564–569
Mascarell L, Lombardi V, Louise A, Saint-Lu N, Chabre H, Moussu H et al (2008) Oral dendritic cells mediate antigen-specific tolerance by stimulating TH1 and regulatory CD4 + T cells. J Allergy Clin Immunol 122:603–609
Allam JP, Novak N, Fuchs C, Asen S, Berge S, Appel T et al (2003) Characterization of dendritic cells from human oral mucosa: a new Langerhans’ cell type with high constitutive FcepsilonRI expression. J Allergy Clin Immunol 112:141–148
Akdis M, Akdis CA (2014) Mechanisms of allergen-specific immunotherapy: multiple suppressor factors at work in immune tolerance to allergens. J Allergy Clin Immunol 133:621–631
Makatsori M, Scadding GW, Lombardo C, Bisoffi G, Ridolo E, Durham SR et al (2014) Dropouts in sublingual allergen immunotherapy trials-a systematic review. Allergy 69:571–580
Senna G, Ridolo E, Calderon M, Lombardi C, Canonica GW, Passalacqua G (2009) Evidence of adherence to allergen-specific immunotherapy. Curr Opin Allergy Clin Immunol 9:544–548
Senna G, Lombardi C, Canonica GW, Passalacqua G (2010) How adherent to sublingual immunotherapy prescriptions are patients? The manufacturers’ viewpoint. J Allergy Clin Immunol 126:668–669
Chester JG, Bremberg MG, Reisacher WR (2016) Patient preferences for route of allergy immunotherapy: a comparison of four delivery methods. Int Forum Allergy Rhinol 6:454–459
Hsu NM, Reisacher WR (2012) A comparison of attrition rates in patients undergoing sublingual immunotherapy vs subcutaneous immunotherapy. Int Forum Allergy Rhinol 2:280–284
Incorvaia C, Mauro M, Ridolo E, Puccinelli P, Liuzzo M, Scurati S et al (2008) Patient’s compliance with allergen immunotherapy. Patient Prefer Adheren 2:247–251
Reisacher WR, Visaya JM (2013) Patient adherence to allergy immunotherapy. Curr Opin Otolaryngol Head Neck Surg 21:256–262
Kumar MS, Oh MS, Leader B, Rotella M, Stillman L, DelGaudio JM et al (2017) Perceived compliance and barriers to care in sublingual immunotherapy. Int Forum Allergy Rhinol 7:525–529
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Ethical approval
This study protocol was approved by the Institutional Review Board of Pusan National University Hospital (PNUHIRB 1804-013-066).
Informed consent
Written informed consent was not obtained from each parent prior to the patient’s participation in the study because of retrospective chart reviews.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, JA., Lee, YM., Yi, KI. et al. Comparative analysis of sublingual immunotherapy medicines for adherence and clinical outcomes. Eur Arch Otorhinolaryngol 277, 135–140 (2020). https://doi.org/10.1007/s00405-019-05656-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05656-6