Abstract
Purpose
To examine the associations of dietary patterns and nutrients with coronary artery calcification (CAC) and pericardial adiposity (PAT) in adults with and without type 1 diabetes.
Methods
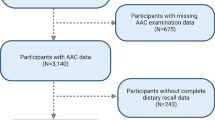
We conducted a six-year longitudinal analysis of data from Coronary Artery Calcification in Type 1 Diabetes study [n = 1255; T1D: n = 563; non-DM: n = 692] collected at baseline, year 3 and year 6. Participants completed a validated food frequency questionnaire, a physical examination, and fasting (12 h overnight fast) biochemical analyses. CAC and PAT were measured using electron beam computed tomography. Dietary patterns were identified using factor analysis. Generalized estimating equations were used to examine associations of dietary patterns and nutrients with CAC and PAT in models adjusted for traditional cardiovascular risks.
Results
The ‘starchy veggies, meats and alcohol pattern’ was associated with significantly increased risk of CAC presence in all adjusted models; an increasing trend was observed with CAC progression. Increasing intake of dietary proteins and total fats were also associated with higher risk of the presence and/or progression of CAC in adjusted models (all p < 0.05). PAT was positively associated with dietary total fats, and inversely associated with dietary intakes of saturated fats, omega-3 fats and fiber in models adjusted for age, sex, total calories, time, diabetes status, systolic blood pressure, serum lipids and physical activity.
Conclusion
Diets high in total fats and proteins, and in meats (processed and red) and alcohol may increase risks of CAC, while saturated fats, omega-3-fats and fiber may be protective against pericardial adiposity as a risk factor for coronary artery disease.
ClinicalTrials.gov Identifier: NCT00005754.
Similar content being viewed by others
References
Rawshani A, Sattar N, Franzén S, Rawshani A, Hattersley AT, Svensson AM, Eliasson B, Gudbjörnsdottir S (2018) Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: a nationwide, register-based cohort study. Lancet 392(10146):477–486. https://doi.org/10.1016/s0140-6736(18)31506-x
de Ferranti SD, de Boer IH, Fonseca V, Fox CS, Golden SH, Lavie CJ, Magge SN, Marx N, McGuire DK, Orchard TJ, Zinman B, Eckel RH (2014) Type 1 diabetes mellitus and cardiovascular disease: a scientific statement from the American Heart Association and American Diabetes Association. Circulation 130(13):1110–1130. https://doi.org/10.1161/cir.0000000000000034
Budoff M, Backlund JC, Bluemke DA, Polak J, Bebu I, Schade D, Strowig S, Raskin P, Lachin JM (2019) The association of coronary artery calcification with subsequent incidence of cardiovascular disease in type 1 diabetes: the DCCT/EDIC trials. JACC Cardiovasc Imaging 12(7 Pt 2):1341–1349. https://doi.org/10.1016/j.jcmg.2019.01.014
Olson JC, Edmundowicz D, Becker DJ, Kuller LH, Orchard TJ (2000) Coronary calcium in adults with type 1 diabetes: a stronger correlate of clinical coronary artery disease in men than in women. Diabetes 49(9):1571–1578. https://doi.org/10.2337/diabetes.49.9.1571
Wheeler GL, Shi R, Beck SR, Langefeld CD, Lenchik L, Wagenknecht LE, Freedman BI, Rich SS, Bowden DW, Chen MY, Carr JJ (2005) Pericardial and visceral adipose tissues measured volumetrically with computed tomography are highly associated in type 2 diabetic families. Invest Radiol 40(2):97–101
Alman AC, Jacobs DR Jr, Lewis CE, Snell-Bergeon JK, Carnethon MR, Terry JG, Goff DC Jr, Ding J, Carr JJ (2016) Higher pericardial adiposity is associated with prevalent diabetes: the coronary artery risk development in young adults study. Nutr Metab Cardiovasc Dis 26(4):326–332. https://doi.org/10.1016/j.numecd.2015.12.011
Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, O’Donnell CJ, Fox CS (2008) Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation 117(5):605–613. https://doi.org/10.1161/circulationaha.107.743062
