Abstract
Purpose
This study examined the association of free sugar (FS) intake with obesity measures and blood pressure (BP) among a nationally representative sample of Australian adults.
Methods
Data from adults (weighted n = 5136) who completed 2 × 24-h recalls and had complete data for BP, waist circumference (WC), waist-to-height ratio (WHtR), and body mass index (BMI) were analyzed. Associations between percentage energy of FS from all food sources (%EFStotal), beverages only (%EFSbeverages), and non-beverages sources only (%EFSnon-beverages) and obesity measures and BP were examined using linear and non-linear regressions. Logistic regression was used to calculate the odds ratios (OR) of being classified as overweight and/or obese, having increased cardiometabolic risks, and elevated BP per 5% point increase in %EFStotal, %EFSbeverages, and %EFSnon-beverages. All regression analyses were adjusted for known socio-economic and lifestyle confounders.
Results
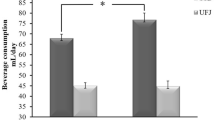
%EFSbeverage was positively associated with BMI, WC, and WHtR (all p < 0.05), while %EFSnon-beverage was inversely associated with these outcomes. Increases in odds of having an undesirable WC/WHtR were found with increasing %EFSbeverages (OR per 5% point increase in %EFSbeverages: 1.19 for WC; 1.23 for WHtR, both p < 0.001). %EFStotal and %EFSnon-beverages were weakly and negatively associated with diastolic BP. A 5% point increase in %EFStotal and %EFSnon-beverage was associated with a 10–25% reduction in odds of having elevated BP.
Conclusions
Our results suggested that only a higher FS intake from beverages may be associated with obesity, and higher FS intake was associated with reduced odds of having elevated BP.
Similar content being viewed by others
Introduction
The potential health effects of sugar, particularly added sugar, have been a regular topic of discussion in public health, especially in light of the worldwide obesity epidemic. The World Health Organization (WHO) has recently updated its recommendation that the intake of ‘free sugar’, defined as added sugar plus sugars naturally occurring in honey, syrups, and fruit juices, be limited [1]. However, this recommendation is mainly based on the association between free sugar and dental caries, as evidence for associations between free sugar and non-communicable diseases, obesity, and poor diet quality is lacking [1].
Major sources of free sugar in a typical western diet include energy-dense foods such as sweetened desserts and beverages [2], with sugar-sweetened beverages (SSB) accounting for the largest contribution in the Australian diet [3, 4]. Therefore, it is not surprising that the associations between SSB and weight gain, and diet quality, have been extensively explored. A recent meta-analysis concluded that high SSB consumption encourages weight gain in both children and adults [5]. Similar results were seen in another meta-analysis, suggesting that intake of free sugar or SSB was associated with weight gain of 0.75 kg in individuals on an ad libitum diet [6]. The available evidence also suggests that free sugar intake may influence blood pressure independently of its effects on body weight [7], with a meta-analysis showing associations between high SSB consumption and increased incidence of hypertension [8].
It has also been suggested that free sugars from different sources (non-beverages vs. beverages) may have different effects on health outcomes. Studies suggest that reductions in liquid sources of free sugar may promote greater weight reduction compared to that of reducing the solid sources of sugar [9, 10]. A high intake of liquid sources of free sugar has been associated with greater energy intake compared to solid sources [10], where the lower satiating effect of liquids may be a contributory factor towards these observations.
Numerous studies have been conducted to examine the health effects of high free sugar intake, particularly from SSB; however, evidence regarding free sugar intake and its association with health outcomes in a nationally representative sample is lacking. Therefore, this study aimed to examine the associations between free sugar intake and blood pressure and obesity measures among a nationally representative sample of Australian adults. A secondary aim was to examine differences in the associations between free sugar intake and blood pressure and obesity measures based on the source of sugar (i.e., beverages vs. non-beverage).
Method
Data source
This secondary analysis was undertaken using data from the National Nutrition and Physical Activity Survey (NNPAS) which was conducted as part of the Australian Health Survey 2011–2012 by the Australian Bureau of Statistics (ABS) [11]. Detailed methodology of the NNPAS can be found elsewhere [12]. The NNPAS data were collected in accordance to the Australian Census and Statistics Act 1905 [13].
