Abstract
Purpose
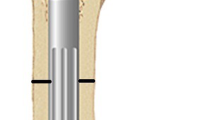
Hip reconstruction with subtrochanteric valgus extension pelvic support osteotomy and distal femoral osteotomy for lengthening and varus correction is one of the options available for salvage of chronic unstable hips and is also known as Ilizarov hip reconstruction (IHR). This study evaluated the outcomes and complications associated with IHR in skeletally mature young patients.
Methods
Twelve patients (7 males, 5 females) with a mean age of 23 years underwent IHR for chronically dislocated hips due to various causes. Preoperative clinical and radiological evaluations were used to determine the site of osteotomies and the required angulations. Postoperatively the patients were followed up clinically and radiologically for a minimum of 36 months. Ilizarov fixator was removed when adequate lengthening was achieved and there was radiological evidence of union. Harris Hip Score was used to document hip function preoperatively and at final evaluation.
Results
Significant improvements occurred in limb length discrepancy (LLD) 5.11 cm preoperatively to 0.9 cm at final evaluation, Harris Hip Score 44.33 points preoperatively to 70.83 points (p < 0.0001) at final evaluation. Trendelenberg sign disappeared completely in nine patients and was delayed in three at final evaluation. The abduction at the hip increased from the preoperative mean of 12.08° (range 0°–25°) to 22.5° (range 15°–35°) postoperatively. The fixed flexion deformity at the hip decreased from 22° (range 10°–35°) preoperatively to 3° postoperatively (range 0°–10°). The amount of free flexion at the operated hips decreased from the preoperative mean of 88.33° (range 70°–120°) to 70.42° (range 45°–105°) at final follow up. The mean fixator interval was 7.33 months (5–12 months) and the mean follow up duration was 59.4 months (38–86 months).
Conclusions
IHR is effective in improving the hip biomechanics, correcting the LLD and eliminating the Trendelenberg sign. Lengthy period of fixator wear, knee stiffness and pin tract infections, though minor are known limitations of this procedure.




Similar content being viewed by others
References
Aksoy MC, Musdal Y (2000) Subtrochanteric valgus-extension osteotomy for neglected congenital dislocation of the hip in young adults. Acta Orthop Belg 66:181–186
Bombelli R (1993) Structure and function in normal and abnormal hips. 3rd edn. Springer, Berlin
Milch H (1989) The “pelvic support” osteotomy. 1941. Clin Orthop Relat Res 249:4–11
Ilizarov GA (1991) Treatment of disorders of the hip, transosseous osteosynthesis: theoretical and clinical aspects of the regeneration and growth of tissue. Springer, Berlin (pp 668–696)
Paley D (ed) (2002) Hip joint considerations, the pelvic support osteotomy. In: Principles of deformity correction. Springer, Berlin, pp 647–694
Kocaoglu M, Eralp L, Sen C, Dinçyürek H (2002) The Ilizarov hip reconstruction osteotomy for hip dislocation: outcome after 4–7 years in 14 young patients. Acta Orthop Scand 73:432–438
Byrd JW, Jones KS (2000) Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy: J Arthrosc Relat Surg 16:578–587
Rozbruch SR, Paley D, Bhave A, Herzenberg JE (2005) Ilizarov hip reconstruction for the late sequelae of infantile hip infection. J Bone Joint Surg Am 87:1007–1018
Paley D (1990) Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 250:81–104
Inan M, Bowen RJ (2005) A pelvic support osteotomy and femoral lengthening with monolateral fixator. Clin Orthop Relat Res 440:192–198
Hass J (1943) A subtrochanteric osteotomy for pelvic support. J Bone Joint Surg Am 25:281–291
Soren A (1964) Hip salvage by pelvic support osteotomy. Arch Surg 89:656–662
Inan M, Alkan A, Harma A, Ertem K (2005) Evaluation of the gluteus medius muscle after a pelvic support osteotomy to treat congenital dislocation of the hip. J Bone Joint Surg Am 87:2246–2252
Glorion C, Pouliquen JC, Langlais J, Ceolin JL, Kassis B (1996) Femoral lengthening using the callotasis method: study of the complications in a series of 70 cases in children and adolescents. J Pediatr Orthop 16:161–167
Barker KL, Simpson AH, Lamb SE (2001) Loss of knee range of motion in leg lengthening. J Orthop Sports Phys Ther 31:238–244 (discussion 245–246)
Bowen JR, Levy EJ, Donohue M (1993) Comparison of knee motion and callus formation in femoral lengthening with the Wagner or monolateral-ring device. J Pediatr Orthop 13:467–472
Milch H (1955) The resection-angulation operation for hip-joint disabilities. J Bone Joint Surg Am 37-A:699–717
Bell BT (1953) Pelvic support osteotomy. Surg Clin North Am 1719–1730
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marimuthu, K., Joshi, N., Sharma, C.S. et al. Ilizarov hip reconstruction in skeletally mature young patients with chronic unstable hip joints. Arch Orthop Trauma Surg 131, 1631–1637 (2011). https://doi.org/10.1007/s00402-011-1376-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-011-1376-4