Abstract
Purpose
Success rates of any artificial reproduction techniques depend on a correct protocol for ovarian stimulation. This can be decided only by proper assessment of ovarian reserve before commencing ovarian stimulation. This study has been conducted to investigate the role of hormonal and functional biomarkers in the prediction of ovarian response.
Methods
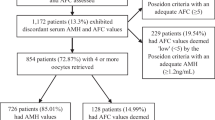
A total of 689 women between July 2012 and July 2013 undergoing IVF at Kocaeli University have been enrolled in the study. Patients have been categorized into three groups according to the number of oocytes retrieved: 0–3 oocytes (poor responders), 4–15 oocytes (normoresponders), and >16 oocytes (hyperresponders). Groups have been compared according to follicle-stimulating hormone (FSH), E2, luteinizing hormone (LH) levels, antral follicle counts, and E2 levels on hCG days. Furthermore, regression analysis has been performed with parameters such as age, FSH, LH, E2, anti-mullerian hormone (AMH) and antral follicle counts (AFC) that can affect the total number of oocytes retrieved and pregnancy rates and their interactions with each other have been investigated.
Results
FSH, age, hCG day LH level, cycle cancellation rate, total gonadotropin dose were significantly higher in the poor responder group, but in this group, AFC, AMH, hCG day E2 level, and the number of MII oocytes were significantly lower. Cut-off values of normal responders for FSH, AMH, and AFC were 8.43 area under curve [AUC: 0.541 (0.491–0.590)], 0.62 [AUC: 0.704 (0.638–0.764)], and 6 [AUC: 0.715 (0.667–0.760)], respectively. Cut-off values for the absolute poor response group (cycle cancellation) were 12.75 for FSH [AUC: 0.533 (0.49–0.57)], 0.23 for AMH [AUC: 0.678 (0.618–0.733)], and 6 for AFC [AUC: 0.576 (0.531–0.613)]. AMH and AFC were the best markers for the prediction of total oocyte count, independent of age, FSH, and LH levels.
Conclusions
AMH and AFC were found to be the best ovarian reserve tests that can determine the total oocyte count retrieved, without any significant effects on pregnancy rates.


Similar content being viewed by others
References
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB (2006) A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update 12(6):685–718
Sills ES, Alper MM, Walsh AP (2009) Ovarian reserve screening in infertility: practical applications and theoretical directions for research. Eur J Obstet Gynecol Reprod Biol 146(1):30–36. doi:10.1016/j.ejogrb.2009.05.008
Yang YS, Hur MH, Kim SY, Young K (2011) Correlation between sonographic and endocrine markers of ovarian aging as predictors for late menopausal transition. Menopause 18(2):138–145
Majumder K, Gelbaya TA, Laing I, Nardo LG (2010) The use of anti-Müllerian hormone and antral follicle count to predict the potential of oocytes and embryos. Eur J Obstet Gynecol Reprod Biol 150(2):166–170. doi:10.1016/j.ejogrb.2010.02.029
Kalaiselvi VS, P S, K P, Krishna GP (2012) The anti mullerian hormone—a novel marker for assessing the ovarian reserve in women with regular menstrual cycles. J Clin Diagn Res 6(10):1636–1639
Panchal S, Nagori C (2012) Comparison of anti-mullerian hormone and antral follicle count for assessment of ovarian reserve. J Hum Reprod Sci 5(3):274–278
Sahmay S, Cetin M, Ocal P, Kaleli S, Senol H, Birol F, Irez T (2011) Serum anti-Müllerian hormone level as a predictor of poor ovarian response in in vitro fertilization patients. Reprod Med Biol 10:9–14
Himabindu Y, Sriharibabu M, Gopinathan K, Satish U, Louis TF, Gopinath P (2013) Anti-mullerian hormone and antral follicle count as predictors of ovarian response in assisted reproduction. J Hum Reprod Sci 6(1):27–31. doi:10.4103/0974-1208.112377
Nelson SM, Yates RW, Lyall H, Jamieson M, Traynor I, Gaudoin M, Mitchell P, Ambrose P, Fleming R (2009) Anti-Müllerian hormone-based approach to controlled ovarian stimulation for assisted conception. Hum Reprod 24(4):867–875. doi:10.1093/humrep/den480
Fiçicioglu C, Kutlu T, Baglam E, Bakacak Z (2006) Early follicular antimüllerian hormone as an indicator of ovarian reserve. Fertil Steril 85(3):592–596
