Abstract
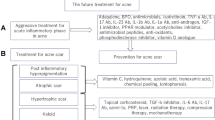
Acne vulgaris is a cutaneous chronic inflammatory disorder with complex pathogenesis. Four factors play vital roles in acne pathophysiology: hyperseborrhea and dysseborrhea, altered keratinization of the pilosebaceous duct, Cutibacterium acnes (C. acnes) and inflammation. The main hormones responsible for the development of acne vulgaris include androgens, insulin and insulin-like growth factor-1. Other factors involved in this process are corticotropin-releasing hormone, α-melanocyte-stimulating hormone and substance P. Wnt/β-catenin signaling pathway, phosphoinositide 3-kinase (PI3K)/Akt pathway, mitogen-activated protein kinase pathway, adenosine 5′-monophosphate-activated protein kinase pathway and nuclear factor kappa B pathway participate in the modulation of sebocyte, keratinocyte and inflammatory cell (e.g. lymphocytes, monocytes, macrophages, neutrophils) activity. Among all the triggers and pathways mentioned above, IGF-1-induced PI3K/Akt/Forkhead box protein O1/mammalian target of rapamycin (mTOR) C1 pathway is the most important signaling responsible for acne pathogenesis. Commonly used anti-acne agents include retinoids, benzoyl peroxide, antibiotics and hormonal agents (e.g. spironolactone, combination oral contraceptive and flutamide). New approaches including peroxisome proliferator-activated receptor γ modifier, melanocortin receptor antagonists, epigallocatechin-3-gallate, metformin, olumacostat glasaretil, stearoyl-CoA desaturase inhibitor omiganan pentahydrochloride, KDPT, afamelanotide, apremilast and biologics have been developed as promising treatments for acne vulgaris. Although these anti-acne agents have various pharmacological effects against the diverse pathogenesis of acne, all of them have a synergistic mode of action, the attenuation of Akt/mTORC1 signaling and enhancement of p53 signal transduction. In addition to drug therapy, diet with no hyperglycemic carbohydrates, no milk and dairy products is also beneficial for treatment of acne.




Similar content being viewed by others
References
Agak GW, Qin M, Nobe J, Kim MH, Krutzik SR, Tristan GR, Elashoff D, Garban HJ, Kim J (2014) Propionibacterium acnes induces an IL-17 response in acne vulgaris that is regulated by vitamin A and vitamin D. J Investig Dermatol 134:366–373. https://doi.org/10.1038/jid.2013.334
Agamia NF, Abdallah DM, Sorour O, Mourad B, Younan DN (2016) Skin expression of mammalian target of rapamycin and forkhead box transcription factor O1, and serum insulin-like growth factor-1 in patients with acne vulgaris and their relationship with diet. Br J Dermatol 174:1299–1307. https://doi.org/10.1111/bjd.14409
Agamia NF, Hussein OM, Abdelmaksoud RE, Abdalla DM, Talaat IM, Zaki EI, El Tawdy A, Melnik BC (2018) Effect of oral isotretinoin on the nucleo-cytoplasmic distribution of FoxO1 and FoxO3 proteins in sebaceous glands of patients with acne vulgaris. Exp Dermatol 27:1344–1351. https://doi.org/10.1111/exd.13787
Aghasi M, Golzarand M, Shab-Bidar S, Aminianfar A, Omidian M, Taheri F (2018) Dairy intake and acne development: a meta-analysis of observational studies. Clin Nutr (Edinburgh, Scotland). https://doi.org/10.1016/j.clnu.2018.04.015
Akamatsu H, Horio T, Hattori K (2003) Increased hydrogen peroxide generation by neutrophils from patients with acne inflammation. Int J Dermatol 42:366–369. https://doi.org/10.1046/j.1365-4362.2003.01540.x
Arowojolu AO, Gallo MF, Lopez LM, Grimes DA (2012) Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004425.pub6
Barnard E, Shi B, Kang D, Craft N, Li H (2016) The balance of metagenomic elements shapes the skin microbiome in acne and health. Sci Rep 6:39491. https://doi.org/10.1038/srep39491
Ben-Amitai D, Laron Z (2011) Effect of insulin-like growth factor-1 deficiency or administration on the occurrence of acne. J Eur Acad Dermatol Venereol 25:950–954. https://doi.org/10.1111/j.1468-3083.2010.03896.x
