Abstract
Purpose
This study aimed to explore the differences in iodine metabolism and expression of NIS and Pendrin in pregnant rats under different iodine nutritional status.
Methods
Female Wistar rats were divided into four groups: low iodine (LI), normal iodine (NI), ten fold high iodine (10HI), and fifty fold high iodine (50HI). The intervention began after one week of adaptive feeding. Iodine metabolism experiments were performed beginning on the 15th day of pregnancy. 24-h iodine intake and excretion were calculated. The concentrations of iodine in urine, fecal, thyroid, and placenta were measured by ICP-MS. PCR and Western Blot were used to detect the mRNA levels and cell membrane protein of sodium/iodide symporter (NIS) and Pendrin in the small intestine, thyroid, kidney, and placenta.
Results
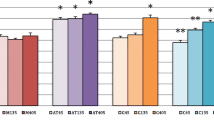
Fecal iodine excretion (FIE) and urinary iodine excretion (UIE) in the 50HI group were significantly higher than those in the NI group (P < 0.05). The NIS protein and mRNA in the kidney and small intestine have an upward trend in iodine deficiency and a downward trend in iodine excess. Thyroid and placental iodine storage in the 50HI group were significantly higher than those in the NI group (P < 0.05). NIS, Pendrin protein, and mRNA in the thyroid and placenta tend to increase when iodine is deficient and decrease when there is excess.
Conclusion
Iodine excretion and iodine stores in the placenta and thyroid gland are positively correlated with iodine intake. NIS and Pendrin are also regulated by iodine intake.






Similar content being viewed by others
Availability of data and materials
All data are available by reasonable request from the corresponding author.
References
Andersson M, Braegger CP (2022) The role of iodine for thyroid function in lactating women and infants. Endocr Rev 43(3):469–506. https://doi.org/10.1210/endrev/bnab029
Pearce EN, Lazarus JH, Moreno-Reyes R, Zimmermann MB (2016) Consequences of iodine deficiency and excess in pregnant women: an overview of current knowns and unknowns. Am J Clin Nutr 104(3):918S-923S. https://doi.org/10.3945/ajcn.115.110429
Zimmermann MB (2009) Iodine deficiency. Endocr Rev 30(4):376–408. https://doi.org/10.1210/er.2009-0011
Zimmermann MB, Boelaert K (2015) Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol 3(4):286–295. https://doi.org/10.1016/s2213-8587(14)70225-6
Abel MH, Caspersen IH, Meltzer HM, Haugen M, Brandlistuen RE, Aase H, Alexander J, Torheim LE, Brantsæter AL (2017) Suboptimal maternal iodine intake is associated with impaired child neurodevelopment at 3 years of age in the Norwegian mother and child cohort study. J Nutr 147(7):1314–1324. https://doi.org/10.3945/jn.117.250456
Abel MH, Ystrom E, Caspersen IH, Meltzer HM, Aase H, Torheim LE, Askeland RB, Reichborn-Kjennerud T, Brantsæter AL (2017) Maternal iodine intake and offspring attention-deficit/hyperactivity disorder: results from a large prospective cohort study. Nutrients. https://doi.org/10.3390/nu9111239
Thomas Jde V, Collett-Solberg PF (2009) Perinatal goiter with increased iodine uptake and hypothyroidism due to excess maternal iodine ingestion. Horm Res 72(6):344–347. https://doi.org/10.1159/000249162
Dworkin HJ, Jacquez JA, Beierwaltes WH (1966) Relationship of iodine ingestion to iodine excretion in pregnancy. J Clin Endocrinol Metab 26(12):1329–1342. https://doi.org/10.1210/jcem-26-12-1329