Dietary intake assessment
A computer-assisted face-to-face 24-h recall based on the US Department of Agriculture (USDA) Automated Multiple Pass Method (AMPM) [14, 15] was used to assess the dietary intake of the 9341 adult respondents of the NNPAS. A second telephone-based AMPM 24-h recall was collected from 65% of these respondents at least 8 days after the first interview (n = 6053). The AUSNUT2011–2013 food composition database [16] was used to translate the 24-h recall data into nutrient intake, and food items were classified into beverages and non-beverages. A modified version of a published ten-step methodology was used to estimate the free sugar content of all food items [17, 18]. In this study, ‘free sugar’ is defined as all sugars (including honey and syrup) added to foods during manufacturing and processing, plus sugar in fruit juices, as per the WHO definition [1].
Anthropometric and blood pressure measurements
The methodologies used for these measurements have been reported in detail by the ABS [12]. In brief, research staff measured the height, weight, and waist circumference (WC) of participants according to a standard protocol. The AHS protocol stipulates that measurements for subjects with weight exceed 150 kg to not be recorded and were treated as missing in this analysis, and that WC measurements above 200 cm to be recorded as 200 cm [19]. For blood pressure, two measurements were taken with the second reading usually being used; however, a third reading was taken if the difference between readings exceeded 10 mmHg. Body mass index (BMI) scores were calculated by dividing weight (kg) by height (m) squared, and were classified according to the WHO recommendations [20,21,22]. Waist:height ratio (WHtR) was calculated as waist (cm) divided by height (m), with a measurement ≥ 0.5 classifying subjects as having increased likelihood of cardiometabolic risk factors [23]. Subjects were classified as having an ‘increased cardiometabolic risk’ if their WC was ≥ 94 cm for men and ≥ 80 cm for women; and ‘substantially increased cardiometabolic risks’ if their WC was ≥ 102 cm for men and ≥ 88 cm for women [24]. Blood pressure measures were categorized as normal or elevated (> 140/90 mmHg), as survey respondents could not be formally diagnosed with hypertension due to blood pressure measurements being taken at only one time point [25].
Assessment of non-dietary variables
Various population characteristics were collected as part of the NNPAS including demographics, income, geographical classifications, and lifestyle factors. Of these, binary variables were created for country of birth (main English speaking vs. other), smoking status (ever smoked vs. never smoked), whether on diet for health reasons or to lose weight (yes vs. no), and remoteness of home (major cities vs. other). Remoteness of home was based on the Accessibility/Remoteness Index of Australia (ARIA) with major cities being those with an index value of 0–0.2 [12, 26]. In addition, quintiles of socio-economic indexes for areas (SEIFA) and deciles of equivalised household income were tested as potential confounders. SEIFA assigns a level of socio-economic advantage or disadvantage to subjects based on their characteristics of their residential area such as education, employment levels, and dwelling size [12]. In comparison, equivalised income is a standardized estimate of household income which aims to reflect the households’ relative well-being [12]. Level of physical activity (expressed as a continuous variable—total time spent doing physical activity per week) was determined through a series of questions regarding physical activity and exercise (excluding vigorous gardening) undertaken in the week prior to the interview [12].
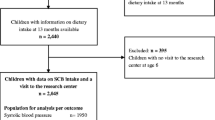
Statistical analysis
This secondary analysis was registered at http://anzctr.org.au (reference number: ACTRN12618001154291). In this study, only adult respondents with data from 2 × 24 h recalls and no missing data for covariates were included (weighted n = 5136). A flow of participant diagram is available as Supplemental Fig. 1. Data were weighted to account for under- and over-sampling allowing representation of the Australian population with regards to age group, gender, and region. The weighting factors supplied by the ABS were readjusted to account for the exclusions made in the analyses. Usual free sugar intake was estimated using the Multiple Source Method [27]. Subject characteristics were examined by sex (Table 1). To explore the relation between the anthropometric and blood pressure measurements, and %EFStotal, %EFSbeverages, and %EFSnonbeverage, linear and non-linear (quadratic and cubic, Online Supplemental Table 1) regressions were used, with β ± SE presented as per 5% point increase in the %EFS variables. Logistic regression was used to calculate the odds (95% CI) of being classified as overweight and/or obese, having increased cardiometabolic risks, and elevated blood pressure per 5% point increase in %EFStotal, %EFSbeverages, and %EFSnon-beverages. All regression analyses were performed using: (1) the crude model (no adjustments); (2) adjustments for age and sex only; and (3) further adjustments for SEIFA (quintiles), equivalised household income (deciles), remoteness of home (urban vs. rural), whether born in English speaking countries (yes/no), on diet (yes/no), smoker status (yes/no), and physical activity (min/week, continuous). Statistical Packages for Social Science version 24.0 (IBM Corporation, New York, NY, USA, 2010) was used for all statistical analyses, where the Complex Sample function was used to correctly handle the sample weighting for the logistic regression analysis. A p < 0.05 was considered statistically significant.