Bissonnette R, Poulin Y, Drew J, Hofland H, Tan J (2017) Olumacostat glasaretil, a novel topical sebum inhibitor, in the treatment of acne vulgaris: a phase IIa, multicenter, randomized, vehicle-controlled study. J Am Acad Dermatol 76:33–39. https://doi.org/10.1016/j.jaad.2016.08.053
Bohm M, Ehrchen J, Luger TA (2014) Beneficial effects of the melanocortin analogue Nle4-D-Phe7-alpha-MSH in acne vulgaris. J Eur Acad Dermatol Venereol 28:108–111. https://doi.org/10.1111/j.1468-3083.2012.04658.x
Bohm M, Schiller M, Stander S, Seltmann H, Li Z, Brzoska T, Metze D, Schioth HB, Skottner A, Seiffert K, Zouboulis CC, Luger TA (2002) Evidence for expression of melanocortin-1 receptor in human sebocytes in vitro and in situ. J Investig Dermatol 118:533–539. https://doi.org/10.1046/j.0022-202x.2001.01704.x
Bohrer LR, Liu P, Zhong J, Pan Y, Angstman J, Brand LJ, Dehm SM, Huang H (2013) FOXO1 binds to the TAU5 motif and inhibits constitutively active androgen receptor splice variants. Prostate 73:1017–1027. https://doi.org/10.1002/pros.22649
Boisselle A, Dionne FT, Tremblay RR (1979) Interaction of spironolactone with rat skin androgen receptor. Can J Biochem 57:1042–1046. https://doi.org/10.1139/o79-131
Bowe WP, Leyden JJ, Crerand CE, Sarwer DB, Margolis DJ (2007) Body dysmorphic disorder symptoms among patients with acne vulgaris. J Am Acad Dermatol 57:222–230. https://doi.org/10.1016/j.jaad.2007.03.030
Burkhart CG, Burkhart CN (2007) Expanding the microcomedone theory and acne therapeutics: Propionibacterium acnes biofilm produces biological glue that holds corneocytes together to form plug. J Am Acad Dermatol 57:722–724. https://doi.org/10.1016/j.jaad.2007.05.013
Burkhart CN, Burkhart CG (2006) Genome sequence of Propionibacterium acnes reveals immunogenic and surface-associated genes confirming existence of the acne biofilm. Int J Dermatol 45:872. https://doi.org/10.1111/j.1365-4632.2006.02734.x
Burris J, Rietkerk W, Woolf K (2013) Acne: the role of medical nutrition therapy. J Acad Nutr Diet 113:416–430. https://doi.org/10.1016/j.jand.2012.11.016
Chen CC, Jeon SM, Bhaskar PT, Nogueira V, Sundararajan D, Tonic I, Park Y, Hay N (2010) FoxOs inhibit mTORC1 and activate Akt by inducing the expression of Sestrin3 and Rictor. Dev Cell 18:592–604. https://doi.org/10.1016/j.devcel.2010.03.008
Claudel JP, Auffret N, Leccia MT, Poli F, Dreno B (2018) Acne and nutrition: hypotheses, myths and facts. J Eur Acad Dermatol Venereol 32:1631–1637. https://doi.org/10.1111/jdv.14998
Coenye T, Peeters E, Nelis HJ (2007) Biofilm formation by Propionibacterium acnes is associated with increased resistance to antimicrobial agents and increased production of putative virulence factors. Res Microbiol 158:386–392. https://doi.org/10.1016/j.resmic.2007.02.001
Cordain L, Lindeberg S, Hurtado M, Hill K, Eaton SB, Brand-Miller J (2002) Acne vulgaris: a disease of Western civilization. Arch Dermatol 138:1584–1590. https://doi.org/10.1001/archderm.138.12.1584
Cottle DL, Kretzschmar K, Schweiger PJ, Quist SR, Gollnick HP, Natsuga K, Aoyagi S, Watt FM (2013) c-MYC-induced sebaceous gland differentiation is controlled by an androgen receptor/p53 axis. Cell Rep 3:427–441. https://doi.org/10.1016/j.celrep.2013.01.013
Cunliffe WJ, Dodman B, Ead R (1978) Benzoyl peroxide in acne. Pract 220:479–482
Cunliffe WJ, Holland DB, Clark SM, Stables GI (2000) Comedogenesis: some new aetiological, clinical and therapeutic strategies. Br J Dermatol 142:1084–1091. https://doi.org/10.1046/j.1365-2133.2000.03531.x
Czernielewski J, Michel S, Bouclier M, Baker M, Hensby JC (2001) Adapalene biochemistry and the evolution of a new topical retinoid for treatment of acne. J Eur Acad Dermatol Venereol 15(Suppl 3):5–12. https://doi.org/10.1046/j.0926-9959.2001.00006.x
Dai R, Hua W, Chen W, Xiong L, Li L (2018) The effect of milk consumption on acne: a meta-analysis of observational studies. J Eur Acad Dermatol Venereol 32:2244–2253. https://doi.org/10.1111/jdv.15204