Shah RV, Anderson A, Ding J, Budoff M, Rider O, Petersen SE, Jensen MK, Koch M, Allison M, Kawel-Boehm N, Wisocky J, Jerosch-Herold M, Mukamal K, Lima JAC, Murthy VL (2017) Pericardial, but not hepatic, fat by CT is associated with CV outcomes and structure: the multi-ethnic study of atherosclerosis. JACC Cardiovasc Imaging 10(9):1016–1027. https://doi.org/10.1016/j.jcmg.2016.10.024
McClain J, Hsu F, Brown E, Burke G, Carr J, Harris T, Kritchevsky S, Szklo M, Tracy R, Ding J (2013) Pericardial adipose tissue and coronary artery calcification in the Multi-ethnic Study of Atherosclerosis (MESA). Obesity (Silver Spring) 21(5):1056–1063. https://doi.org/10.1002/oby.20090
Alman AC, Smith SR, Eckel RH, Hokanson JE, Burkhardt BR, Sudini PR, Wu Y, Schauer IE, Pereira RI, Snell-Bergeon JK (2017) The ratio of pericardial to subcutaneous adipose tissues is associated with insulin resistance. Obesity (Silver Spring) 25(7):1284–1291. https://doi.org/10.1002/oby.21875
Zhong VW, Lamichhane AP, Crandell JL, Couch SC, Liese AD, The NS, Tzeel BA, Dabelea D, Lawrence JM, Marcovina SM, Kim G, Mayer-Davis EJ (2016) Association of adherence to a Mediterranean diet with glycemic control and cardiovascular risk factors in youth with type I diabetes: the SEARCH Nutrition Ancillary Study. Eur J Clin Nutr 70(7):802–807. https://doi.org/10.1038/ejcn.2016.8
Nansel TR, Lipsky LM, Liu A (2016) Greater diet quality is associated with more optimal glycemic control in a longitudinal study of youth with type 1 diabetes. Am J Clin Nutr 104(1):81–87. https://doi.org/10.3945/ajcn.115.126136
Ahola AJ, Freese R, Mäkimattila S, Forsblom C, Groop PH (2016) Dietary patterns are associated with various vascular health markers and complications in type 1 diabetes. J Diabetes Complications 30(6):1144–1150. https://doi.org/10.1016/j.jdiacomp.2016.03.028
Jaacks LM, Crandell J, Mendez MA, Lamichhane AP, Liu W, Ji L, Du S, Rosamond W, Popkin BM, Mayer-Davis EJ (2015) Dietary patterns associated with HbA1c and LDL cholesterol among individuals with type 1 diabetes in China. J Diabetes Complications 29(3):343–349. https://doi.org/10.1016/j.jdiacomp.2014.12.014
Jacobs DR Jr, Steffen LM (2003) Nutrients, foods, and dietary patterns as exposures in research: a framework for food synergy. Am J Clin Nutr 78(3 Suppl):508s–513s. https://doi.org/10.1093/ajcn/78.3.508S
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13(1):3–9
Frölich S, Lehmann N, Weyers S, Wahl S, Dragano N, Budde T, Kälsch H, Mahabadi AA, Erbel R, Moebus S, Jöckel KH, Schmidt B (2017) Association of dietary patterns with five-year degree and progression of coronary artery calcification in the Heinz Nixdorf Recall study. Nutr Metab Cardiovasc Dis 27(11):999–1007. https://doi.org/10.1016/j.numecd.2017.09.002
Nettleton JA, Schulze MB, Jiang R, Jenny NS, Burke GL, Jacobs DR Jr (2008) A priori-defined dietary patterns and markers of cardiovascular disease risk in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 88(1):185–194. https://doi.org/10.1093/ajcn/88.1.185
Miedema MD, Petrone A, Shikany JM, Greenland P, Lewis CE, Pletcher MJ, Gaziano JM, Djousse L (2015) Association of fruit and vegetable consumption during early adulthood with the prevalence of coronary artery calcium after 20 years of follow-up: the coronary artery risk development in young adults (CARDIA) study. Circulation 132(21):1990–1998. https://doi.org/10.1161/circulationaha.114.012562
Heine-Bröring RC, Brouwer IA, Proença RV, van Rooij FJ, Hofman A, Oudkerk M, Witteman JC, Geleijnse JM (2010) Intake of fish and marine n-3 fatty acids in relation to coronary calcification: the Rotterdam Study. Am J Clin Nutr 91(5):1317–1323. https://doi.org/10.3945/ajcn.2009.28416