Sensitivity analyses
We performed additional sensitivity analyses which exclude energy mis-reporters to examine the effect of mis-reporting on our results, as previously described [28]. The Goldberg cut-off [29] for 2-day dietary data and a physical activity level (PAL) of 1.55 [i.e., plausible if energy intake:basal metabolic rate (EI:BMR) is within 0.96–2.49] were used to identify mis-reporters [4]. This range was used per the advice of the ABS [15], and is similar to that used in the previous studies [30,31,32]. We excluded 1025 extreme mis-reporters based on this method. Results of the sensitivity analyses are presented in Online Supplemental Tables 2, 3, and 4.
Results
Table 2 displays the β ± SE and R2 of the linear regression models. Although some β ± SE values were statistically significant, the crude model all had very small R2 values, which were improved by further adjustments in the age- and sex-adjusted and multivariate adjusted models. The multivariate adjusted models explained between 4.0 and 26.8% of the variance in the outcomes examined (as continuous variables), where the variance in waist circumference is the most explained by the model. Variance in diastolic blood pressure is largely unexplained, while 24.2% of the variance in systolic pressure could be explained by the multivariate model. The non-linear (quadratic and cubic) models tested did not significantly improve the R2 (see Online Supplemental Table 1), and thus, results from the linear model are presented below.
A 5% point increase in %EFStotal is significantly associated with a small decrease in diastolic blood pressure (− 0.322 ± 0.148 mmHg; p = 0.029). No linear relationship was observed between %EFS from beverage or non-beverage sources and systolic blood pressure, while a 5% point increase in %EFSnon-beverages was associated with a decrease in diastolic blood pressure (− 0.531 ± 0.253 mmHg; p = 0.036). Both %EFSbeverages and %EFSnon-beverages were linearly associated with BMI, WC, and WHtR, but, in opposite directions, increases in %EFSnon-beverages were significantly associated with decreases in these outcomes (changes in BMI, WC, and WHtR per 5%point increase in %EFSnon-beverage: – 0.311 ± 0.121 kg/m2; − 0.823 ± 0.297 cm; and − 0.006 ± 0.002, respectively; all p < 0.01), while increases in %EFSbeverages were associated with increases (changes in BMI, WC and WHtR per 5%point increase in %EFSnon-beverage: 0.212 ± 0.092 kg/m2; 0.742 ± 0.225 cm and 0.006 ± 0.002, respectively; all p < 0.05). While there were slight changes in the β ± SE and p values, interpretations of the sensitivity analyses results were not materially different from the main analysis (Online Supplemental Table 3).
Table 3 shows the odds of being classified as overweight and/or obese, and having increased or substantially increased risk for CVD as categorized by WC cut-offs, and undesirable WHtR and BP per 5% point increase in %EFStotal, %EFSbeverages, and %EFSnon-beverages. Similar to the linear regression, the crude model fit poorly with low R2 values, while further adjustments improved the fit. In the multivariate model, increases in %EFStotal and %EFSnon-beverages were not associated with higher odds of having the aforementioned undesirable health measures. On the other hand, increased odds of having an undesirable WC and WHtR were observed per 5% point increase in %EFSbeverages (OR 1.19 for undesirable WC and 1.23 for undesirable WHtR, p < 0.001), while a 25% decrease in odds of having elevated BP was observed per 5% point increase in %EFSnon-beverages (p = 0.001). Although there were slight changes in the ORs, the overall results were similar when under- and over- reporters were excluded (see Online Supplemental Table 4).
Discussion
The present study is the first to examine free sugar intake from both solid foods and beverages and its association with obesity and blood pressure measures for Australian adults. Interestingly, positive associations with obesity measures were identified only for free sugar from beverage sources alone. No adverse relationship was identified for free sugar intake and blood pressure measures.