Day LE (1966) Tetracycline inhibition of cell-free protein synthesis. II. Effect of the binding of tetracycline to the components of the system. J Bacteriol 92:197–203. https://doi.org/10.1016/0006-291X(80)91307-8
Denda M, Fuziwara S, Inoue K (2003) Influx of calcium and chloride ions into epidermal keratinocytes regulates exocytosis of epidermal lamellar bodies and skin permeability barrier homeostasis. J Eur Acad Dermatol Venereol 121:362–367. https://doi.org/10.1046/j.1523-1747.2003.12367.x
Denda M, Fuziwara S, Inoue K (2004) Association of cyclic adenosine monophosphate with permeability barrier homeostasis of murine skin. J Investig Dermatol 122:140–146. https://doi.org/10.1046/j.0022-202X.2003.22115.x
Donlan RM (2001) Biofilm formation: a clinically relevant microbiological process. Clin Infect Dis 33:1387–1392. https://doi.org/10.1086/322972
Dreno B, Pecastaings S, Corvec S, Veraldi S, Khammari A, Roques C (2018) Cutibacterium acnes (Propionibacterium acnes) and acne vulgaris: a brief look at the latest updates. J Eur Acad Dermatol Venereol 32(Suppl 2):5–14. https://doi.org/10.1111/jdv.15043
Eisinger M, Li WH, Anthonavage M, Pappas A, Zhang L, Rossetti D, Huang Q, Seiberg M (2011) A melanocortin receptor 1 and 5 antagonist inhibits sebaceous gland differentiation and the production of sebum-specific lipids. J Dermatol Sci 63:23–32. https://doi.org/10.1016/j.jdermsci.2011.04.001
Eller MS, Yaar M, Ostrom K, Harkness DD, Gilchrest BA (1995) A role for interleukin-1 in epidermal differentiation: regulation by expression of functional versus decoy receptors. J Cell Sci 108(Pt 8):2741–2746. https://doi.org/10.1083/jcb.130.4.1005
Esterly NB, Furey NL, Flanagan LE (1978) The effect of antimicrobial agents on leukocyte chemotaxis. J Investig Dermatol 70:51–55. https://doi.org/10.1111/1523-1747.ep12543487
Fabbrocini G, Izzo R, Faggiano A, Del Prete M, Donnarumma M, Marasca C, Marciello F, Savastano R, Monfrecola G, Colao A (2016) Low glycaemic diet and metformin therapy: a new approach in male subjects with acne resistant to common treatments. Clinical Exp Dermatol 41:38–42. https://doi.org/10.1111/ced.12673
Fan W, Yanase T, Morinaga H, Okabe T, Nomura M, Daitoku H, Fukamizu A, Kato S, Takayanagi R, Nawata H (2007) Insulin-like growth factor 1/insulin signaling activates androgen signaling through direct interactions of Foxo1 with androgen receptor. J Biol Chem 282:7329–7338. https://doi.org/10.1074/jbc.M610447200
Farrah G, Tan E (2016) The use of oral antibiotics in treating acne vulgaris: a new approach. Dermatol Ther 29:377–384. https://doi.org/10.1111/dth.12370
Fitz-Gibbon S, Tomida S, Chiu BH, Nguyen L, Du C, Liu M, Elashoff D, Erfe MC, Loncaric A, Kim J, Modlin RL, Miller JF, Sodergren E, Craft N, Weinstock GM, Li H (2013) Propionibacterium acnes strain populations in the human skin microbiome associated with acne. J Investig Dermatol 133:2152–2160. https://doi.org/10.1038/jid.2013.21
Fulton JE Jr, Farzad-Bakshandeh A, Bradley S (1974) Studies on the mechanism of action to topical benzoyl peroxide and vitamin A acid in acne vulgaris. J Cutan Pathol 1:191–200. https://doi.org/10.1111/j.1600-0560.1974.tb00628.x
Ganceviciene R, Graziene V, Bohm M, Zouboulis CC (2007) Increased in situ expression of melanocortin-1 receptor in sebaceous glands of lesional skin of patients with acne vulgaris. Exp Dermatol 16:547–552. https://doi.org/10.1111/j.1600-0625.2007.00565.x
Ganceviciene R, Graziene V, Fimmel S, Zouboulis CC (2009) Involvement of the corticotropin-releasing hormone system in the pathogenesis of acne vulgaris. Br J Dermatol 160:345–352. https://doi.org/10.1111/j.1365-2133.2008.08959.x
Gille J, Paxton LL, Lawley TJ, Caughman SW, Swerlick RA (1997) Retinoic acid inhibits the regulated expression of vascular cell adhesion molecule-1 by cultured dermal microvascular endothelial cells. J Clin Investig 99:492–500. https://doi.org/10.1172/jci119184
