Abstract
Objective
To explore the optimal time for initiating in vitro fertilization and embryo transfer (IVF-ET) in women with complete remission after fertility-sparing treatment for grade I endometrial cancer (EC) or atypical endometrial hyperplasia (AEH).
Patients and methods
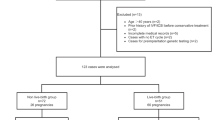
Young women who demonstrated complete remission after fertility-sparing treatment for grade I EC or AEH and underwent IVF-ET treatment were included. A generalized estimating equation (GEE) was used to compare the outcomes of controlled ovarian hyperstimulation (COH) and embryo transfer at different times after discontinuing high-dose progesterone therapy, and patients were divided into three groups: ≤ 3 months (time 1), 3–9 months (time 2) and > 9 months (time 3).
Results
Thirty-seven women with complete remission after fertility-sparing treatment for grade I EC or AEH underwent 75 IVF-ET cycles. Regarding initiation of COH, 10 cycles for time 1, 31 cycles for time 2 and 34 cycles for time 3 were included. The odds ratios (95% confidence intervals) for the number of available embryos at time 2 and time 3 were 1.82 (1.08–3.08) and 2.45 (1.39–4.33), and those for the number of high-quality embryos at time 2 and time 3 were, respectively, 3.64 (1.34–9.87) and 3.62 (1.10–11.91), compared with that at time 1. Nineteen (51.4%) women had at least one clinical pregnancy and 13 (35.1%) women had live births. During a median follow-up period of 51 months (range 5–168 months), 10 (27.0%) women had disease relapse, with a median interval of 15.5 months (range 5–104 months).
Conclusion
Initiating IVF-ET 3 months after ceasing high-dose progesterone therapy can lead to better outcomes of controlled ovarian hyperstimulation for women with endometrial cancer or atypical endometrial hyperplasia.
Similar content being viewed by others
References
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F et al (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66(2):115–132
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70(1):7–30
Lee NK, Cheung MK, Shin JY, Husain A, Teng NN, Berek JS et al (2007) Prognostic factors for uterine cancer in reproductive-aged women. Obstet Gynecol 109(3):655–662
Rodolakis A, Biliatis I, Morice P, Reed N, Mangler M, Kesic V et al (2015) European Society of Gynecological Oncology Task Force for fertility preservation: clinical recommendations for fertility sparing management in young endometrial cancer patients. Int J Gynecol Cancer 25(7):1258–1265
Colombo N, Creutzberg C, Amant F, Bosse T, González-Martín A, Ledermann J et al (2016) ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: diagnosis, treatment and follow-up. Ann Oncol 27(1):16–41
Gressel GM, Parkash V, Pal L (2015) Management options and fertility-preserving therapy for premenopausal endometrial hyperplasia and early-stage endometrial cancer. Int J Gynaecol Obstet 131(3):234–239
Zhou R, Yang Y, Lu Q, Wang J, Miao Y, Wang S et al (2015) Prognostic factors of oncological and reproductive outcomes in fertility-sparing treatment of complex atypical hyperplasia and low-grade endometrial cancer using oral progestin in Chinese patients. Gynecol Oncol 139(3):424–428
Inoue O, Hamatani T, Susumu N, Yamagami W, Ogawa S, Takemoto T et al (2016) Factors affecting pregnancy outcomes in young women treated with fertility-preserving therapy for well-differentiated endometrial cancer or atypical endometrial hyperplasia. Reprod Biol Endocrinol 14:2
Chao AS, Chao A, Wang CJ, Lai CH, Wang HS (2011) Obstetric outcomes of pregnancy after conservative treatment of endometrial cancer: case series and literature review. Taiwan J Obstet Gynecol 50(1):62–66
Gallos ID, Yap J, Rajkhowa M, Luesley DM, Coomarasamy A, Gupta JK (2012) Regression, relapse, and live birth rates with fertility-sparing therapy for endometrial cancer and atypical complex endometrial hyperplasia: a systematic review and meta analysis. Am J Obstet Gynecol 207(4):266.e1–12
Rivera R, Yacobson I, Grimes D (1999) The mechanism of action of hormonal contraceptives and intrauterine contraceptive devices. Am J Obstet Gynecol 181(5 Pt 1):1263–1269
Novikova OV, Nosov VB, Panov VA, Novikova EG, Krasnopolskaya KV, Andreeva YY et al (2021) Live births and maintenance with levonorgestrel IUD improve disease-free survival after fertility-sparing treatment of atypical hyperplasia and early endometrial cancer. Gynecol Oncol 161:152
Silva Idos S, Wark PA, McCormack VA, Mayer D, Overton C, Little V et al (2009) Ovulation-stimulation drugs and cancer risks: a long-term follow-up of a British cohort. Br J Cancer 100(11):1824–1831
Althuis MD, Moghissi KS, Westhoff CL, Scoccia B, Lamb EJ, Lubin JH et al (2005) Uterine cancer after use of clomiphene citrate to induce ovulation. Am J Epidemiol 161(7):607–615