Few studies examined the effects of solid sources of free sugar on obesity as most previous studies predominantly focus on added sugar intake from beverages (e.g., SSB). The present study found that the source of free sugar is important in determining the effects on obesity measures. Total free sugar intake or free sugar from solid foods alone had no adverse impact on obesity measures, whereas increasing beverage sources of free sugar resulted in higher WC and WHtR.
A previous Australian study conducted by Cobiac et al. similarly found no association between total added sugar intake and BMI among Australians [2]. However, this may be due to energy intake being included as a covariate, as it is well known that excess energy intake plays a key role in the obesity development. Contrary to popular belief, a secondary analysis of the 2007 Australian National Children’s Nutrition and Physical Activity Survey suggested that free sugar may not be uniquely obesogenic apart from its contribution to total energy intake [33].
The previous systemic reviews and meta-analyses of prospective cohort studies and randomized control trials unanimously found that SSB promoted weight gain in adults [5, 6]. This is in accordance with the present findings which indicate that only liquid sources of free sugars (i.e., obtained from beverages) are associated with increased BMI and WC. A common suggestion for the potential mechanism of liquid sources having a greater effect on weight and obesity measures is that liquid sources produce a lower sense of satiety compared to solid sources [34]. Liquid energy has been suggested to be more obesogenic than solid energy in a modelling study in Australian children [35]. Another study demonstrated that liquid sugars (from SSBs) are associated with increased energy intake, whereas solid sugars from jellybeans with similar macronutrient content provoked dietary compensation [10]. This is possibly due to the mastication required for solid foods which induces internal satiety signals, in addition to the early pancreatic exocrine and endocrine responses being lower for liquids [36, 37].
The present study found higher intakes of %EFS, in particular that from non-beverage sources, were associated with a lower odds of having elevated BP. This concurs with the findings of a previous systematic review and meta-analysis of randomized-controlled trials which suggested that total dietary free sugar influenced BP independent of the effect on body weight [7]. On the other hand, another review found that increased SSBs’ consumption is associated with elevated BP [38]. The disparity in the results may be due to the differences in the sweeteners examined; sucrose is the main sweetener used in Australia [39], whereas high-fructose corn syrup was the dominant sweetener in the studies examined in the previous reviews. In addition, it was proposed that the association between high SSBs consumption and increased BP may be in part due to increased salt intake [40], where increased salt intake has been widely associated with increased total fluid consumption, and if SSBs contribute to this fluid consumption, then salt intake may be a causal factor of increased BP rather than SSBs per se [40]. However, we were unable to examine such relationship as data quality of sodium intake in the NNPAS is considered suboptimal [41]. Nonetheless, it should be kept in mind that the single measurement of BP in this study does not allow the accurate classification of BP status.
This study provides further evidence to support the reduction of free sugar intake from beverages as a possible strategy towards addressing the worldwide obesity epidemic. In fact, many countries are now considering to, or have already imposed a ‘sugar tax’ to limit the intake of SSBs [42,43,44,45]. Furthermore, although nutrient-rich fruit and vegetable juices were counted as beverage sources of free sugar, they are normally not the main source of free sugar consumed [46]. While evidence for a recommended threshold of free sugar intake is currently limited, the benefits of reducing free sugar intake for weight have been substantiated by many studies [9, 47, 48].
This study has several strengths. First, a nationally representative sample was used in the analysis, allowing generalizability to the Australian population. Second, anthropometric and blood pressure parameters were measured (not self-reported) using the standard protocols, thus, increasing accuracy. Furthermore, an adapted version of a published method was used to estimate free sugar levels of foods, and we utilized a statistical approach [27] to transform the dietary data to better represent usual intake, both of which would improve the validity of the study findings. While it is acknowledged that the statistically modelled usual intake may not have captured the full extent of within-person variation, this approach is considered to be better than using the average from two 24-h recalls and have become common practice in nutritional epidemiological research [49].