Sekikawa A, Mahajan H, Kadowaki S, Hisamatsu T, Miyagawa N, Fujiyoshi A, Kadota A, Maegawa H, Murata K, Miura K, Edmundowicz D, Ueshima H (2019) Association of blood levels of marine omega-3 fatty acids with coronary calcification and calcium density in Japanese men. Eur J Clin Nutr 73(5):783–792. https://doi.org/10.1038/s41430-018-0242-7
van Woudenbergh GJ, Vliegenthart R, van Rooij FJ, Hofman A, Oudkerk M, Witteman JC, Geleijnse JM (2008) Coffee consumption and coronary calcification: the Rotterdam Coronary Calcification Study. Arterioscler Thromb Vasc Biol 28(5):1018–1023. https://doi.org/10.1161/atvbaha.107.160457
Miller PE, Zhao D, Frazier-Wood AC, Michos ED, Averill M, Sandfort V, Burke GL, Polak JF, Lima JAC, Post WS, Blumenthal RS, Guallar E, Martin SS (2017) Associations of coffee, tea, and caffeine intake with coronary artery calcification and cardiovascular events. Am J Med 130(2):188-197.e185. https://doi.org/10.1016/j.amjmed.2016.08.038
Shah RV, Murthy VL, Allison MA, Ding J, Budoff M, Frazier-Wood AC, Lima JA, Steffen L, Siscovick D, Tucker KL, Ouyang P, Abbasi SA, Danielson K, Jerosch-Herold M, Mozaffarian D (2016) Diet and adipose tissue distributions: the multi-ethnic study of atherosclerosis. Nutr Metab Cardiovasc Dis 26(3):185–193. https://doi.org/10.1016/j.numecd.2015.12.012
Snell-Bergeon JK, Chartier-Logan C, Maahs DM, Ogden LG, Hokanson JE, Kinney GL, Eckel RH, Ehrlich J, Rewers M (2009) Adults with type 1 diabetes eat a high-fat atherogenic diet that is associated with coronary artery calcium. Diabetologia 52(5):801–809. https://doi.org/10.1007/s00125-009-1280-4
Basu A, Alman AC, Snell-Bergeon JK (2019) Dietary fiber intake and glycemic control: coronary artery calcification in type 1 diabetes (CACTI) study. Nutr J 18(1):23. https://doi.org/10.1186/s12937-019-0449-z
Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC (1992) Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol 135(10):1114–1126; discussion 1127–1136. https://doi.org/10.1093/oxfordjournals.aje.a116211
Willett WC, Sampson L, Browne ML, Stampfer MJ, Rosner B, Hennekens CH, Speizer FE (1988) The use of a self-administered questionnaire to assess diet four years in the past. Am J Epidemiol 127(1):188–199. https://doi.org/10.1093/oxfordjournals.aje.a114780
Dabelea D, Kinney G, Snell-Bergeon JK, Hokanson JE, Eckel RH, Ehrlich J, Garg S, Hamman RF, Rewers M (2003) Effect of type 1 diabetes on the gender difference in coronary artery calcification: a role for insulin resistance? The coronary artery calcification in type 1 diabetes (CACTI) study. Diabetes 52(11):2833–2839. https://doi.org/10.2337/diabetes.52.11.2833
Snell-Bergeon JK, Hokanson JE, Jensen L, MacKenzie T, Kinney G, Dabelea D, Eckel RH, Ehrlich J, Garg S, Rewers M (2003) Progression of coronary artery calcification in type 1 diabetes: the importance of glycemic control. Diabetes Care 26(10):2923–2928. https://doi.org/10.2337/diacare.26.10.2923
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15(4):827–832. https://doi.org/10.1016/0735-1097(90)90282-t
Keselman HJ, Cribbie R, Holland B (2002) Controlling the rate of type I error over a large set of statistical tests. Br J Math Stat Psychol 55(Pt 1):27–39. https://doi.org/10.1348/000711002159680
Nettleton JA, Steffen LM, Schulze MB, Jenny NS, Barr RG, Bertoni AG, Jacobs DR Jr (2007) Associations between markers of subclinical atherosclerosis and dietary patterns derived by principal components analysis and reduced rank regression in the multi-ethnic study of atherosclerosis (MESA). Am J Clin Nutr 85(6):1615–1625. https://doi.org/10.1093/ajcn/85.6.1615
Wang D, Karvonen-Gutierrez CA, Jackson EA, Elliott MR, Appelhans BM, Barinas-Mitchell E, Bielak LF, Huang MH, Baylin A (2020) Western dietary pattern derived by multiple statistical methods is prospectively associated with subclinical carotid atherosclerosis in midlife women. J Nutr 150(3):579–591. https://doi.org/10.1093/jn/nxz270