Gollnick HP, Zouboulis CC, Akamatsu H, Kurokawa I, Schulte A (1991) Pathogenesis and pathogenesis related treatment of acne. J Dermatol 18:489–499. https://doi.org/10.1111/j.1346-8138.1991.tb03122.x
Graham GM, Farrar MD, Cruse-Sawyer JE, Holland KT, Ingham E (2004) Proinflammatory cytokine production by human keratinocytes stimulated with Propionibacterium acnes and P. acnes GroEL. Br J Dermatol 150:421–428. https://doi.org/10.1046/j.1365-2133.2004.05762.x
Grange PA, Chereau C, Raingeaud J, Nicco C, Weill B, Dupin N, Batteux F (2009) Production of superoxide anions by keratinocytes initiates P. acnes-induced inflammation of the skin. PLoS Pathog 5:e1000527. https://doi.org/10.1371/journal.ppat.1000527
Guevara-Aguirre J, Balasubramanian P, Guevara-Aguirre M, Wei M, Madia F, Cheng CW, Hwang D, Martin-Montalvo A, Saavedra J, Ingles S, de Cabo R, Cohen P, Longo VD (2011) Growth hormone receptor deficiency is associated with a major reduction in pro-aging signaling, cancer, and diabetes in humans. Sci Transl Med 3:70ra13. https://doi.org/10.1126/scitranslmed.3001845
Guy R, Green MR, Kealey T (1996) Modeling acne in vitro. J Investig Dermatol 106:176–182. https://doi.org/10.1111/1523-1747.ep12329907
Hancock RE, Rozek A (2002) Role of membranes in the activities of antimicrobial cationic peptides. FEMS Microbiol Lett 206:143–149. https://doi.org/10.1111/j.1574-6968.2002.tb11000.x
Harper JC (2009) Should dermatologists prescribe hormonal contraceptives for acne? Dermatol Ther 22:452–457. https://doi.org/10.1111/j.1529-8019.2009.01261.x
He TC, Sparks AB, Rago C, Hermeking H, Zawel L, da Costa LT, Morin PJ, Vogelstein B, Kinzler KW (1998) Identification of c-MYC as a target of the APC pathway. Science 281:1509–1512. https://doi.org/10.1126/science.281.5382.1509
Higaki S, Kitagawa T, Kagoura M, Morohashi M, Yamagishi T (2000) Correlation between Propionibacterium acnes biotypes, lipase activity and rash degree in acne patients. J Dermatol 27:519–522. https://doi.org/10.1111/j.1346-8138.2000.tb02219.x
Hobbs CJ, Plymate SR, Rosen CJ, Adler RA (1993) Testosterone administration increases insulin-like growth factor-I levels in normal men. The Journal of clinical endocrinology metabolism 77:776–779. https://doi.org/10.1210/jcem.77.3.7690364
Holland C, Mak TN, Zimny-Arndt U, Schmid M, Meyer TF, Jungblut PR, Bruggemann H (2010) Proteomic identification of secreted proteins of Propionibacterium acnes. BMC microbiology 10:230. https://doi.org/10.1186/1471-2180-10-230
Hunt DW, Winters GC, Brownsey RW, Kulpa JE, Gilliland KL, Thiboutot DM, Hofland HE (2017) Inhibition of Sebum Production with the Acetyl Coenzyme A Carboxylase Inhibitor Olumacostat Glasaretil. J Investig Dermatol 137:1415–1423. https://doi.org/10.1016/j.jid.2016.12.031
Im M, Kim SY, Sohn KC, Choi DK, Lee Y, Seo YJ, Kim CD, Hwang YL, Zouboulis CC, Lee JH (2012) Epigallocatechin-3-gallate suppresses IGF-I-induced lipogenesis and cytokine expression in SZ95 sebocytes. J Investig Dermatol 132:2700–2708. https://doi.org/10.1038/jid.2012.202
Jahns AC, Lundskog B, Ganceviciene R, Palmer RH, Golovleva I, Zouboulis CC, McDowell A, Patrick S, Alexeyev OA (2012) An increased incidence of Propionibacterium acnes biofilms in acne vulgaris: a case-control study. Br J Dermatol 167:50–58. https://doi.org/10.1111/j.1365-2133.2012.10897.x
Jappe U, Ingham E, Henwood J, Holland KT (2002) Propionibacterium acnes and inflammation in acne; P. acnes has T-cell mitogenic activity. Br J Dermatol 146:202–209. https://doi.org/10.1046/j.1365-2133.2002.04602.x
Jugeau S, Tenaud I, Knol AC, Jarrousse V, Quereux G, Khammari A, Dreno B (2005) Induction of toll-like receptors by Propionibacterium acnes. Br J Dermatol 153:1105–1113. https://doi.org/10.1111/j.1365-2133.2005.06933.x
Juhl CR, Bergholdt HKM, Miller IM, Jemec GBE, Kanters JK, Ellervik C (2018) Dairy intake and acne vulgaris: a systematic review and meta-analysis of 78,529 children, adolescents, and young adults. Nutrients. https://doi.org/10.3390/nu10081049