Limitations of this study include its cross-sectional nature, which does not allow the assessment of causal relationship. However, we were able to show that, among a nationally representative sample of Australian adults, the association between high free sugar intake and adverse obesity and blood pressure parameters appear to be largely attributable to free sugars from liquid sources only. Self-report of dietary intake using 24 h recalls has inherent limitations such as those associated with memory and difficulty quantifying portion sizes [50]. We also caution the readers about the possibility of mis-reporting free sugars intake due to selective under-reporting of foods, e.g., social desirability bias where an obese individual is more likely to report a lower free sugar intake to impress the interviewer. This usually attenuates the association between free sugar intake and overweight and obesity. Unlike the other nutrients where objective measures such as recovery biomarker are available to validate the self-reported data, for free sugars, there are currently no established biomarkers or other objective measures, as naturally occurring and added sugars are chemically identical and thus non-distinguishable [18]. In recent years, researchers have investigated urinary sucrose/fructose [51], as well as carbon stable isotope ratio [52] as biomarkers for dietary total/added sugars intake; however, the specificity to added/free sugar is poor. Population-specific biomarker calibration equations have been utilized in some studies [53,54,55] to estimate true total sugar intake, but no such calibration studies have been conducted on the NNPAS. Moreover, as our aim was to estimate free sugars, not total sugars, other more direct methods to estimate free sugar intake are warranted. Nonetheless, results from the sensitivity analyses showed no material difference in the direction of associations observed, which indicated that mis-reporting may not have a large impact on the validity of the conclusions drawn.
Conclusions
This nationally representative study of the Australian adult population provides evidence that only a higher free sugar intake from beverages may be associated with overweight/obesity and increased cardiometabolic risk; and free sugar intake was not associated with elevated blood pressure. Our findings support the current direction of public health strategies to lower free sugars intake from beverages.
References
World Health Organization (2015) Guideline: sugars intake for adults and children. World Health Organization, Geneva
Cobiac L, Record S, Leppard P, Syrette J, Flight I (2003) Sugars in the Australian diet: results from the 1995 National Nutrition Survey. Nutr Diet 60(3):152–173
Louie JCY, Moshtaghian H, Rangan AM, Flood VM, Gill TP (2016) Intake and sources of added sugars among Australian children and adolescents. Eur J Nutr 55(8):2347–2355. https://doi.org/10.1007/s00394-015-1041-8
Lei L, Rangan AM, Flood VM, Louie JCY (2016) Dietary intake and food sources of added sugar in the Australian population. Br J Nutr 115(5):868–877
Luger M, Lafontan M, Bes-Rastrollo M et al (2018) Sugar-sweetened beverages and weight gain in children and adults: a systematic review from 2013 to 2015 and a comparison with previous studies. Obes Facts 10(6):674–693. https://doi.org/10.1159/000484566
Te Morenga L, Mallard S, Mann J (2013) Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 346:e7492. https://doi.org/10.1136/bmj.e7492
Te Morenga LA, Howatson AJ, Jones RM, Mann J (2014) Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. Am J Clin Nutr 100(1):65–79. https://doi.org/10.3945/ajcn.113.081521
Jayalath VH, de Souza RJ, Ha V et al (2015) Sugar-sweetened beverage consumption and incident hypertension: a systematic review and meta-analysis of prospective cohorts. Am J Clin Nutr 102(4):914–921. https://doi.org/10.3945/ajcn.115.107243
Chen L, Appel LJ, Loria C et al (2009) Reduction in consumption of sugar-sweetened beverages is associated with weight loss: the PREMIER trial. Am J Clin Nutr 89(5):1299–1306
DiMeglio DP, Mattes RD (2000) Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes 24(6):794–800
Australian Bureau of Statistics (2014) Australian Health Survey, 2011–13. ABS, Canberra
Australian Bureau of Statistics (2014) Australian health survey: users’ guide, 2011–13. Australian Bureau of Statistics, Canberra
Commonwealth Government of Australia (2016) Census and statistics act 1905. Federal Register of Legislation, Canberra
