Abstract
Objective
To create a Proportional Hazards Model of prospective factors associated with time-to-vaginal-delivery (TTVD).
Methods
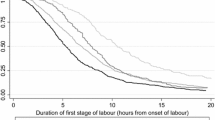
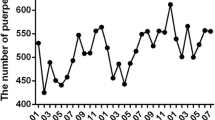
We analyzed a group of 144 women undergoing childbirth who received one out of two possible axial analgesia techniques, to find-out factors associated with TTVD. The patients were randomly assigned to receive either a levobupivacaine labor epidural (bolus concentration 0.25 % or less; infusion concentration 0.125 % or less) or a combined spinal–epidural procedure (morphine 0.20 mg, fentanyl 25 µg and hyperbaric bupivacaine 2.5 mg as spinal components) for labor analgesia. The factors initially chosen were: mother age, height and weight, parity, gestational age, newborn weight, type of labor, analgesic procedure, levobupivacaine and fentanyl doses, Bromage scale, pain Numeric Rating Scale, and a satisfaction interview. Cesarean section was the censored variable in our model. A systematic multivariate Cox regression was performed.
Results
Our Final Model stated that nulliparous women had 2.5 times more chances of having longer TTVD than primiparous (p < 0.001, CI 1.76–3.8), and 3.4 times more (p = 0.015, CI 1.27–9.25) than multiparous. Women with oxytocin-augmented labor had 2.05 times more chances (p = 0.001, CI 1.31–3.22) of having longer TTVD than patients without oxytocin. An induced partum had 3.8 times more chances (p < 0.001, CI 2.09–6.8) of having longer TTVD compared to a spontaneous partum.
Conclusion
Parity, labor augmentation, induction of labor and fetal weight determine TTVD; axial analgesia-related factors do not contribute to the model.


Similar content being viewed by others
References
Friedman E (1954) The graphic analysis of labor. Am J Obstet Gynecol 68:1568–1575
Zhang J, Troendle JF, Yancey MK (2002) Reassessing the labor curve in nulliparous women. Am J Obstet Gynecol 187:824–828
Debiec J, Conell-Price J, Evansmith J, Shafer LS, Flood P (2009) Mathematical modeling of the pain and progress of the first stage of nulliparous labor. Anesthesiology 111:1093–1110
Anim-Somuah M, Smyth RMD, Howell CJ (2005) Epidural versus non-epidural or no analgesia in labour. Cochrane Database of Systematic Reviews, Issue 4
Hawkins JL, Arens JF, Bucklin BA et al. for the American Society of Anesthesiologists Task Force on Obstetric Anesthesia (2007) Practice guidelines for obstetric anesthesia. Anesthesiology 106:843–863
Pascual-Ramírez J, Haya J, Perez-Lopez F, Gil-Trujillo S, Garrido-Esteban RA, Bernal G (2011) Effect of combined spinal–epidural analgesia versus epidural analgesia on labor and delivery duration. Int J Gynecol Obstet 114(3):246–250
Wang F, Shen X, Guo X, Peng Y, Gu X (2009) Epidural analgesia in the latent phase of labor and the risk of cesarean delivery: a five-year randomized controlled trial. Anesthesiology 111:871–880
Abouleish E, Rawal N, Shaw J, Rashad MN, Lorenz T (1990) Subarachnoid morphine prolongs labor compared to epidural bupivacaine. Anesth Analg 70:S4
Culha HT, Ozdamar D, Toker K, Solak M (2007) The effects of various doses of intrathecal morphine in addition with ropivacaine in combined spinal-epidural technique for labour analgesia. Agri. 19:16–23
Hess PH, Vasudevan A, Snowman C, Pratt SD (2003) Small dose bupivacaine–fentanyl spinal analgesia combined with morphine for labor. Anesth Analg 97:247–252
Simmons SW, Cyna AM, Dennis AT, Hughes D (2007) Combined spinal–epidural versus epidural analgesia in labour. Cochrane Database of Systematic Reviews, Issue 3
Tsen LC, Thue B, Datta S, Segal S (1999) Is combined spinal–epidural analgesia associated with more rapid cervical dilation in nulliparous patients when compared with conventional epidural analgesia? Anesthesiology 91:920–925
Bhagwat AG, Dua CK, Saxena KN, Srinivasan S, Dua K (2008) Comparison of combined spinal epidural technique and low dose epidural technique in progress of labour. Indian J Anaesth 52:282–287
Dunn SM, Connelly NR, Steinberg RB, Lewis TJ, Bazzell M, Klatt JL et al (1998) Intrathecal sufentanil versus epidural lidocaine with epinephrine and sufentanil for early labor analgesia. Anesth Analg 87:331–335
Roux M, Wattrisse G, Tai RB, Dufossez F, Krivosic-Horber R (1999) Analgesie obstetricale: analgesie peridurale versis analgesie rachidienne et peridurale combine. Annales Francaises d’Anesthesie et de Reanimation 18:487–498
Wong CA, Scavone BM, Paceman AM, McCarthy RJ, Sullivan JT, Diaz NT et al (2005) The risk of cesarean delivery with neuraxial analgesia given early versus late in labor. N Engl J Med 352:655–665
Nesheim BI (1988) Duration of labor. An analysis of influencing factors. Acta Obstet Gynecol Scand 67:121–124
Vahratian A, Zhang J, Troendle JF, Savitz DA, Siega-Riz AM (2004) Maternal prepregnancy overweight and obesity and the pattern of labor progression in term nulliparous women. Obstet Gynecol 104:943–951
Vahratian A, Hoffman MK, Troendle JF, Zhang J (2006) The influence of parity on course of labor in a contemporary population. Birth Issues Perinatal care 33:1–12
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pascual-Ramírez, J., Haya, J., Pérez-López, F. et al. Type of axial analgesia does not influence time to vaginal delivery in a Proportional Hazards Model. Arch Gynecol Obstet 286, 873–880 (2012). https://doi.org/10.1007/s00404-012-2360-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2360-0