Kamei Y, Miura S, Suganami T, Akaike F, Kanai S, Sugita S, Katsumata A, Aburatani H, Unterman TG, Ezaki O, Ogawa Y (2008) Regulation of SREBP1c gene expression in skeletal muscle: role of retinoid X receptor/liver X receptor and forkhead-O1 transcription factor. Endocrinology 149:2293–2305. https://doi.org/10.1210/en.2007-1461
Kang BY, Chung SW, Kim SH, Kang SN, Choe YK, Kim TS (2000) Retinoid-mediated inhibition of interleukin-12 production in mouse macrophages suppresses Th1 cytokine profile in CD4(+) T cells. Br J Pharmacol 130:581–586. https://doi.org/10.1038/sj.bjp.0703345
Katsuta Y, Iida T, Hasegawa K, Inomata S, Denda M (2009) Function of oleic acid on epidermal barrier and calcium influx into keratinocytes is associated with N-methyl D-aspartate-type glutamate receptors. Br J Dermatol 160:69–74. https://doi.org/10.1111/j.1365-2133.2008.08860.x
Kim H, Moon SY, Sohn MY, Lee WJ (2017) Insulin-like growth factor-1 increases the expression of inflammatory biomarkers and sebum production in cultured sebocytes. Ann Dermatol 29:20–25. https://doi.org/10.5021/ad.2017.29.1.20
Kim J, Ochoa MT, Krutzik SR, Takeuchi O, Uematsu S, Legaspi AJ, Brightbill HD, Holland D, Cunliffe WJ, Akira S, Sieling PA, Godowski PJ, Modlin RL (2002) Activation of toll-like receptor 2 in acne triggers inflammatory cytokine responses. J Immunol 169:1535–1541. https://doi.org/10.4049/jimmunol.169.3.1535
Kistowska M, Meier B, Proust T, Feldmeyer L, Cozzio A, Kuendig T, Contassot E, French LE (2015) Propionibacterium acnes promotes Th17 and Th17/Th1 responses in acne patients. J Investig Dermatol 135:110–118. https://doi.org/10.1038/jid.2014.290
Klinger B, Anin S, Silbergeld A, Eshet R, Laron Z (1998) Development of hyperandrogenism during treatment with insulin-like growth factor-I (IGF-I) in female patients with Laron syndrome. Clin Endocrinol 48:81–87. https://doi.org/10.1046/j.1365-2265.1998.00356.x
Knaggs HE, Layton AM, Morris C, Wood EJ, Holland DB, Cunliffe WJ (1994) Investigation of the expression of the extracellular matrix glycoproteins tenascin and fibronectin during acne vulgaris. Br J Dermatol 130:576–582. https://doi.org/10.1111/j.1365-2133.1994.tb13102.x
Krautheim A, Gollnick H (2003) Transdermal penetration of topical drugs used in the treatment of acne. Clin Pharmacokinet 42:1287–1304. https://doi.org/10.2165/00003088-200342140-00005
Kretzschmar K, Cottle DL, Schweiger PJ, Watt FM (2015) The androgen receptor antagonizes Wnt/beta-catenin signaling in epidermal stem cells. J Investig Dermatol 135:2753–2763. https://doi.org/10.1038/jid.2015.242
Lang S, Palmer M (2003) Characterization of Streptococcus agalactiae CAMP factor as a pore-forming toxin. J Biol Chem 278:38167–38173. https://doi.org/10.1074/jbc.M303544200
Lee JK, Smith AD (2017) Metformin as an adjunct therapy for the treatment of moderate to severe acne vulgaris. Dermatol Online J 23:5–6
Lee WL, Shalita AR, Suntharalingam K, Fikrig SM (1982) Neutrophil chemotaxis by Propionibacterium acnes lipase and its inhibition. Infect Immunity 35:71–78
Leyden JJ, Shalita A, Thiboutot D, Washenik K, Webster G (2005) Topical retinoids in inflammatory acne: a retrospective, investigator-blinded, vehicle-controlled, photographic assessment. Clin Ther 27:216–224. https://doi.org/10.1016/j.clinthera.2005.02.009
Liu PT, Krutzik SR, Kim J, Modlin RL (2005) Cutting edge: all-trans retinoic acid down-regulates TLR2 expression and function. J Immunol 174:2467–2470. https://doi.org/10.4049/jimmunol.174.5.2467
Lomholt HB, Scholz CFP, Bruggemann H, Tettelin H, Kilian M (2017) A comparative study of Cutibacterium (Propionibacterium) acnes clones from acne patients and healthy controls. Anaerobe 47:57–63. https://doi.org/10.1016/j.anaerobe.2017.04.006
Lovaszi M, Mattii M, Eyerich K, Gacsi A, Csanyi E, Kovacs D, Ruhl R, Szegedi A, Kemeny L, Stahle M, Zouboulis CC, Eyerich S, Torocsik D (2017) Sebum lipids influence macrophage polarization and activation. Br J Dermatol 177:1671–1682. https://doi.org/10.1111/bjd.15754