Bliss R (2004) Researchers produce innovation in dietary recall. Agric Res 52(6):10–12
Australian Bureau of Statistics (2013) Australian Health Survey: Users’ Guide, 2011–2013. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/74D87E30B3539C53CA257BBB0014BB36?opendocument. Accessed 2 Jun 2015
Food Standards Australia New Zealand (2014) AUTNUT 2011–13 food composition database
Louie JCY, Lei L, Rangan AM (2016) Reliability of a systematic methodology to estimate added sugars content of foods when applied to a recent Australian food composition database. J Food Comp Anal 46:36–42. https://doi.org/10.1016/j.jfca.2015.11.002
Louie JC, Moshtaghian H, Boylan S et al (2015) A systematic methodology to estimate added sugar content of foods. Eur J Clin Nutr 69(2):154–161. https://doi.org/10.1038/ejcn.2014.256
Australian Buread of Statistics (2013) 4363.0.55.001 - Australian Health Survey: Users’ Guide, 2011–2013—BODY MASS AND PHYSICAL MEASUREMENTS. Australia Bureau of Statistics. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/9C2B28A7F682FD6FCA257B8D00229E9B?opendocument. Accessed 19 Jul 2018
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320(7244):1240
Cole TJ, Flegal KM, Nicholls D, Jackson AA (2007) Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ 335(7612):194
World Health Organisation (2006) BMI classification. WHO, Geneva
Ashwell M, Gunn P, Gibson S (2012) Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev 13(3):275–286
World Health Organization (2000) Obesity: preventing and managing the global epidemic, vol 894. World Health Organization, Geneva
Stergiou G, Palatini P, Asmar R et al (2018) Blood pressure measurement and hypertension diagnosis in the 2017 US guidelines: first things first. Hypertension 71(6):963–965. https://doi.org/10.1161/hypertensionaha.118.10853
Australian Government Department of Health (2015) ASGC remoteness areas. Australian Government Department of Health, Australia
Harttig U, Haubrock J, Knuppel S, Boeing H (2011) The MSM program: web-based statistics package for estimating usual dietary intake using the multiple source method. Eur J Clin Nutr 65(Suppl 1):S87–S91. https://doi.org/10.1038/ejcn.2011.92
Mok A, Ahmad R, Rangan A, Louie JCY (2018) Intake of free sugars and micronutrient dilution in Australian adults. Am J Clin Nutr 107(1):94–104. https://doi.org/10.1093/ajcn/nqx008
Goldberg G, Black A, Jebb S et al (1991) Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr 45(12):569–581
Louie JCY, Buyken AE, Heyer K, Flood VM (2011) Dietary glycaemic index and glycaemic load among Australian children and adolescents. Br J Nutr 106(08):1273–1282. https://doi.org/10.1017/S0007114511001577
Tornaritis MJ, Philippou E, Hadjigeorgiou C et al (2014) A study of the dietary intake of Cypriot children and adolescents aged 6–18 years and the association of mother’s educational status and children’s weight status on adherence to nutritional recommendations. BMC Public Health 14:13. https://doi.org/10.1186/1471-2458-14-13
Ferrari P, Slimani N, Ciampi A et al (2002) Evaluation of under- and overreporting of energy intake in the 24-hour diet recalls in the European Prospective Investigation into Cancer and Nutrition (EPIC). Public Health Nutr 5(6B):1329–1345. https://doi.org/10.1079/PHN2002409
Wong THT, Louie JCY (2018) The direct and indirect associations of usual free sugar intake on BMI z-scores of Australian children and adolescents. Eur J Clin Nutr 72(7):1058–1060. https://doi.org/10.1038/s41430-018-0124-z
Pan A, Hu FB (2011) Effects of carbohydrates on satiety: differences between liquid and solid food. Curr Opin Clin Nutr Metab Care 14(4):385–390
Zheng M, Allman-Farinelli M, Heitmann BL et al (2015) Liquid versus solid energy intake in relation to body composition among Australian children. J Hum Nutr Diet 28(s2):70–79. https://doi.org/10.1111/jhn.12223 doi
Haber G, Heaton K, Murphy D, Burroughs L (1977) Depletion and disruption of dietary fibre: effects on satiety, plasma-glucose, and serum-insulin. Lancet 310(8040):679–682
Teff KL, Devine J, Engelman K (1995) Sweet taste: effect on cephalic phase insulin release in men. Physiol Behav 57(6):1089–1095
Malik AH, Akram Y, Shetty S, Malik SS, Njike VY (2014) Impact of sugar-sweetened beverages on blood pressure. Am J Cardiol 113(9):1574–1580
Probst YC, Dengate A, Jacobs J, Louie JC, Dunford EK (2017) The major types of added sugars and non-nutritive sweeteners in a sample of Australian packaged foods. Public Health Nutr 20(18):3228–3233. https://doi.org/10.1017/S136898001700218X