Costa CS, Del-Ponte B, Assunção MCF, Santos IS (2018) Consumption of ultra-processed foods and body fat during childhood and adolescence: a systematic review. Public Health Nutr 21(1):148–159. https://doi.org/10.1017/s1368980017001331
Micha R, Wallace SK, Mozaffarian D (2010) Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation 121(21):2271–2283. https://doi.org/10.1161/circulationaha.109.924977
Song F, Schmidt AM (2012) Glycation and insulin resistance: novel mechanisms and unique targets? Arterioscler Thromb Vasc Biol 32(8):1760–1765. https://doi.org/10.1161/atvbaha.111.241877
Huang J, Liao LM, Weinstein SJ, Sinha R, Graubard BI, Albanes D (2020) Association between plant and animal protein intake and overall and cause-specific mortality. JAMA Intern Med 180(9):1–12. https://doi.org/10.1001/jamainternmed.2020.2790
McClelland RL, Bild DE, Burke GL, Mukamal KJ, Lima JA, Kronmal RA (2008) Alcohol and coronary artery calcium prevalence, incidence, and progression: results from the multi-ethnic study of atherosclerosis (MESA). Am J Clin Nutr 88(6):1593–1601. https://doi.org/10.3945/ajcn.2008.26420
Pletcher MJ, Varosy P, Kiefe CI, Lewis CE, Sidney S, Hulley SB (2005) Alcohol consumption, binge drinking, and early coronary calcification: findings from the coronary artery risk development in young adults (CARDIA) study. Am J Epidemiol 161(5):423–433. https://doi.org/10.1093/aje/kwi062
Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J (2017) Relationship of alcohol consumption to all-cause, cardiovascular, and cancer-related mortality in U.S. adults. J Am Coll Cardiol 70(8):913–922. https://doi.org/10.1016/j.jacc.2017.06.054
Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S, Bolton T, Paige E, Paul DS, Sweeting M, Burgess S, Bell S, Astle W, Stevens D, Koulman A, Selmer RM, Verschuren WMM, Sato S, Njølstad I, Woodward M, Salomaa V, Nordestgaard BG, Yeap BB, Fletcher A, Melander O, Kuller LH, Balkau B, Marmot M, Koenig W, Casiglia E, Cooper C, Arndt V, Franco OH, Wennberg P, Gallacher J, de la Cámara AG, Völzke H, Dahm CC, Dale CE, Bergmann MM, Crespo CJ, van der Schouw YT, Kaaks R, Simons LA, Lagiou P, Schoufour JD, Boer JMA, Key TJ, Rodriguez B, Moreno-Iribas C, Davidson KW, Taylor JO, Sacerdote C, Wallace RB, Quiros JR, Tumino R, Blazer DG 2nd, Linneberg A, Daimon M, Panico S, Howard B, Skeie G, Strandberg T, Weiderpass E, Nietert PJ, Psaty BM, Kromhout D, Salamanca-Fernandez E, Kiechl S, Krumholz HM, Grioni S, Palli D, Huerta JM, Price J, Sundström J, Arriola L, Arima H, Travis RC, Panagiotakos DB, Karakatsani A, Trichopoulou A, Kühn T, Grobbee DE, Barrett-Connor E, van Schoor N, Boeing H, Overvad K, Kauhanen J, Wareham N, Langenberg C, Forouhi N, Wennberg M, Després JP, Cushman M, Cooper JA, Rodriguez CJ, Sakurai M, Shaw JE, Knuiman M, Voortman T, Meisinger C, Tjønneland A, Brenner H, Palmieri L, Dallongeville J, Brunner EJ, Assmann G, Trevisan M, Gillum RF, Ford I, Sattar N, Lazo M, Thompson SG, Ferrari P, Leon DA, Smith GD, Peto R, Jackson R, Banks E, Di Angelantonio E, Danesh J (2018) Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 391(10129):1513–1523. https://doi.org/10.1016/s0140-6736(18)30134-x
Mukamal KJ, Conigrave KM, Mittleman MA, Camargo CA Jr, Stampfer MJ, Willett WC, Rimm EB (2003) Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N Engl J Med 348(2):109–118. https://doi.org/10.1056/NEJMoa022095
Zhao J, Stockwell T, Roemer A, Naimi T, Chikritzhs T (2017) Alcohol consumption and mortality from coronary heart disease: an updated meta-analysis of cohort studies. J Stud Alcohol Drugs 78(3):375–386. https://doi.org/10.15288/jsad.2017.78.375
Kauhanen J, Kaplan GA, Goldberg DE, Salonen R, Salonen JT (1999) Pattern of alcohol drinking and progression of atherosclerosis. Arterioscler Thromb Vasc Biol 19(12):3001–3006. https://doi.org/10.1161/01.atv.19.12.3001
