Abstract
Purpose
There is a growing literature on the significance of tumor-associated macrophages (TAMs) in colorectal cancer (CRC). However, the role of TAMs in predicting the prognosis of CRC remains controversial. The current study aims to determine the prognostic and clinicopathological value of different types and distribution of TAMs in CRC.
Methods
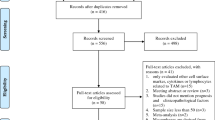
A comprehensive literature search of PubMed, Embase, and Cochrane Library databases was conducted from the inception to 1 September 2019. The correlations of TAMs with overall survival (OS), disease-free survival (DFS), cancer-specific survival (CSS), and clinicopathological characteristics were analyzed.
Results
A total of 5,575 patients from 29 studies were included in this meta-analysis. The pooled hazard ratios (HRs) indicated that high density of pan-macrophages in tumor invasive margin (IM) was associated with better OS (HR = 0.57, 95%CI = 0.38–0.85), DFS (HR = 0.32, 95%CI = 0.19–0.52), and CSS (HR = 0.56, 95%CI = 0.41–0.77). Moreover, the high density of pan-macrophages in tumor center (TC) was correlated with better DFS (HR = 0.66, 95%CI = 0.45–0.96). However, high expression of M2 macrophages in TC was associated with poor DFS (HR = 2.42, 95%CI = 1.45–4.07) and CSS (HR = 1.74, 95%CI = 1.24–2.44). High M2 macrophages density in IM was also associated with short DFS (HR = 2.81, 95%CI = 1.65–4.77). In addition, the results showed that high density of pan-macrophages in IM was associated with no tumor metastasis, while high M2 macrophages density in TC was correlated with poor tumor differentiation.
Conclusion
High Pan-TAMs density in IM has a positive effect on the prognosis of CRC patients, while high density M2 macrophage infiltration in TC is a strong indicator of poor prognosis.






Similar content being viewed by others
Availability of data and material
Not applicable.
References
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69(1):7–34. https://doi.org/10.3322/caac.21551
Hari DM, Leung AM, Lee J-H, Sim M-S, Vuong B, Chiu CG, Bilchik AJ (2013) AJCC Cancer Staging Manual 7th edition criteria for colon cancer: do the complex modifications improve prognostic assessment? J Am Coll Surg 217(2):181–190. https://doi.org/10.1016/j.jamcollsurg.2013.04.018
Feng Q, Chang W, Mao Y, He G, Zheng P, Tang W, Wei Y, Ren L, Zhu D, Ji M, Tu Y, Qin X, Xu J (2019) Tumor-associated macrophages as prognostic and predictive biomarkers for postoperative adjuvant chemotherapy in patients with stage II colon cancer. Clin Cancer Res 25(13):3896–3907. https://doi.org/10.1158/1078-0432.CCR-18-2076
Malesci A, Bianchi P, Celesti G, Basso G, Marchesi F, Grizzi F, Di Caro G, Cavalleri T, Rimassa L, Palmqvist R, Lugli A, Koelzer VH, Roncalli M, Mantovani A, Ogino S, Laghi L (2017) Tumor-associated macrophages and response to 5-fluorouracil adjuvant therapy in stage III colorectal cancer. Oncoimmunology 6(12):e1342918. https://doi.org/10.1080/2162402x.2017.1342918
Bingle L, Brown NJ, Lewis CE (2002) The role of tumour-associated macrophages in tumour progression: implications for new anticancer therapies. J Pathol 196(3):254–265. https://doi.org/10.1002/path.1027
Quail DF, Joyce JA (2013) Microenvironmental regulation of tumor progression and metastasis. Nat Med 19(11):1423–1437. https://doi.org/10.1038/nm.3394
Yang L, Zhang Y (2017) Tumor-associated macrophages: from basic research to clinical application. J Hematol Oncol 10(1):58. https://doi.org/10.1186/s13045-017-0430-2
Biswas SK, Mantovani A (2010) Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol 11(10):889–896. https://doi.org/10.1038/ni.1937
Komohara Y, Fujiwara Y, Ohnishi K, Takeya M (2016) Tumor-associated macrophages: potential therapeutic targets for anti-cancer therapy. Adv Drug Deliv Rev 99(Pt B):180–185. https://doi.org/10.1016/j.addr.2015.11.009
