Abstract
Introduction
Non-steroidal anti-inflammatory drug (NSAID) is well known to significantly delay fracture healing. Results from in vitro studies implicate an impairment of osteoblast proliferation due to NSAIDs during the initial stages of healing. We studied whether diclofenac, a non-selective NSAID, also impairs appearance of osteoblasts in vivo during the early phase of healing (at 10 days).
Materials and methods
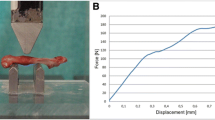
Two defects (Ø 1.1 mm) were drilled within distal femurs of 20 male Wistar rats. Ten rats received diclofenac continuously; the other obtained a placebo until sacrificing at 10 days. Osteoblast proliferation was assessed by cell counting using light microscopy, and bone mineral density (BMD) was measured using pQCT.
Results
Osteoblast counts from the centre of bone defect were significantly reduced in the diclofenac group (median 73.5 ± 8.4 cells/grid) compared to animals fed with placebo (median 171.5 ± 13.9 cells/grid). BMD within the defect showed a significant reduction after diclofenac administration (median 111.5 ± 9.3 mg/cm³) compared to the placebo group (median 177 ± 45.4 mg/cm³).
Conclusion
The reduced appearance of osteoblasts in vivo implicates an inhibiting effect of diclofenac on osteoblasts at a very early level of bone healing. The inhibition of proliferation and migration of osteoblasts, or differentiation from progenitor cells, is implicated in the delay of fracture healing after NSAID application.





Similar content being viewed by others
References
al Balla SR, el Sayed YM, al Meshal MA, Gouda MW (1994) The effects of cholestyramine and colestipol on the absorption of diclofenac in man. Int J Clin Pharmacol Ther 32:441–445
Arikawa T, Omura K, Morita I (2004) Regulation of bone morphogenetic protein-2 expression by endogenous prostaglandin E2 in human mesenchymal stem cells. J Cell Physiol 200:400–406
Beck A, Krischak G, Sorg T, Augat P, Farker K, Merkel U, Kinzl L, Claes L (2003) Influence of diclofenac (group of nonsteroidal anti-inflammatory drugs) on fracture healing. Arch Orthop Trauma Surg 123:327–332
Bhandari M, Schemitsch EH (2002) Bone formation following intramedullary femoral reaming is decreased by indomethacin and antibodies to insulin-like growth factors. J Orthop Trauma 16:717–722
Blair HC, Athanasou NA (2004) Recent advances in osteoclast biology and pathological bone resorption. Histol Histopathol 19:189–199
Bort R, Ponsoda X, Jover R, Gomez-Lechon MJ, Castell JV (1999) Diclofenac toxicity to hepatocytes: a role for drug metabolism in cell toxicity. J Pharmacol Exp Ther 288:65–72
Boushel R, Langberg H, Risum N, Kjaer M (2004) Regulation of blood flow by prostaglandins. Curr Vasc Pharmacol 2:191–197
Brown KM, Saunders MM, Kirsch T, Donahue HJ, Reid JS (2004) Effect of COX-2-specific inhibition on fracture-healing in the rat femur. J Bone Joint Surg Am 86-A:116–123
Dekel S, Lenthall G, Francis MJO (1981) Release of prostaglandins from bone and muscle after tibial fracture. An experimental study in rabbits. J Bone Joint Surg Br 63-B:185–189
Dinarello CA (2002) The IL-1 family and inflammatory diseases. Clin Exp Rheumatol 20:S1–S13
Endo K, Sairyo K, Komatsubara S, Sasa T, Egawa H, Yonekura D, Adachi K, Ogawa T, Murakami R, Yasui N (2002) Cyclooxygenase-2 inhibitor inhibits the fracture healing. J Physiol Anthropol Appl Human Sci 21:235–238
Harizi H, Norbert G (2004) Inhibition of IL-6, TNF-alpha, and cyclooxygenase-2 protein expression by prostaglandin E2-induced Il-10 in bone marrow-derived dendritic cells. Cell Immunol 228:99–109
Ho ML, Chang JK, Chuang LY, Hsu HK, Wang GJ (1999) Effects of nonsteroidal anti-inflammatory drugs and prostaglandins on osteoblastic functions. Biochem Pharmacol 58:983–990
Høgevold HE, Grøgaard B, Reikerås O (1992) Effects of short-term treatment with corticosteroids and indomethacin on bone healing. A mechanical study of osteotomies in rats. Acta Orthop Scand 63:607–611
Kaspar D, Hedrich CM, Schmidt C, Liedert A, Claes LE, Ignatius AA (2005) Diclofenac hemmt die Proliferation und Matrixbildung osteoblastärer Zellen. Unfallchirurg 108:18–24
Krischak GD, Augat P, Sorg T, Blakytny R, KInzl L, Claes L, Beck A (2007) Effects of diclofenac on periosteal callus maturation in osteotomy healing in an animal model. Arch Orthop Trauma Surg 127:3–9
Li TF, Zuscik MJ, Ionescu AM, Zhang X, Rosier RN, Schwarz EM, Drissi H, O’Keefe RJ (2004) PGE2 inhibits chondrocyte differentiation through PKA and PKC signaling. Exp Cell Res 300:159–169
Liles JH, Flecknell PA (1994) A comparison of the effects of buprenorphine, carprofen and flunixin following laparotomy in rats. J Vet Pharmacol Ther 17:284–290
Matziolis G, Rau HM, Klever P, Erli HJ, Paar O (2002) Beeinflussung humaner Osteoblasten durch verschiedene Analgetika. Unfallchirurg 105:527–531
Needleman P, Turk J, Jakschik BA, Morrison AR, Lefkowith JB (1986) Arachidonic acid metabolism. Annu Rev Biochem 55:69–102
Okamoto F, Kajiya H, Fukushima H, Jimi E, Okabe K (2004) Prostaglandin E2 activates outwardly rectifying Cl(-) channels via a cAMP-dependent pathway and reduces cell motility in rat osteoclasts. Am J Physiol Cell Physiol 287:114–124
Raisz LG, Woodiel FN (2003) Effects of selective prostaglandin EP2 and EP4 receptor agonists on bone resorption and formation on fetal rat organ cultures. Prostaglandins Other Lipid Mediat 71:287–292
Shamir D, Keila S, Weinreb M (2004) A selective EP4 receptor antagonist abrogates the stimulation of osteoblast recruitment from bone marrow stromal cells by prostaglandin E2 in vivo and in vitro. Bone 34:157–162
Vane JR, Botting RM (1998) Mechanism of action of antiinflammatory drugs. Int J Tissue React 20:3–15
Vassiliou E, Jing H, Ganea D (2003) Prostaglandin E2 inhibits TNF production in murine bone marrow-derived dendritic cells. Cell Immunol 223:120–132
Vrotsos Y, Miller SC, Marks SC Jr (2003) Prostaglandin E–a powerful anabolic agent for generalized or site-specific bone formation. Crit Rev Eukaryot Gene Expr 13:255–263
Acknowledgments
We are grateful for the excellent technical assistance of Liselotte Mueller-Molenar, Patrizia Horny, Sonja Grueninger, and Marion Tomo. We would like to thank Novartis Pharma (Nuremberg, Germany) for their support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krischak, G.D., Augat, P., Blakytny, R. et al. The non-steroidal anti-inflammatory drug diclofenac reduces appearance of osteoblasts in bone defect healing in rats. Arch Orthop Trauma Surg 127, 453–458 (2007). https://doi.org/10.1007/s00402-007-0288-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-007-0288-9