Ma Q, Fu W, Li P, Nicosia SV, Jenster G, Zhang X, Bai W (2009) FoxO1 mediates PTEN suppression of androgen receptor N- and C-terminal interactions and coactivator recruitment. Mol Endocrinol (Baltimore Md) 23:213–225. https://doi.org/10.1210/me.2008-0147
Maeda T (1991) An electron microscopic study of experimentally-induced comedo and effects of vitamin A acid on comedo formation. J Dermatol 18:397–407. https://doi.org/10.1111/j.1346-8138.1991.tb03105.x
Makris G, Wright JD, Ingham E, Holland KT (2004) The hyaluronate lyase of Staphylococcus aureus—a virulence factor? Microbiology 150:2005–2013. https://doi.org/10.1099/mic.0.26942-0
Mastrofrancesco A, Kokot A, Eberle A, Gibbons NC, Schallreuter KU, Strozyk E, Picardo M, Zouboulis CC, Luger TA, Bohm M (2010) KdPT, a tripeptide derivative of alpha-melanocyte-stimulating hormone, suppresses IL-1 beta-mediated cytokine expression and signaling in human sebocytes. J Immunol 185:1903–1911. https://doi.org/10.4049/jimmunol.0902298
Mattii M, Lovaszi M, Garzorz N, Atenhan A, Quaranta M, Lauffer F, Konstantinow A, Kupper M, Zouboulis CC, Kemeny L, Eyerich K, Schmidt-Weber CB, Torocsik D, Eyerich S (2018) Sebocytes contribute to skin inflammation by promoting the differentiation of T helper 17 cells. Br J Dermatol 178:722–730. https://doi.org/10.1111/bjd.15879
Meingassner JG, Aschauer H, Winiski AP, Dales N, Yowe D, Winther MD, Zhang Z, Stutz A, Billich A (2013) Pharmacological inhibition of stearoyl CoA desaturase in the skin induces atrophy of the sebaceous glands. J Investig Dermatol 133:2091–2094. https://doi.org/10.1038/jid.2013.89
Melnik B (2012) Dietary intervention in acne: attenuation of increased mTORC1 signaling promoted by Western diet. Dermato-endocrinology 4:20–32. https://doi.org/10.4161/derm.19828
Melnik BC (2015) Linking diet to acne metabolomics, inflammation, and comedogenesis: an update. Clin Cosmet Investig Dermatol 8:371–388. https://doi.org/10.2147/ccid.s69135
Melnik BC (2015) Milk—a nutrient system of mammalian evolution promoting mTORC1-dependent translation. Int J Mol Sci 16:17048–17087. https://doi.org/10.3390/ijms160817048
Melnik BC (2017) Milk disrupts p53 and DNMT1, the guardians of the genome: implications for acne vulgaris and prostate cancer. Nutr Metab 14:55. https://doi.org/10.1186/s12986-017-0212-4
Melnik BC (2017) p53: key conductor of all anti-acne therapies. J Transl Med 15:195. https://doi.org/10.1186/s12967-017-1297-2
Melnik BC (2018) Overexpression of p53 explains isotretinoin’s teratogenicity. Exp Dermatol 27:91–93. https://doi.org/10.1111/exd.13420
Melnik BC, John SM, Schmitz G (2011) Over-stimulation of insulin/IGF-1 signaling by western diet may promote diseases of civilization: lessons learnt from laron syndrome. Nutr Metab 8:41. https://doi.org/10.1186/1743-7075-8-41
Melnik BC, Schmitz G (2009) Role of insulin, insulin-like growth factor-1, hyperglycaemic food and milk consumption in the pathogenesis of acne vulgaris. Exp Dermatol 18:833–841. https://doi.org/10.1111/j.1600-0625.2009.00924.x
Melnik BC, Schmitz G (2013) Are therapeutic effects of antiacne agents mediated by activation of FoxO1 and inhibition of mTORC1? Exp Dermatol 22:502–504. https://doi.org/10.1111/exd.12172
Melnik BC, Zouboulis CC (2013) Potential role of FoxO1 and mTORC1 in the pathogenesis of Western diet-induced acne. Exp Dermatol 22:311–315. https://doi.org/10.1111/exd.12142
Melo MN, Dugourd D, Castanho MA (2006) Omiganan pentahydrochloride in the front line of clinical applications of antimicrobial peptides. Recent Patents Anti-infect Drug Discov 1:201–207. https://doi.org/10.2174/157489106777452638
Monfrecola G, Lembo S, Caiazzo G, De Vita V, Di Caprio R, Balato A, Fabbrocini G (2016) Mechanistic target of rapamycin (mTOR) expression is increased in acne patients’ skin. Exp Dermatol 25:153–155. https://doi.org/10.1111/exd.12885