Takeya M, Komohara Y (2016) Role of tumor-associated macrophages in human malignancies: friend or foe? Pathol Int 66(9):491–505. https://doi.org/10.1111/pin.12440
Edin S, Wikberg ML, Dahlin AM, Rutegård J, Öberg Å, Oldenborg PA, Palmqvist R (2012) The distribution of macrophages with a M1 or M2 phenotype in relation to prognosis and the molecular characteristics of colorectal cancer. PLoS One 10:e47045. https://doi.org/10.1371/journal.pone.0047045
Kim Y, Wen X, Bae JM, Kim JH, Cho NY, Kang GH (2018) The distribution of intratumoral macrophages correlates with molecular phenotypes and impacts prognosis in colorectal carcinoma. Histopathology 73(4):663–671. https://doi.org/10.1111/his.13674
Koelzer VH, Canonica K, Dawson H, Sokol L, Karamitopoulou-Diamantis E, Lugli A, Zlobec I (2016) Phenotyping of tumor-associated macrophages in colorectal cancer: impact on single cell invasion (tumor budding) and clinicopathological outcome. OncoImmunology 5(4):e1106677. https://doi.org/10.1080/2162402X.2015.1106677
Strasser K, Birnleitner H, Beer A, Pils D, Gerner MC, Schmetterer KG, Bachleitner-Hofmann T, Stift A, Bergmann M, Oehler R (2019) Immunological differences between colorectal cancer and normal mucosa uncover a prognostically relevant immune cell profile. OncoImmunology 8(2):e1537693. https://doi.org/10.1080/2162402X.2018.1537693
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8:16. https://doi.org/10.1186/1745-6215-8-16
Väyrynen JP, Kantola T, Väyrynen SA, Klintrup K, Bloigu R, Karhu T, Mäkelä J, Herzig KH, Karttunen TJ, Tuomisto A, Mäkinen MJ (2016) The relationships between serum cytokine levels and tumor infiltrating immune cells and their clinical significance in colorectal cancer. Int J Cancer 139(1):112–121. https://doi.org/10.1002/ijc.30040
Jakubowska K, Kisielewski W, Kańczuga-Koda L, Koda M, Famulski W (2017) Stromal and intraepithelial tumor-infiltrating lymphocytes in colorectal carcinoma. Oncol Lett 14(6):6421–6432. https://doi.org/10.3892/ol.2017.7013
Oberg A, Samii S, Stenling R, Lindmark G (2002) Different occurrence of CD8+, CD45R0+, and CD68+ immune cells in regional lymph node metastases from colorectal cancer as potential prognostic predictors. Int J Color Dis 17(1):25–29. https://doi.org/10.1007/s003840100337
Ohnishi K, Komohara Y, Saito Y, Miyamoto Y, Watanabe M, Baba H, Takeya M (2013) CD169-positive macrophages in regional lymph nodes are associated with a favorable prognosis in patients with colorectal carcinoma. Cancer Sci 104(9):1237–1244. https://doi.org/10.1111/cas.12212
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Ålgars A, Irjala H, Vaittinen S, Huhtinen H, Sundström J, Salmi M, Ristamäki R, Jalkanen S (2012) Type and location of tumor-infiltrating macrophages and lymphatic vessels predict survival of colorectal cancer patients. Int J Cancer 131(4):864–873. https://doi.org/10.1002/ijc.26457
Bacman D, Merkel S, Croner R, Papadopoulos T, Brueckl W, Dimmler A (2007) TGF-beta receptor 2 downregulation in tumour-associated stroma worsens prognosis and high-grade tumours show more tumour-associated macrophages and lower TGF-beta1 expression in colon carcinoma: a retrospective study. BMC Cancer 7:156. https://doi.org/10.1186/1471-2407-7-156
Cavnar MJ, Turcotte S, Katz SC, Kuk D, Gönen M, Shia J, Allen PJ, Balachandran VP, D’Angelica MI, Kingham TP, Jarnagin WR, DeMatteo RP (2017) Tumor-associated macrophage infiltration in colorectal cancer liver metastases is associated with better outcome. Ann Surg Oncol 24(7):1835–1842. https://doi.org/10.1245/s10434-017-5812-8
Chaput N, Svrcek M, Auperin A, Locher C, Drusch F, Malka D, Taieb J, Goere D, Ducreux M, Boige V (2013) Tumour-infiltrating CD68+ and CD57+ cells predict patient outcome in stage II-III colorectal cancer. Br J Cancer 109(4):1013–1022. https://doi.org/10.1038/bjc.2013.362