Alviggi C, Humaidan P, Ezcurra D (2012) Hormonal, functional and genetic biomarkers in controlled ovarian stimulation: tools for matching patients and protocols. Reprod Biol Endocrinol 10(9):1–9
Broer SL, Mol BW, Hendriks D, Broekmans FJ (2009) The role of antimullerian hormone in prediction of outcome after IVF: comparison with the antral follicle count. Fertil Steril 91:705–714
Celik H, Bıldırcın D, Güven D, Cetinkaya MB, Alper T, Batuoğlu AS (2012) Random anti-Müllerian hormone predicts ovarian response in women with high baseline follicle-stimulating hormone levels: anti-Müllerian hormone in poor responders in assisted reproductive treatment. J Assist Reprod Genet 29(8):797–802. doi:10.1007/s10815-012-9794-y (Epub 2012 May 10)
La Marca A (2013) Whatever its variability, antimüllerian hormone remains the most stable hormonal predictor. Fertil Steril 100(1):e1. doi:10.1016/j.fertnstert.2013.04.010
Gnoth C, Schuring AN, Friol K, Tigges J, Mallmann P, Godehardt E (2008) Relevance of anti-Mullerian hormone measurement in a routine IVF program. Hum Reprod 23:1359–1365
Ebner T, Sommergruber M, Moser M, Shebl O, Schreier-Lechner E, Tews G (2006) Basal level of anti-Müllerian hormone is associated with oocyte quality in stimulated cycles. Hum Reprod 21(8):2022–2026
Muttukrishna S, Suharjono H, McGarrigle H, Sathanandan M (2004) Inhibin B and anti-Mullerian hormone: markers of ovarian response in IVF/ICSI patients? BJOG 111(11):1248–1253
Nardo LG, Gelbaya TA, Wilkinson H, Roberts SA, Yates A, Pemberton P, Laing I (2009) Circulating basal anti- Müllerian hormone levels as predictor of ovarian response in women undergoing ovarian stimulation for in vitro fertilization. Fertil Steril 92(5):1586–1593. doi:10.1016/j.fertnstert.2008.08.127
Nakhuda GS, Sauer MV, Wang JG, Ferin M, Lobo RA (2007) Müllerian inhibiting substance is an accurate marker of ovarian response in women of advanced reproductive age undergoing IVF. Reprod Biomed Online 14(4):450–454
La Marca A, Giulini S, Tirelli A, Bertucci E, Marsella T, Xella S, Volpe A (2007) Anti-Müllerian hormone measurement on any day of the menstrual cycle strongly predicts ovarian response in assisted reproductive technology. Hum Reprod 22(3):766–771
Ben-Haroush A, Farhi J, Zahalka Y, Sapir O, Meizner I, Fisch B (2012) Correlations between antral follicle count and ultrasonographic ovarian parameters and clinical variables and outcomes in IVF cycles. Gynecol Endocrinol 28(6):432–435
Melo MA, Garrido N, Alvarez C, Bellver J, Meseguer M, Pellicer A, Remohí J (2009) Antral follicle count (AFC) can be used in the prediction of ovarian response but cannot predict the oocyte/embryo quality or the in vitro fertilization outcome in an egg donation program. Fertil Steril 91(1):148–156. doi:10.1016/j.fertnstert.2007.11.042
Frattarelli JL, Levi AJ, Miller BT, Segars JH (2003) A prospective assessment of the predictive value of basal antral follicles in in vitro fertilization cycles. Fertil Steril 80(2):350–355
Van Disseldorp J, Lambalk CB, Kwee J, Looman CW, Eijkemans MJ, Fauser BC, Broekmans FJ (2010) Comparison of inter- and intra-cycle variability of anti-Mullerian hormone and antral follicle counts. Hum Reprod 25(1):221–227. doi:10.1093/humrep/dep366
Panchal S, Nagori C (2012) Comparison of anti-mullerian hormone and antral follicle count for assessment of ovarian reserve. J Hum Reprod Sci 5(3):274–278. doi:10.4103/0974-1208.106340
Nahum R, Shifren JL, Chang Y, Leykin L, Isaacson K, Toth TL (2001) Antral follicle assessment as a tool for predicting outcome in IVF—is it a better predictor than age and FSH? J Assist Reprod Genet 18(3):151–155
Kunt C, Ozaksit G, Keskin Kurt R, Cakir Gungor AN, Kanat-Pektas M, Kilic S, Dede A (2011) Anti-Mullerian hormone is a better marker than inhibin B, follicle stimulating hormone, estradiol or antral follicle count in predicting the outcome of in vitro fertilization. Arch Gynecol Obstet 283(6):1415–1421. doi:10.1007/s00404-011-1889-7
Conflict of interest
There are no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vural, B., Cakiroglu, Y., Vural, F. et al. Hormonal and functional biomarkers in ovarian response. Arch Gynecol Obstet 289, 1355–1361 (2014). https://doi.org/10.1007/s00404-013-3132-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-013-3132-1