He FJ, MacGregor GA (2014) Salt intake, sugar-sweetened soft drink consumption, and blood pressure. Am J Cardiol 114(3):499
Santos JA, Webster J, Land M-A et al (2017) Dietary salt intake in the Australian population. Public Health Nutr 20(11):1887–1894. https://doi.org/10.1017/S1368980017000799
Burki TK (2016) Sugar tax in the UK. Lancet Oncol 17(5):e182. https://doi.org/10.1016/S1470-2045(16)30021-3
Vecino-Ortiz AI, Arroyo-Ariza D (2018) A tax on sugar sweetened beverages in Colombia: estimating the impact on overweight and obesity prevalence across socio economic levels. Soc Sci Med 209:111–116. https://doi.org/10.1016/j.socscimed.2018.05.043
Nakamura R, Mirelman AJ, Cuadrado C et al (2018) Evaluating the 2014 sugar-sweetened beverage tax in Chile: an observational study in urban areas. PLoS Med 15(7):e1002596. https://doi.org/10.1371/journal.pmed.1002596
Long MW, Gortmaker SL, Ward ZJ et al (2015) Cost effectiveness of a sugar-sweetened beverage excise tax in the US. Am J Prev Med 49(1):112–123. https://doi.org/10.1016/j.amepre.2015.03.004
Australian Bureau of Statistics (2015) Consumption of sweetened beverages. Australian Bureau of Statistics, Canberra
Malik VS, Pan A, Willett WC, Hu FB (2013) Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr 98(4):1084–1102
de Ruyter JC, Olthof MR, Seidell JC, Katan MB (2012) A trial of sugar-free or sugar-sweetened beverages and body weight in children. New Eng J Med 367(15):1397–1406
National Cancer Institute (2015) Dietary assessment primer. Summary tables: recommendations on potential approaches to dietary assessment for different research objectives requiring group-level estimates. http://dietassessmentprimer.cancer.gov/approach/table.html. Accessed 21 May 2015
Subar AF, Freedman LS, Tooze JA et al (2015) Addressing current criticism regarding the value of self-report dietary data. J Nutr 145(12):2639–2645. https://doi.org/10.3945/jn.115.219634
Tasevska N (2015) Urinary sugars—a biomarker of total sugars intake. Nutrients 7(7):5255
Liu SV, Moore LB, Halliday TM et al (2018) Short-term changes in added sugar consumption by adolescents reflected in the carbon isotope ratio of fingerstick blood. Nutr Health 24(4):251–259. https://doi.org/10.1177/0260106018799522
Beasley JM, Jung M, Tasevska N et al (2016) Biomarker-predicted sugars intake compared with self-reported measures in US Hispanics/Latinos: results from the HCHS/SOL SOLNAS study. Public Health Nutr 19(18):3256–3264. https://doi.org/10.1017/S1368980016001580
Campbell R, Tasevska N, Jackson KG et al (2017) Association between urinary biomarkers of total sugars intake and measures of obesity in a cross-sectional study. PLoS One 12(7):e0179508. https://doi.org/10.1371/journal.pone.0179508
Tasevska N, Pettinger M, Kipnis V et al (2018) Associations of biomarker-calibrated intake of total sugars with the risk of Type 2 diabetes and cardiovascular disease in the Women’s Health Initiative Observational study. Am J Epidemiol 187(10):2126–2135. https://doi.org/10.1093/aje/kwy115
Acknowledgements
We would like to acknowledge that the original data of 2011-12 National Nutrition and Physical Activity Survey were collected by the Australian Bureau of Statistics. The authors declare that those who carried out the original analysis and collection of data bear no responsibility for further analysis and interpretation.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows—JCYL and AR: jointly designed, supervised, and guided the study. RA: coded foods in the AUSNUT2012-13 database as beverages and non-beverages. RA, JCYL, and AM: involved in calculating usual intake of nutrients. RA and JCYL: analyzed the data. RA: wrote the first draft of the manuscript. AM, RA, JCYL, and AR: interpretation of data, contributed to the discussion, and critically reviewed the final manuscript. JCYL had primary responsibility for the final content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest. No specific funding was received from any agency in the public, commercial, or not-for-profit sectors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ahmad, R., Mok, A., Rangan, A.M. et al. Association of free sugar intake with blood pressure and obesity measures in Australian adults. Eur J Nutr 59, 651–659 (2020). https://doi.org/10.1007/s00394-019-01932-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-019-01932-7