Abstract
Background/objectives
The present controlled sialographical study was conducted to learn more from the horizontal and vertical symmetry of the ductal lesions of the major salivary glands in primary (pSS) and secondary (sSS) forms of the disease.
Materials and methods
A total of 98 patients (38 pSS patients, 38 sSS patients, 22 control subjects) were included in the study. Contrast radiography of both parotid and submandibular glands was performed within the same session. A 6-point scoring system allowed summary indexes for each of the glands to be calculated.
Results
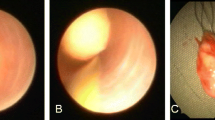
Pansialography was accomplished within 30 min each. The sparsity of the branching pattern of the ducts was the most frequent pathological finding. In pSS, horizontal symmetry was more pronounced in the parotid glands, whereas in sSS it was more pronounced in the submandibular glands. The most discriminating features were the width of the peripheral ducts in the parotid and the number of acinar dilatations in the submandibular glands. The most advanced lesions were found in the left parotid gland.
Conclusion
The peripheral ducts are more affected by SS than the main excretory duct. There is a tendency for asymmetric involvement of the parotid glands in pSS and of the submandibular glands in sSS. Parotid glands are globally more involved than submandibular glands. Differential diagnosis between pSS and sSS cannot be accomplished by means of pansialography alone. Left parotid sialography is recommended for routine use.
Zusammenfassung
Ziel der Arbeit
Die kontrollierte sialographische Studie soll dazu beitragen, die Kenntnis der horizontalen und vertikalen Symmetrie der duktalen Läsionen der großen Speicheldrüsen bei der primären (pSS) und sekundären (sSS) Form des Sjögren-Syndroms (SS) zu vertiefen.
Material und Methoden
Insgesamt 98 Patienten (38 pSS- und 38 sSS-Patienten sowie 22 Patienten in der Kontrollgruppe) wurden in die Studie aufgenommen. Die Kontrastdarstellung der Ausführungsgänge beider Ohr- und Unterkieferspeicheldrüsen wurde jeweils in der gleichen Sitzung durchgeführt. Mithilfe eines 6-Punkte-Bewertungssystems wurden für jede Drüse Summenindizes ermittelt und diese anschließend miteinander verglichen.
Ergebnisse
Alle Pansialographien wurden innerhalb von maximal 30 min durchgeführt. Häufigster pathologischer Befund war die Rarefizierung des Verzweigungsmusters der Drüsenausführungsgänge. Horizontal symmetrische Läsionen fanden sich beim pSS vorwiegend in den Ohrspeicheldrüsen, beim sSS vorwiegend in den Unterkieferspeicheldrüsen. Die zur Differenzierung am besten geeigneten Merkmale waren die Weite der peripheren Gänge in den Ohrspeicheldrüsen und die Zahl der azinären Dilatationen in den Unterkieferspeicheldrüsen. Die am meisten fortgeschrittenen Läsionen wurden in der linken Ohrspeicheldrüse nachgewiesen.
Diskussion
Die peripheren Gänge sind beim SS in allen Drüsen stärker betroffen als der Hauptausführungsgang. Beim pSS wird symmetrischer Befall vorwiegend in den Ohrspeicheldrüsen, beim sSS vorwiegend in den Unterkieferspeicheldrüsen nachgewiesen. Grundsätzlich sind die Ohrspeicheldrüsen stärker betroffen als die Unterkieferspeicheldrüsen. Die Differenzialdiagnose zwischen pSS und sSS ist mithlfe der Pansialographie nicht möglich. Für die klinische Routine wird die Sialographie der linken Ohrspeicheldrüse empfohlen.