Clark MK, Sowers M, Levy BT, Tenhundfeld P (2001) Magnitude and variability of sequential estradiol and progesterone concentrations in women using depot medroxyprogesterone acetate for contraception. Fertil Steril 75(5):871–877
Gordon GG, Southren AL, Tochimoto S, Olivo J, Altman K, Rand J et al (1970) Effect of medroxyprogesterone acetate (Provera) on the metabolism and biological activity of testosterone. J Clin Endocrinol Metab 30(4):449–456. https://doi.org/10.1210/jcem-30-4-449
Blossey HC, Wander HE, Koebberling J, Nagel GA (1984) Pharmacokinetic and pharmacodynamic basis for the treatment of metastatic breast cancer with high-dose medroxyprogesterone acetate. Cancer 54(6):1208–1215
Bassol S, Garza-Flores J, Cravioto MC, Diaz-Sanchez V, Fotherby K, Lichtenberg R et al (1984) Ovarian function following a single administration of depomedroxy progesterone acetate (DMPA) at different doses, development, and research training in human reproduction, World Health Organization, Geneva Switzerland. Fertil Steril 42(2):216–222
Wortsman J, Khan MS, Rosner W (1986) Suppression of testosterone-estradiol binding globulin by medroxyprogesterone acetate in polycystic ovary syndrome. Obstet Gynecol 67(5):705–709
Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH (2003) Classification and pharmacology of progestins. Maturitas 46(Suppl 1):S7–S16
Ata B, Capuzzo M, Turkgeldi E, Yildiz S, La Marca A (2021) Progestins for pituitary suppression during ovarian stimulation for ART: a comprehensive and systematic review including meta-analyses. Hum Reprod Update 27(1):48–66
Xi Q, Tao Y, Qiu M, Wang Y, Kuang Y (2020) Comparison between PPOS and GnRHa-long protocol in clinical outcome with the first IVF/ICSI cycle: a randomized clinical trial. Clin Epidemiol 12:261–272
Peters AE, Mihalas BP, Bromfield EG, Roman SD, Nixon B, Sutherland JM (2020) Autophagy in female fertility: a role in oxidative stress and aging. Antioxid Redox Signal 32(8):550–568
Koskas M, Uzan J, Luton D, Rouzier R, Daraï E (2014) Prognostic factors of oncologic and reproductive outcomes in fertility-sparing management of endometrial atypical hyperplasia and adenocarcinoma: systematic review and meta-analysis. Fertil Steril 101(3):785–794
Kim MJ, Choe SA, Kim MK, Yun BS, Seong SJ, Kim YS (2019) Outcomes of in vitro fertilization cycles following fertility-sparing treatment in stage IA endometrial cancer. Arch Gynecol Obstet 300(4):975–980
Du XG, Song XL, Li R, Li HZ, Qiao J (2018) Analysis of the clinical outcome of in vitro fertilization in infertility patients with conservative treatment of atypical endometrial hyperplasia and early well-differentiated endometrial adenocarcinoma. Reprod Contracept 38(9):741–747
Fujimoto A, Ichinose M, Harada M, Hirata T, Osuga Y, Fujii T (2014) The outcome of infertility treatment in patients undergoing assisted reproductive technology after conservative therapy for endometrial cancer. J Assist Reprod Gene 31(9):1189–1194
Ichinose M, Fujimoto A, Osuga Y, Minaguchi T, Kawana K, Yano T et al (2013) The influence of infertility treatment on the prognosis of endometrial cancer and atypical complex endometrial hyperplasia. Int J Gynecol Cancer 23(2):288–293
Chae SH, Shim SH, Lee SJ, Lee JY, Kim SN, Kang SB (2019) Pregnancy and oncologic outcomes after fertility-sparing management for early stage endometrioid endometrial cancer. Int J Gynecol Cancer 29(1):77–85
Park JY, Seong SJ, Kim TJ, Kim JW, Kim SM, Bae DS et al (2013) Pregnancy outcomes after fertility-sparing management in young women with early endometrial cancer. Obstet Gynecol 121(1):136–142
Funding
This work was supported by the National Key Technology R&D Program of China (no. 2019YFC1005200 and 2019YFC1005203).
Author information
Authors and Affiliations
Contributions
ZS: data curation, investigation, writing- original draft preparation; HL: software, validation, formal analysis; RZ: conceptualization, resources; ZX: data curation, investigation; JL: supervision, funding acquisition; QL: methodology, writing— reviewing and editing; HW: methodology, validation.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
This research study was conducted retrospectively from data obtained for clinical purposes. The Peking University People’s Hospital Research Ethics Committee has confirmed that no ethical approval is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Song, Z., Liu, H., Zhou, R. et al. The optimal time for the initiation of in vitro fertilization and embryo transfer among women with atypical endometrial hyperplasia and endometrial carcinoma receiving fertility-sparing treatment. Arch Gynecol Obstet 305, 1215–1223 (2022). https://doi.org/10.1007/s00404-021-06320-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06320-3