Climent M, Ryan ÉJ, Stakelum Á, Khaw YL, Creavin B, Lloyd A, Alhassan D, Mohan HM, Kennelly R, Sheahan K, Winter DC (2019) Systemic inflammatory response predicts oncological outcomes in patients undergoing elective surgery for mismatch repair-deficient colorectal cancer. Int J Color Dis 34(6):1069–1078. https://doi.org/10.1007/s00384-019-03274-6
Dost Gunay FS, Kırmızı BA, Ensari A, İcli F, Akbulut H (2019) Tumor-associated macrophages and neuroendocrine differentiation decrease the efficacy of Bevacizumab plus chemotherapy in patients with advanced colorectal cancer. Clin Colorectal Cancer 18(2):e244–e250. https://doi.org/10.1016/j.clcc.2018.12.004
Forssell J, Oberg A, Henriksson ML, Stenling R, Jung A, Palmqvist R (2007) High macrophage infiltration along the tumor front correlates with improved survival in colon cancer. Clin Cancer Res 13(5):1472–1479. https://doi.org/10.1158/1078-0432.Ccr-06-2073
Funada Y, Noguchi T, Kikuchi R, Takeno S, Uchida Y, Gabbert HE (2003) Prognostic significance of CD8+ T cell and macrophage peritumoral infiltration in colorectal cancer. Oncol Rep 10(2):309–313
Gulubova M, Ananiev J, Yovchev Y, Julianov A, Karashmalakov A, Vlaykova T (2013) The density of macrophages in colorectal cancer is inversely correlated to TGF-β1 expression and patients’ survival. J Mol Histol 44(6):679–692. https://doi.org/10.1007/s10735-013-9520-9
Herrera M, Herrera A, Domínguez G, Silva J, García V, García JM, Gómez I, Soldevilla B, Muñoz C, Provencio M, Campos-Martin Y, García de Herreros A, Casal I, Bonilla F, Peña C (2013) Cancer-associated fibroblast and M2 macrophage markers together predict outcome in colorectal cancer patients. Cancer Sci 104(4):437–444. https://doi.org/10.1111/cas.12096
Jakubowska K, Koda M, Kisielewski W, Kańczuga-Koda L, Famulski W (2019) Prognostic significance of inflammatory cell response in patients with colorectal cancer. Oncol Lett 18(1):783–791. https://doi.org/10.3892/ol.2019.10343
Khorana AA, Ryan CK, Cox C, Eberly S, Sahasrabudhe DM (2003) Vascular endothelial growth factor, CD68, and epidermal growth factor receptor expression and survival in patients with stage II and stage III colon carcinoma: a role for the host response in prognosis. Cancer 97(4):960–968. https://doi.org/10.1002/cncr.11152
Klintrup K, Mäkinen JM, Kauppila S, Väre PO, Melkko J, Tuominen H, Tuppurainen K, Mäkelä J, Karttunen TJ, Mäkinen MJ (2005) Inflammation and prognosis in colorectal cancer. Eur J Cancer 41(17):2645–2654
Li S, Xu F, Zhang J, Wang L, Zheng Y, Wu X, Wang J, Huang Q, Lai M (2018) Tumor-associated macrophages remodeling EMT and predicting survival in colorectal carcinoma. OncoImmunology 7(2):e1380765. https://doi.org/10.1080/2162402X.2017.1380765
Shabo I, Olsson H, Elkarim R, Sun XF, Svanvik J (2014) Macrophage infiltration in tumor stroma is related to tumor cell expression of CD163 in colorectal cancer. Cancer Microenviron 7(1–2):61–69. https://doi.org/10.1007/s12307-014-0145-7
Shibutani M, Maeda K, Nagahara H, Fukuoka T, Nakao S, Matsutani S, Hirakawa K, Ohira M (2017) The peripheral monocyte count is associated with the density of tumor-associated macrophages in the tumor microenvironment of colorectal cancer: a retrospective study. BMC Cancer 17(1):404. https://doi.org/10.1186/s12885-017-3395-1
Tan SY, Fan Y, Luo HS, Shen ZX, Guo Y, Zhao LJ (2005) Prognostic significance of cell infiltrations of immunosurveillance in colorectal cancer. World J Gastroenterol 11(8):1210–1214. https://doi.org/10.3748/wjg.v11.i8.1210
Waniczek D, Lorenc Z, Śnietura M, Wesecki M, Kopec A, Muc-Wierzgoń M (2017) Tumor-associated macrophages and regulatory T cells infiltration and the clinical outcome in colorectal cancer. Arch Immunol Ther Exp 65(5):445–454. https://doi.org/10.1007/s00005-017-0463-9