Nagy I, Pivarcsi A, Koreck A, Szell M, Urban E, Kemeny L (2005) Distinct strains of Propionibacterium acnes induce selective human beta-defensin-2 and interleukin-8 expression in human keratinocytes through toll-like receptors. J Investig Dermatol 124:931–938. https://doi.org/10.1111/j.0022-202X.2005.23705.x
Nakamura MT, Nara TY (2002) Gene regulation of mammalian desaturases. Biochem Soc Trans 30:1076–1079
Papakonstantinou E, Aletras AJ, Glass E, Tsogas P, Dionyssopoulos A, Adjaye J, Fimmel S, Gouvousis P, Herwig R, Lehrach H, Zouboulis CC, Karakiulakis G (2005) Matrix metalloproteinases of epithelial origin in facial sebum of patients with acne and their regulation by isotretinoin. J Investig Dermatol 125:673–684. https://doi.org/10.1111/j.0022-202X.2005.23848.x
Pappas K, Xu J, Zairis S, Resnick-Silverman L, Abate F, Steinbach N, Ozturk S, Saal LH, Su T, Cheung P, Schmidt H, Aaronson S, Hibshoosh H, Manfredi J, Rabadan R, Parsons R (2017) p53 maintains baseline expression of multiple tumor suppressor genes. MCR 15:1051–1062. https://doi.org/10.1158/1541-7786.mcr-17-0089
Qin M, Pirouz A, Kim MH, Krutzik SR, Garban HJ, Kim J (2014) Propionibacterium acnes Induces IL-1beta secretion via the NLRP3 inflammasome in human monocytes. J Investig Dermatol 134:381–388. https://doi.org/10.1038/jid.2013.309
Rabe T, Kowald A, Ortmann J, Rehberger-Schneider S (2000) Inhibition of skin 5 alpha-reductase by oral contraceptive progestins in vitro. Gynecol Endocrinol 14:223–230. https://doi.org/10.3109/09513590009167685
Rifka SM, Pita JC, Vigersky RA, Wilson YA, Loriaux DL (1978) Interaction of digitalis and spironolactone with human sex steroid receptors. J Clin Endocrinol Metab 46:338–344. https://doi.org/10.1210/jcem-46-2-338
Rocha MA, Bagatin E (2018) Skin barrier and microbiome in acne. Arch Dermatol Res 310:181–185. https://doi.org/10.1007/s00403-017-1795-3
Schmidt N, Gans EH (2011) Tretinoin: a review of its anti-inflammatory properties in the treatment of acne. J Clin Aesth Dermatol 4:22–29
Schmuth M, Ortegon AM, Mao-Qiang M, Elias PM, Feingold KR, Stahl A (2005) Differential expression of fatty acid transport proteins in epidermis and skin appendages. J Investig Dermatol 125:1174–1181. https://doi.org/10.1111/j.0022-202X.2005.23934.x
Schneider MR, Paus R (2010) Sebocytes, multifaceted epithelial cells: lipid production and holocrine secretion. Int J Biochem Cell Biol 42:181–185. https://doi.org/10.1016/j.biocel.2009.11.017
Seleit I, Bakry OA, Abdou AG, Hashim A (2014) Body mass index, selected dietary factors, and acne severity: are they related to in situ expression of insulin-like growth factor-1? Anal Quant Cytopathol Histopathol 36:267–278
Serafini PC, Catalino J, Lobo RA (1985) The effect of spironolactone on genital skin 5 alpha-reductase activity. J Steroid Biochem 23:191–194. https://doi.org/10.1016/0022-4731(85)90236-5
Shi G, Liao PY, Cai XL, Pi XX, Zhang MF, Li SJ, Quan JH, Fan YM (2018) FoxO1 enhances differentiation and apoptosis in human primary keratinocytes. Exp Dermatol 27:1254–1260. https://doi.org/10.1111/exd.13775
Skidmore R, Kovach R, Walker C, Thomas J, Bradshaw M, Leyden J, Powala C, Ashley R (2003) Effects of subantimicrobial-dose doxycycline in the treatment of moderate acne. Arch Dermatol 139:459–464. https://doi.org/10.1001/archderm.139.4.459
Smith R, Mann N, Makelainen H, Roper J, Braue A, Varigos G (2008) A pilot study to determine the short-term effects of a low glycemic load diet on hormonal markers of acne: a nonrandomized, parallel, controlled feeding trial. Mol Nutr Food Res 52:718–726. https://doi.org/10.1002/mnfr.200700307
Smith RN, Mann NJ, Braue A, Makelainen H, Varigos GA (2007) The effect of a high-protein, low glycemic-load diet versus a conventional, high glycemic-load diet on biochemical parameters associated with acne vulgaris: a randomized, investigator-masked, controlled trial. J Am Acad Dermatol 57:247–256. https://doi.org/10.1016/j.jaad.2007.01.046