Chen W, Wang W, Gao M, Chen Y, Guo W, Dong S, Sun H, Pan Z, Pearce EN, Tan L, Shen J, Zhang W (2023) Iodine intakes of <150 μg/day or >550 μg/day are not recommended during pregnancy: a balance study. J Nutr 153(7):2041–2050. https://doi.org/10.1016/j.tjnut.2022.10.017
Lacroix L, Mian C, Caillou B, Talbot M, Filetti S, Schlumberger M, Bidart JM (2001) Na+/I− symporter and Pendred syndrome gene and protein expressions in human extra-thyroidal tissues. Eur J Endocrinol 144(3):297–302. https://doi.org/10.1530/eje.0.1440297
De la Vieja A, Santisteban P (2018) Role of iodide metabolism in physiology and cancer. Endocr Relat Cancer 25(4):R225-r245. https://doi.org/10.1530/erc-17-0515
Portulano C, Paroder-Belenitsky M, Carrasco N (2014) The Na+/I− symporter (NIS): mechanism and medical impact. Endocr Rev 35(1):106–149. https://doi.org/10.1210/er.2012-1036
Nicola JP, Reyna-Neyra A, Carrasco N, Masini-Repiso AM (2012) Dietary iodide controls its own absorption through post-transcriptional regulation of the intestinal Na+/I− symporter. J Physiol 590(23):6013–6026. https://doi.org/10.1113/jphysiol.2012.241307
Bizhanova A, Kopp P (2009) Minireview: the sodium-iodide symporter NIS and Pendrin in iodide homeostasis of the thyroid. Endocrinology 150(3):1084–1090. https://doi.org/10.1210/en.2008-1437
Karaoglan M, İşbilen E (2021) The role of placental iodine storage in the neonatal thyroid stimulating hormone surge: iodine as a driving force to adapt the terrestrial life. J Endocrinol Invest 44(5):1041–1052. https://doi.org/10.1007/s40618-020-01399-y
Neven KY, Marien CBD, Janssen BG, Roels HA, Waegeneers N, Nawrot TS, Ruttens A (2020) Variability of iodine concentrations in the human placenta. Sci Rep 10(1):161. https://doi.org/10.1038/s41598-019-56775-3
Neven KY, Cox B, Vrijens K, Plusquin M, Roels HA, Ruttens A, Nawrot TS (2020) Determinants of placental iodine concentrations in a mild-to-moderate iodine-deficient population: an ENVIRONAGE cohort study. J Transl Med 18(1):426. https://doi.org/10.1186/s12967-020-02601-8
Chen XY, Lin CH, Yang LH, Li WG, Zhang JW, Zheng WW, Wang X, Qian J, Huang JL, Lei YX (2016) The effect on sodium/iodide symporter and Pendrin in thyroid colloid retention developed by excess iodide intake. Biol Trace Elem Res 172(1):193–200. https://doi.org/10.1007/s12011-015-0580-4
Suzuki K, Kimura H, Wu H, Kudo N, Kim WB, Suzuki S, Yoshida A, Caturegli P, Kohn LD (2010) Excess iodide decreases transcription of NIS and VEGF genes in rat FRTL-5 thyroid cells. Biochem Biophys Res Commun 393(2):286–290. https://doi.org/10.1016/j.bbrc.2010.01.123
Sun Y, Han Y, Qian M, Li Y, Ye Y, Lin L, Liu Y (2021) Defending effects of iodide transfer in placental barrier against maternal iodine deficiency. Thyroid 31(3):509–518. https://doi.org/10.1089/thy.2020.0510
Spitzweg C, Dutton CM, Castro MR, Bergert ER, Goellner JR, Heufelder AE, Morris JC (2001) Expression of the sodium iodide symporter in human kidney. Kidney Int 59(3):1013–1023. https://doi.org/10.1046/j.1523-1755.2001.0590031013.x
Li N, Jiang Y, Shan Z, Teng W (2012) Prolonged high iodine intake is associated with inhibition of type 2 deiodinase activity in pituitary and elevation of serum thyrotropin levels. Br J Nutr 107(5):674–682. https://doi.org/10.1017/s0007114511003552
Serrano-Nascimento C, Salgueiro RB, Pantaleão T, Corrêa da Costa VM, Nunes MT (2017) Maternal exposure to iodine excess throughout pregnancy and lactation induces hypothyroidism in adult male rat offspring. Sci Rep 7(1):15591. https://doi.org/10.1038/s41598-017-15529-9
