Abstract
Introduction
Total laryngectomy (TL) with neck dissection (ND) is considered as crucial management for advanced-stage of laryngeal cancer. Shoulder dysfunction has long been recognized as a potential complication resulting from neck dissection. The aim of this study was to evaluate the effect of early prophylactic rehabilitation program in patients who underwent TL with ND.
Methods
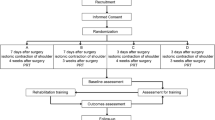
A prospective, nonrandomized design was used. Seventy-six participants who underwent TL with ND were assigned into either an intervention or a control group. The control group received current standard care with no formal shoulder exercise provided, while the intervention group attended early preventive rehabilitation lasting 12 weeks. Participants were assessed at baseline, and at 3 and 6 months after surgery. Measured outcomes included shoulder function and patient-reported quality of life. General linear models with repeated measures were used to examine outcome changes in both groups over the designated assessment intervals.
Results
Improvement in shoulder function and patient-reported quality of life were both statistically significant over time, with no significant difference between control or intervention groups, indicating little or no benefit of preventative intervention on shoulder function outcomes. Analysis involving five subscales and the summary score of the quality of life questionnaire had only statistically significant improvement over time for both the control or intervention groups, except for physical well-being domain which had statistical significance both over time and between the control and intervention groups.
Conclusion
In this study, preventative exercise program initiated immediately after surgery had a limited impact on both shoulder function and perceived quality of life.
Similar content being viewed by others
References
Patten C, Hillel AD (1993) The 11th nerve syndrome. Accessory nerve palsy or adhesive capsulitis? Arch Otolaryngol Head Neck Surg 119(2):215–220
Cappiello J, Piazza C, Nicolai P (2007) The spinal accessory nerve in head and neck surgery. Curr Opin Otolaryngol Head Neck Surg 15(2):107–111
Dijkstra PU, Wilgenc PCV, Buijsc RP et al (2001) Incidence of shoulder pain after neck dissection: a clinical explorative study for risk factors. Head Neck 23(11):947–953
van Wilgen CP, Dijkstra PU, van der Laan BF et al (2004) Shoulder complaints after nerve sparing neck dissections. Int J Oral Max Surg 33(3):253–257
Stuiver MM, van Wilgen CP, de Boer EM et al (2008) Impact of shoulder complaints after neck dissection on shoulder disability and quality of life. JAMA Otolaryngol Head Neck Surg 139(1):32–39
Lassig AAD, Duffy SA, Fowler KE et al (2008) The effect of neck dissection on quality of life after chemoradiation. Otolaryngol Head Neck Surg 139(4):511–518
Salerno G, Cavaliere M, Foglia A et al (2002) The 11th nerve syndrome in functional neck dissection. Laryngoscope 112(7):1299–1307
Lauchlan DT, Mccaul JA, Mccarron T et al (2011) An exploratory trial of preventative rehabilitation on shoulder disability and quality of life in patients following neck dissection surgery. Eur J Cancer Care 20(1):113–122
Mcgarvey AC, Hoffman GR, Osmotherly PG et al (2015) Maximizing shoulder function after accessory nerve injury and neck dissection surgery: a multicenter randomized controlled trial. Head Neck 37(7):1022–1031
Ahlberg A, Engström T, Nikolaidis P et al (2010) Early self-care rehabilitation of head and neck cancer patients. Acta Oto-Laryngol 131(5):552–561
Carvalho AP, Vital FM, Soares BG (2012) Exercise interventions for shoulder dysfunction in patients treated for head and neck cancer. Cochrane Database Syst Rev 4:CD008693
Mcneely ML, Parliament M, Courneya KS et al (2004) A pilot study of a randomized controlled trial to evaluate the effects of progressive resistance exercise training on shoulder dysfunction caused by spinal accessory neurapraxia/neurectomy in head and neck cancer survivors. Head Neck 26(6):518–530
McNeely ML, Parliament MB, Seikaly H et al (2008) Effect of exercise on upper extremity pain and dysfunction in head and neck cancer survivors. Cancer Am Cancer Soc 113(1):214–222
Hsu JE, Anakwenze OA, Warrender WJ et al (2011) Current review of adhesive capsulitis. J Shoulder Elb Surg 20(3):502–514
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214(214):160–164
Roy JS, Macdermid JC, Woodhouse LJ (2010) A systematic review of the psychometric properties of the Constant-Murley score. J Shoulder Elbow Surg 19(1):157–164
Razmjou H, Bean A, Macdermid JC, Van OV et al (2008) Convergent validity of the Constant-Murley outcome measure in patients with rotator cuff disease. Physiother Can 60(1):72–75
Norkin CC, White DJ (1985) Measurement of joint motion: a guide to goniometry, 1st edn. F. A. Davis, Philadelphia, p 149
Cella DF, Tulsky DS, Gray G et al (1993) The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 11(3):570–579
Bezjak A, O’Sullivan B, Redelmeier DA (2004) Interpreting differences in quality of life: the FACT-H&N in laryngeal cancer patients. Qual Life Res 13(4):725–733
Sobia B, Jennifer Geraldine D, David C et al (2015) Quality of life associated factors in head and neck cancer patients in a developing country using the FACT-H&N. J Cranio Maxill Surg 43(2):274–280
Piotrowicz E, Korzeniowskakubacka I, Chrapowicka A et al (2014) Feasibility of home-based cardiac telerehabilitation: results of TeleInterMed study. Cardiol J 21(5):539–546
Armfield NR, Gray LC, Smith AC (2012) Clinical use of Skype: a review of the evidence base. J Telemed Telecare 18(3):125–127
Tsai LL, Mcnamara RJ, Moddel C et al (2016) Home-based telerehabilitation via real-time videoconferencing improves endurance exercise capacity in patients with COPD: the randomized controlled TeleR Study. Respirology 22(4):699–707
Güldiken Y, Orhan KS, Demirel T et al (2005) Assessment of shoulder impairment after functional neck dissection: long-term results. Auris Nasus Larynx 32(4):387–391
Shah S, Harel G, Rosenfeld RM (2001) Short-term and long-term quality of life after neck dissection. Head Neck 23(11):954–961
Wade DT (2003) Outcome measures for clinical rehabilitation trials: impairment, function, quality of life, or value? Am J Phys Med Rehabil 82(10S):26–31
Ohura T, Nishiyama C, Nakayama T (2009) More appropriate, practical outcome measures in clinical trials for rehabilitation: a survey of medical literature from 1996 to 2005. Asian J Occup Therap 7(1):13–22
Funding
This study was supported by Shanghai Municipal Health Bureau Project for Youth (Grant No. 20134y161).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Peixia Wu declares that she has no conflict of interest. Zhengrong Peng declares that she has no conflict of interest. Junyi Chen declares that she has no conflict of interest. Yan Hu declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants included in this study.
Rights and permissions
About this article
Cite this article
Wu, P., Peng, Z., Chen, J. et al. Uncertain effect of preventative shoulder rehabilitation for patients who underwent total laryngectomy with neck dissection. Eur Arch Otorhinolaryngol 275, 795–801 (2018). https://doi.org/10.1007/s00405-018-4875-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-4875-x