Aune D (2019) Plant foods, antioxidant biomarkers, and the risk of cardiovascular disease, cancer, and mortality: a review of the evidence. Adv Nutr 10(Suppl 4):S404–S421. https://doi.org/10.1093/advances/nmz042
Wang PY, Fang JC, Gao ZH, Zhang C, Xie SY (2016) Higher intake of fruits, vegetables or their fiber reduces the risk of type 2 diabetes: a meta-analysis. J Diabetes Investig 7(1):56–69. https://doi.org/10.1111/jdi.12376
Zurbau A, Au-Yeung F, Blanco Mejia S, Khan TA, Vuksan V, Jovanovski E, Leiter LA, Kendall CWC, Jenkins DJA, Sievenpiper JL (2020) Relation of different fruit and vegetable sources with incident cardiovascular outcomes: a systematic review and meta-analysis of prospective cohort studies. J Am Heart Assoc 9(19):e017728. https://doi.org/10.1161/jaha.120.017728
Bertoia ML, Mukamal KJ, Cahill LE, Hou T, Ludwig DS, Mozaffarian D, Willett WC, Hu FB, Rimm EB (2015) Changes in intake of fruits and vegetables and weight change in United States men and women followed for up to 24 years: analysis from three prospective cohort studies. PLoS Med 12(9):e1001878. https://doi.org/10.1371/journal.pmed.1001878
Hennein R, Liu C, McKeown NM, Hoffmann U, Long MT, Levy D, Ma J (2019) Increased diet quality is associated with long-term reduction of abdominal and pericardial fat. Obesity (Silver Spring) 27(4):670–677. https://doi.org/10.1002/oby.22427
Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, Willett WC, Rimm EB, Hu FB (2015) Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation 132(23):2212–2219. https://doi.org/10.1161/circulationaha.115.017158
Yi SY, Steffen LM, Terry JG, Jacobs DR, Duprez D, Steffen BT, Zhou X, Shikany JM, Harnack L, Carr JJ (2020) Added sugar intake is associated with pericardial adipose tissue volume. Eur J Prev Cardiol 27(18):2016–2023. https://doi.org/10.1177/2047487320931303
Albracht-Schulte K, Kalupahana NS, Ramalingam L, Wang S, Rahman SM, Robert-McComb J, Moustaid-Moussa N (2018) Omega-3 fatty acids in obesity and metabolic syndrome: a mechanistic update. J Nutr Biochem 58:1–16. https://doi.org/10.1016/j.jnutbio.2018.02.012
Rafraf M, Mohammadi E, Asghari-Jafarabadi M, Farzadi L (2012) Omega-3 fatty acids improve glucose metabolism without effects on obesity values and serum visfatin levels in women with polycystic ovary syndrome. J Am Coll Nutr 31(5):361–368. https://doi.org/10.1080/07315724.2012.10720443
Spencer M, Finlin BS, Unal R, Zhu B, Morris AJ, Shipp LR, Lee J, Walton RG, Adu A, Erfani R, Campbell M, McGehee RE Jr, Peterson CA, Kern PA (2013) Omega-3 fatty acids reduce adipose tissue macrophages in human subjects with insulin resistance. Diabetes 62(5):1709–1717. https://doi.org/10.2337/db12-1042
Li Y, Hruby A, Bernstein AM, Ley SH, Wang DD, Chiuve SE, Sampson L, Rexrode KM, Rimm EB, Willett WC, Hu FB (2015) Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: a prospective cohort study. J Am Coll Cardiol 66(14):1538–1548. https://doi.org/10.1016/j.jacc.2015.07.055
Hu FB, Willett WC (2002) Optimal diets for prevention of coronary heart disease. JAMA 288(20):2569–2578. https://doi.org/10.1001/jama.288.20.2569
Astrup A, Magkos F, Bier DM, Brenna JT, de Oliveira Otto MC, Hill JO, King JC, Mente A, Ordovas JM, Volek JS, Yusuf S, Krauss RM (2020) Saturated fats and health: a reassessment and proposal for food-based recommendations: JACC state-of-the-art review. J Am Coll Cardiol 76(7):844–857. https://doi.org/10.1016/j.jacc.2020.05.077
Hjelmgaard K, Eschen RB, Schmidt EB, Andreasen JJ, Lundbye-Christensen S (2018) Fatty acid composition in various types of cardiac adipose tissues and its relation to the fatty acid content of atrial tissue. Nutrients 10(10):1506. https://doi.org/10.3390/nu10101506
Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, Sampson L, Willett WC (1999) Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr 69(2):243–249. https://doi.org/10.1093/ajcn/69.2.243