Guo W, Yang Y, Jiang W, Cheng Y, Wu W, Pan Z, Zhang D, Li S, Ren Z, Zhang N, Zhang K, Pearce EN, Chen W, Zhang W (2023) An iodine balance study in Chinese school-age children. J Clin Endocrinol Metab 108(10):e949–e955. https://doi.org/10.1210/clinem/dgad244
Kessler J, Hooge D (2007) Aqueous iodine equilibria in Mammalian iodination reactions. Thyroid 17(1):19–24. https://doi.org/10.1089/thy.2006.0243
Altorjay A, Dohán O, Szilágyi A, Paroder M, Wapnir IL, Carrasco N (2007) Expression of the Na+/I− symporter (NIS) is markedly decreased or absent in gastric cancer and intestinal metaplastic mucosa of Barrett esophagus. BMC Cancer 7:5–5. https://doi.org/10.1186/1471-2407-7-5
Rozenfeld J, Efrati E, Adler L, Tal O, Carrithers SL, Alper SL, Zelikovic I (2011) Transcriptional regulation of the Pendrin gene. Cell Physiol Biochem 28(3):385–396. https://doi.org/10.1159/000335100
Burns R, O’Herlihy C, Smyth PP (2011) The placenta as a compensatory iodine storage organ. Thyroid 21(5):541–546. https://doi.org/10.1089/thy.2010.0203
Burns R, Azizi F, Hedayati M, Mirmiran P, O’Herlihy C, Smyth PP (2011) Is placental iodine content related to dietary iodine intake? Clin Endocrinol (Oxf) 75(2):261–264. https://doi.org/10.1111/j.1365-2265.2011.04039.x
Mitchell AM, Manley SW, Morris JC, Powell KA, Bergert ER, Mortimer RH (2001) Sodium iodide symporter (NIS) gene expression in human placenta. Placenta 22(2–3):256–258. https://doi.org/10.1053/plac.2000.0609
Bidart JM, Lacroix L, Evain-Brion D, Caillou B, Lazar V, Frydman R, Bellet D, Filetti S, Schlumberger M (2000) Expression of Na+/I− symporter and Pendred syndrome genes in trophoblast cells. J Clin Endocrinol Metab 85(11):4367–4372. https://doi.org/10.1210/jcem.85.11.6969
Andersen SL, Nøhr SB, Wu CS, Olsen J, Pedersen KM, Laurberg P (2013) Thyroglobulin in smoking mothers and their newborns at delivery suggests autoregulation of placental iodide transport overcoming thiocyanate inhibition. Eur J Endocrinol 168(5):723–731. https://doi.org/10.1530/eje-12-0759
Schröder-van der Elst JP, van der Heide D, Kastelijn J, Rousset B, Obregón MJ (2001) The expression of the sodium/iodide symporter is up-regulated in the thyroid of fetuses of iodine-deficient rats. Endocrinology 142(9):3736–3741. https://doi.org/10.1210/endo.142.9.8377
Li H, Richard K, McKinnon B, Mortimer RH (2007) Effect of iodide on human choriogonadotropin, sodium-iodide symporter expression, and iodide uptake in BeWo choriocarcinoma cells. J Clin Endocrinol Metab 92(10):4046–4051. https://doi.org/10.1210/jc.2006-2358
Funding
This work study was funded by the National Natural Science Foundation of China (NSFC Grant nos. 81920108031).
Author information
Authors and Affiliations
Contributions
WZ and MF contributed to the study conception and design. MF, HZ, YG, RY, QJ, QM, YQ, and NS performed the experiments. Data analysis was performed by MF, YG, and QM. The first draft of the manuscript was written by MF and YG. RY checks the manuscript. All authors commented on previous versions of the manuscript; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
The Tianjin Hospital of ITCWM Nankai Hospital Animal Ethics Committee approved all the experimental procedures (NKYY-DWLL-2021-048).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, M., Zhang, H., Gao, Y. et al. Mechanism of multi-organ compensation under different iodine intake in pregnant rats: results from a repeated-measures study of iodine metabolism. Eur J Nutr 63, 589–598 (2024). https://doi.org/10.1007/s00394-023-03288-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03288-5