Similar content being viewed by others
References
Vitali C, Bombardieri S, Moutsopoulos HM et al (1993) Preliminary criteria for the classification of Sjögren’s syndrome. Results of a prospective concerted action supported by the European Community. Arthritis Rheum 36:340–347
Daniels TE, Benn DK (1996) Is sialography effective in diagnosing the salivary component of Sjögren’s syndrome? Adv Dent Res 10:25–28
Chisholm DM, Waterhouse JP, Mason DK (1970) Lymphocytic sialadenitis in the major and minor glands: a correlation in postmortem subjects. J Clin Pathol 23:690–694
Waterhouse JP (1963) Focal adenitis in salivary and lacrimal glands. Proc R Soc Med 56:911–918
Obinata K, Sato T, Ohmori K et al (2010) A comparison of diagnostic tools for Sjögren syndrome, with emphasis on sialography, histopathology, and ultrasonography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:129–134
Aung W, Yamada I, Umehara I et al (2000) Sjögren’s syndrome: comparison of assessments with quantitative salivary gland scintigraphy and contrast sialography. J Nucl Med 41:257–262
Cornec D, Jousse-Jolin S, Pers JO et al (2013) Contribution of salivary gland ultrasonography to the diagnosis of Sjögren’s syndrome: toward new diagnostic criteria? Arthritis Rheum 65:216–225
Takagi Y, Kimura Y, Nakamura H et al (2010) Salivary gland ultrasonography: can it be an alternative to sialography as an imaging modality for Sjogren’s syndrome? Ann Rheum Dis 69:1321–1324
Ohbayashi N, Yamada I, Yoshino I et al (1998) Sjögren syndrome: comparison of assessments with MR sialography and conventional sialography. Radiology 209:683–688
Vitali C, Moutsopoulos HM, Bombardieri S (1994) The European Community Study Group on diagnostic criteria for Sjögren’s syndrome. Sensitivity and specificity of tests for ocular and oral involvement in Sjögren’s syndrome. Ann Rheum Dis 53:637–647
Shiboski SC, Shiboski CH, Criswell LA et al (2012) American College of Rheumatology classification criteria for Sjögren’s syndrome: a data-driven, expert consensus approach in the Sjögren’s International Collaborative Clinical Alliance Cohort. Arthritis Care Res 64:475–487
Markusse HM, Putten WIJ van, Breedveld FC et al (1993) Digital subtraction sialography of the parotid glands in primary Sjögren’s syndrome. J Rheumatol 20:279–283
Kalk WW, Vissink A, Spijkervet FK et al (2002) Parotid sialography for diagnosing Sjögren’s syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94:131–137
Andretta M, Ianniello A, Ostuni PA et al (1995) Diagnostic value of labial salivary biopsy in Sjögren’s syndrome: report of 182 cases. Acta Otorhinolaryngol Ital 15:40–46
Bloch KJ, Buchanan WW, Bunim JJ (1995) Sjögren’s syndrome: a clinical, pathological and serological study of sixty-two cases. Medicine 44:187–231
De Clerck LS, Corthouts R, Francx L et al (1988) Ultrasonography and computer tomography of the salivary glands in the evaluation of Sjögren’s syndrome. Comparison with parotid sialography. J Rheumatol 15:1777–1781
Lindvall AM, Jonsson R (1986) The salivary gland component of Sjögren’s syndrome: an evaluation of diagnostic methods. Oral Surg Oral Med Oral Pathol 62:32–42
Vitali C, Monti P, Giuggioli C et al (1989) Parotid sialography and lip biopsy in the evaluation of oral component in Sjögren’s syndrome. Clin Exp Rheumatol 7:131–135
Salaffi F, Argalia G, Carotti M et al (2000) Salivary gland ultrasonography in the evaluation of primary Sjögren’s syndrome. Comparison with minor salivary gland biopsy. J Rheumatol 27:1229–1236
Niemela RK, Paakko E, Suramo I et al (2001) Magnetic resonance imaging and magnetic resonance sialography of parotid glands in primary Sjögren’s syndrome. Arthritis Rheum 45:512–518
Alarcon-Segovia D, Ibanez G, Hernandez-Ortiz J et al (1974) Salivary gland involvement in diseases associated with Sjögren’s syndrome. 1. Radionuclide & Roentgenographic Studies. J Rheumatol 1:159–165
Tanaka O (1989) A diagnostic and etiologic study of Sjögren’s syndrome—I. Sialographical and histopathological findings of the major and minor salivary glands. Nippon Jibiinkoka Gakkai Kaiho 92:362–373
Acknowledgments
The authors thank Michael Borchert, Kornelia Kliem, and Hans-Jürgen Wolf, Berlin, and all involved patients for their invaluable contributions to the study.
Compliance with ethical guidelines
Conflict of interest. W. Golder and M. Stiller state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Golder, W., Stiller, M. Distribution pattern of Sjögren’s syndrome. Z. Rheumatol. 73, 928–933 (2014). https://doi.org/10.1007/s00393-014-1372-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-014-1372-5