Abstract
Background
Compromised wound healing following stoma reversal is a frequent problem. The use of negative suction drainage for reduction of complications remains controversial.
Methods
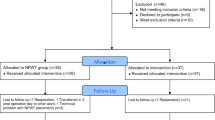
The patient database of our center was reviewed for patients with ileostomy reversal between 2007 and 2017. Risk factors for wound complications were analyzed using multivariate regression analysis. Systematic review and meta-analysis was performed. Ultimately, results of this study were integrated into meta-analysis to assess the effect of drainage placement on wound healing.
Results
In our institutional analysis, a total of 406 patients with ileostomy reversal were included (n = 240 (59.1%) with drainage vs. n = 166 (40.8%) without drainage). In multivariate analysis, body mass index (BMI) was a risk factor for wound complications (odds ratio (95% CI) 1.06 (1.02–1.12)). Patients with drainage needed significantly fewer interventions than those without drainage (17.1% vs. 28.9%, p = 0.005). Placement of drainage significantly reduced the risk of wound complications even in the group with elevated BMI (odds ratio (95% CI) 0.462 (0.28–0.76), p = 0.003). Meta-analysis identified 6 studies with a total of 1180 patients eligible for further analysis (2 prospectively randomized trials; 4 retrospective cohort studies). Overall analysis revealed a significantly beneficial effect of wound drainage following ileostomy reversal (RR (95% CI) 0.47 (0.34, 0.66); p < 0.0001).
Conclusion
In our institutional analysis as well as meta-analysis, the use of subcutaneous suction drains was beneficial for prevention of wound healing complications following ostomy reversal. Drainage placement is especially valuable in high-risk situations such as in obese patients.



Similar content being viewed by others
References
Mrak K, Uranitsch S, Pedross F, Heuberger A, Klingler A, Jagoditsch M, Weihs D, Eberl T, Tschmelitsch J (2016) Diverting ileostomy versus no diversion after low anterior resection for rectal cancer: a prospective, randomized, multicenter trial. Surgery 159:1129–1139
Huser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J, Friess H (2008) Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg 248:52–60
Ulrich AB, Seiler C, Rahbari N, Weitz J, Buchler MW (2009) Diverting stoma after low anterior resection: more arguments in favor. Dis Colon Rectum 52:412–418
Bhama AR, Batool F, Collins SD, Ferraro J, Cleary RK (2017) Risk factors for postoperative complications following diverting loop ileostomy takedown. J Gastrointest Surg 21:2048–2055
Schneider V, Lee LD, Stroux A, Buhr HJ, Ritz JP, Kreis ME, Lauscher JC (2016) Risk factors for reoperation after ileostomy reversal - results from a prospective cohort study. Int J Surg 36:233–239
Mansfield SD, Jensen C, Phair AS, Kelly OT, Kelly SB (2008) Complications of loop ileostomy closure: a retrospective cohort analysis of 123 patients. World J Surg 32:2101–2106
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Kosins AM, Scholz T, Cetinkaya M, Evans GR (2013) Evidence-based value of subcutaneous surgical wound drainage: the largest systematic review and meta-analysis. Plast Reconstr Surg 132:443–450
Pan HD, Wang L, Peng YF, Li M, Yao YF, Zhao J, Zhan TC, Du CZ, Gu J (2015) Subcutaneous vacuum drains reduce surgical site infection after primary closure of defunctioning ileostomy. Int J Color Dis 30:977–982
Chu DI, Schlieve CR, Colibaseanu DT, Simpson PJ, Wagie AE, Cima RR, Habermann EB (2015) Surgical site infections (SSIs) after stoma reversal (SR): risk factors, implications, and protective strategies. J Gastrointest Surg 19:327–334
Mirbagheri N, Dark J, Skinner S (2013) Factors predicting stomal wound closure infection rates. Tech Coloproctol 17:215–220
Thomson JP, Hawley PR (1972) Results of closure of loop transverse colostomies. Br Med J 3:459–462
Lauscher JC, Schneider V, Lee LD, Stroux A, Buhr HJ, Kreis ME, Ritz JP (2016) Necessity of subcutaneous suction drains in ileostomy reversal (DRASTAR)-a randomized, controlled bi-centered trial. Langenbeck's Arch Surg 401:409–418
Liang MK, Li LT, Avellaneda A, Moffett JM, Hicks SC, Awad SS (2013) Outcomes and predictors of incisional surgical site infection in stoma reversal. JAMA Surg 148:183–189
O’Leary DP, Carter M, Wijewardene D, Burton M, Waldron D, Condon E, Coffey JC, Peirce C (2017) The effect of purse-string approximation versus linear approximation of ileostomy reversal wounds on morbidity rates and patient satisfaction: the ‘STOMA’ trial. Tech Coloproctol 21:863–868
McCartan DP, Burke JP, Walsh SR, Coffey JC (2013) Purse-string approximation is superior to primary skin closure following stoma reversal: a systematic review and meta-analysis. Tech Coloproctol 17:345–351
Hajibandeh S, Hajibandeh S, Kennedy-Dalby A, Rehman S, Zadeh RA (2018) Purse-string skin closure versus linear skin closure techniques in stoma closure: a comprehensive meta-analysis with trial sequential analysis of randomised trials. Int J Color Dis 33:1319–1332
Dusch N, Goranova D, Herrle F, Niedergethmann M, Kienle P (2013) Randomized controlled trial: comparison of two surgical techniques for closing the wound following ileostomy closure: purse string vs direct suture. Color Dis 15:1033–1040
Khansa I, Khansa L, Meyerson J, Janis JE (2018) Optimal use of surgical drains: evidence-based strategies. Plast Reconstr Surg 141:1542–1549
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the ethical board of the Technical University of Munich (No. 207/18s).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Neumann, PA., Reischl, S., Berg, F. et al. Meta-analysis and single-center experience on the protective effect of negative suction drains on wound healing after stoma reversal. Int J Colorectal Dis 35, 403–411 (2020). https://doi.org/10.1007/s00384-019-03492-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03492-y