Wei C, Yang C, Wang S, Shi D, Zhang C, Lin X, Liu Q, Dou R, Xiong B (2019) Crosstalk between cancer cells and tumor associated macrophages is required for mesenchymal circulating tumor cell-mediated colorectal cancer metastasis. Mol Cancer 18(1):64. https://doi.org/10.1186/s12943-019-0976-4
Zhou Q, Peng RQ, Wu XJ, Xia Q, Hou JH, Ding Y, Zhou QM, Zhang X, Pang ZZ, Wan DS, Zeng YX, Zhang XS (2010) The density of macrophages in the invasive front is inversely correlated to liver metastasis in colon cancer. J Transl Med 8:13. https://doi.org/10.1186/1479-5876-8-13
Kang JC, Chen JS, Lee CH, Chang JJ, Shieh YS (2010) Intratumoral macrophage counts correlate with tumor progression in colorectal cancer. J Surg Oncol 102(3):242–248. https://doi.org/10.1002/jso.21617
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674. https://doi.org/10.1016/j.cell.2011.02.013
Kono H, Fujii H, Furuya S, Hara M, Hirayama K, Akazawa Y, Nakata Y, Tsuchiya M, Hosomura N, Sun C (2016) Macrophage colony-stimulating factor expressed in non-cancer tissues provides predictive powers for recurrence in hepatocellular carcinoma. World J Gastroenterol 22(39):8779–8789
Li Z, Maeda D, Yoshida M, Umakoshi M, Nanjo H, Shiraishi K, Saito M, Kohno T, Konno H, Saito H, Minamiya Y, Goto A (2018) The intratumoral distribution influences the prognostic impact of CD68- and CD204-positive macrophages in non-small cell lung cancer. Lung Cancer 123:127–135. https://doi.org/10.1016/j.lungcan.2018.07.015
Pelekanou V, Villarroel-Espindola F, Schalper KA, Pusztai L, Rimm DL (2018) CD68, CD163, and matrix metalloproteinase 9 (MMP-9) co-localization in breast tumor microenvironment predicts survival differently in ER-positive and -negative cancers. Breast Cancer Res 20(1):154. https://doi.org/10.1186/s13058-018-1076-x
Grizzi F, Bianchi P, Malesci A, Laghi L (2013) Prognostic value of innate and adaptive immunity in colorectal cancer. World J Gastroenterol 19(2):174–184. https://doi.org/10.3748/wjg.v19.i2.174
Kong JC, Guerra GR, Pham T, Mitchell C, Lynch AC, Warrier SK, Ramsay RG, Heriot AG (2019) Prognostic impact of tumor-infiltrating lymphocytes in primary and metastatic colorectal cancer: a systematic review and meta-analysis. Dis Colon Rectum 62(4):498–508. https://doi.org/10.1097/dcr.0000000000001332
Dehai C, Bo P, Qiang T, Lihua S, Fang L, Shi J, Jingyan C, Yan Y, Guangbin W, Zhenjun Y (2014) Enhanced invasion of lung adenocarcinoma cells after co-culture with THP-1-derived macrophages via the induction of EMT by IL-6. Immunol Lett 160(1):1–10. https://doi.org/10.1016/j.imlet.2014.03.004
Singh R, Shankar BS, Sainis KB (2014) TGF-β1-ROS-ATM-CREB signaling axis in macrophage mediated migration of human breast cancer MCF7 cells. Cell Signal 26(7):1604–1615. https://doi.org/10.1016/j.cellsig.2014.03.028
Funding
The work was supported by the National Basic Research Program of China (973 program, J.L., Grant #2015CB932600), the National Natural Science Foundation of China (J.L., No. 81472735); Wuhan University (J.L., 2042019kf0206).
Author information
Authors and Affiliations
Contributions
All the authors designed the study. Data were collected by Zhenwei Yang, Mengna Zhang, Ruyi Peng, and Jialong Liu. Quality control of data was performed by Fan Wang and Yizhang Li. All authors analyzed the data. Zhenwei Yang and Mengna Zhang wrote the first draft of article. All authors revised the article and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This is a meta-analysis, no ethical approval is required.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, Z., Zhang, M., Peng, R. et al. The prognostic and clinicopathological value of tumor-associated macrophages in patients with colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis 35, 1651–1661 (2020). https://doi.org/10.1007/s00384-020-03686-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03686-9