Steiner B, Romero-Steiner S, Cruce D, George R (1997) Cloning and sequencing of the hyaluronate lyase gene from Propionibacterium acnes. Can J Microbiol 43:315–321. https://doi.org/10.1139/m97-044
Stewart TJ, Bazergy C (2018) Hormonal and dietary factors in acne vulgaris versus controls. Dermato-endocrinol 10:e1442160. https://doi.org/10.1080/19381980.2018.1442160
Thiboutot D, Gollnick H, Bettoli V, Dreno B, Kang S, Leyden JJ, Shalita AR, Lozada VT, Berson D, Finlay A, Goh CL, Herane MI, Kaminsky A, Kubba R, Layton A, Miyachi Y, Perez M, Martin JP, Ramos ESM, See JA, Shear N, Wolf J Jr (2009) New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol 60:S1–S50. https://doi.org/10.1016/j.jaad.2009.01.019
Thiboutot DM, Knaggs H, Gilliland K, Hagari S (1997) Activity of type 1 5 alpha-reductase is greater in the follicular infrainfundibulum compared with the epidermis. Br J Dermatol 136:166–171
Thielitz A, Sidou F, Gollnick H (2007) Control of microcomedone formation throughout a maintenance treatment with adapalene gel, 0.1%. J Eur Acad Dermatol Venereol 21:747–753. https://doi.org/10.1111/j.1468-3083.2007.02190.x
Torocsik D, Kovacs D, Camera E, Lovaszi M, Cseri K, Nagy GG, Molinaro R, Ruhl R, Tax G, Szabo K, Picardo M, Kemeny L, Zouboulis CC, Remenyik E (2014) Leptin promotes a proinflammatory lipid profile and induces inflammatory pathways in human SZ95 sebocytes. Br J Dermatol 171:1326–1335. https://doi.org/10.1111/bjd.13229
Vlassova N, Han A, Zenilman JM, James G, Lazarus GS (2011) New horizons for cutaneous microbiology: the role of biofilms in dermatological disease. Br J Dermatol 165:751–759. https://doi.org/10.1111/j.1365-2133.2011.10458.x
Wiesner J, Vilcinskas A (2010) Antimicrobial peptides: the ancient arm of the human immune system. Virulence 1:440–464. https://doi.org/10.4161/viru.1.5.12983
Williams HC, Dellavalle RP, Garner S (2012) Acne vulgaris. Lancet 379:361–372. https://doi.org/10.1016/s0140-6736(11)60321-8
Yoon JY, Kwon HH, Min SU, Thiboutot DM, Suh DH (2013) Epigallocatechin-3-gallate improves acne in humans by modulating intracellular molecular targets and inhibiting P. acnes. J Investig Dermatol 133:429–440. https://doi.org/10.1038/jid.2012.292
Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, Bowe WP, Graber EM, Harper JC, Kang S, Keri JE, Leyden JJ, Reynolds RV, Silverberg NB, Stein Gold LF, Tollefson MM, Weiss JS, Dolan NC, Sagan AA, Stern M, Boyer KM, Bhushan R (2016) Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol 74:945–973.e933. https://doi.org/10.1016/j.jaad.2015.12.037
Zhang L, Anthonavage M, Huang Q, Li WH, Eisinger M (2003) Proopiomelanocortin peptides and sebogenesis. Ann N Y Acad Sci 994:154–161. https://doi.org/10.1111/j.1749-6632.2003.tb03175.x
Zouboulis CC, Akamatsu H, Stephanek K, Orfanos CE (1994) Androgens affect the activity of human sebocytes in culture in a manner dependent on the localization of the sebaceous glands and their effect is antagonized by spironolactone. Skin Pharmacol 7:33–40
Zouboulis CC, Angres S, Seltmann H (2011) Regulation of stearoyl-coenzyme A desaturase and fatty acid delta-6 desaturase-2 expression by linoleic acid and arachidonic acid in human sebocytes leads to enhancement of proinflammatory activity but does not affect lipogenesis. Br J Dermatol 165:269–276. https://doi.org/10.1111/j.1365-2133.2011.10340.x
Zouboulis CC, Dessinioti C, Tsatsou F, Gollnick HPM (2017) Anti-acne drugs in phase 1 and 2 clinical trials. Expert Opin Investig Drugs 26:813–823. https://doi.org/10.1080/13543784.2017.1337745
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This review does not involve human participants; therefore, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cong, TX., Hao, D., Wen, X. et al. From pathogenesis of acne vulgaris to anti-acne agents. Arch Dermatol Res 311, 337–349 (2019). https://doi.org/10.1007/s00403-019-01908-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-019-01908-x