McGrath AJ, Hamill LL, Cardwell CR, Draffin CR, Neville CE, Appleton KM, McEneny J, McKinley MC, Young IS, Woodside JV (2016) Combining vitamin C and carotenoid biomarkers better predicts fruit and vegetable intake than individual biomarkers in dietary intervention studies. Eur J Nutr 55(4):1377–1388. https://doi.org/10.1007/s00394-015-0953-7
McLean RM, Farmer VL, Nettleton A, Cameron CM, Cook NR, Campbell NRC (2017) Assessment of dietary sodium intake using a food frequency questionnaire and 24-hour urinary sodium excretion: a systematic literature review. J Clin Hypertens (Greenwich) 19(12):1214–1230. https://doi.org/10.1111/jch.13148
Bédard A, Garcia-Aymerich J, Sanchez M, Le Moual N, Clavel-Chapelon F, Boutron-Ruault MC, Maccario J, Varraso R (2015) Confirmatory factor analysis compared with principal component analysis to derive dietary patterns: a longitudinal study in adult women. J Nutr 145(7):1559–1568. https://doi.org/10.3945/jn.114.204479
Schoenaker DA, Dobson AJ, Soedamah-Muthu SS, Mishra GD (2013) Factor analysis is more appropriate to identify overall dietary patterns associated with diabetes when compared with Treelet transform analysis. J Nutr 143(3):392–398. https://doi.org/10.3945/jn.112.169011
Shikany JM, Safford MM, Newby PK, Durant RW, Brown TM, Judd SE (2015) Southern dietary pattern is associated with hazard of acute coronary heart disease in the reasons for geographic and racial differences in stroke (REGARDS) study. Circulation 132(9):804–814. https://doi.org/10.1161/circulationaha.114.014421
Shu L, Shen XM, Li C, Zhang XY, Zheng PF (2017) Dietary patterns are associated with type 2 diabetes mellitus among middle-aged adults in Zhejiang Province. China Nutr J 16(1):81. https://doi.org/10.1186/s12937-017-0303-0
Acknowledgements
We would like to thank all participants for their contributions to this study.
Funding
Support for this study was provided by the National Institutes of Health National Heart, Lung and Blood Institute grants R01 HL61753, R01 HL079611 and R01 HL113029, American Diabetes Association grant 7-06-CVD-28, American Diabetes Association Grant 7-13-CD-10 (Snell-Bergeon), American Diabetes Association Grant 7-13-CE-02 (Alman), and Diabetes Endocrinology Research Center Clinical Investigation Core P30 DK57516. The study was performed at the Adult General Clinical Research Center at the University of Colorado Denver Anschutz Medical Center supported by the NIH M01 RR000051 and NIH/NCATS Colorado CTSA Grant Number UL1TR002535, the Barbara Davis Center for Childhood Diabetes in Denver and at Colorado Heart Imaging Center in Denver, CO, USA. In addition, support for statistical analyses for the current report was provided by the Dean’s Faculty Development award (Basu) at the School of Integrated Health Sciences at UNLV.
Author information
Authors and Affiliations
Contributions
AB, ACA and JKS-B contributed to the conception and design of the study, analysis, and interpretation of the data and drafted the manuscript. LCC performed data analyses. All authors critically revised, read, and approved the final manuscript and agreed to be fully accountable for ensuring the integrity and accuracy of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethics approval and consent to participate
All study participants provided informed consent and the study protocol was approved by the Colorado Multiple Institutional Review Board. This observational study was performed in consistent with the approved guidelines.
Rights and permissions
About this article
Cite this article
Basu, A., Chien, LC., Alman, A.C. et al. Associations of dietary patterns and nutrients with coronary artery calcification and pericardial adiposity in a longitudinal study of adults with and without type 1 diabetes. Eur J Nutr 60, 3911–3925 (2021). https://doi.org/10.1007/s00394-021-02564-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02564-6