Abstract
Purpose
This study aimed to evaluate the prognostic value of circulating tumor cells (CTCs) in advanced colorectal cancer (CRC) patients during chemotherapy course.
Methods
From January 2016 to September 2017, the clinicopathological variables, such as gender, age, tumor location, tumor de-differentiation, depth of invasion, lymphatic invasion, distant metastasis, TNM stage, CTCs enumeration during 2-6 cycles of chemotherapy, and serum carcinoembryonic antigen (CEA) level during the same period, of 121 newly acquired and histopathologically confirmed CRC patients were collected from the Shanghai Ninth People’s Hospital affiliated to Shanghai Jiao Tong University School of Medicine. All patients were followed up for survival until the end of November 2018. Statistical analysis focused on the associations between CTCs counts and clinicopathological variables. Overall survival (OS) and progression-free survival (PFS) among different prognostic factors were calculated using the Kaplan–Meier method, and the differences between the survival curves were compared by using the log-rank test. Factors of prognostic significance were investigated with the multivariate Cox regression analysis.
Results
Here, 71 of 121 patients were CTC-positive, in which CTC-positive rate was positively correlated with the depth of invasion, lymphatic invasion, distant metastasis, TNM stage, and serum CEA level (P < 0.05 for all). However, no significant difference was found between CTC-positive and other clinicopathological variables (P > 0.05 for all), such as gender, age, tumor location, and tumor de-differentiation. CTCs counts gradually increased with the advancement of depth of invasion (P = 0.002), lymphatic invasion (P = 0.004), distant metastasis (P = 0.007), TNM stage (P = 0.001), serum CEA level (P = 0.001), and decreased tumor de-differentiation (P = 0.011). Furthermore, the Kaplan–Meier survival curves showed that patients with CTC-positive had a significantly unfavorable PFS (14 vs. 23 months, P = 0.001) and OS (18 vs. 25 months, P = 0.003). The multivariate Cox regression analyses revealed that the presence of CTCs during chemotherapy was an independent factor for unfavorable PFS (hazard ratio (HR) 2.682, P = 0.017, 95% confidence interval (CI) 1.193–6.029) and OS (HR 2.790, P = 0.048, 95% CI 1.010–7.705) in advanced CRC patients.
Conclusions
This study provided an evidence that the presence of CTCs may be valuable for predicting survival outcome, and CTCs was associated with unfavorable survival in advanced CRC patients during chemotherapy.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most common tumor in men and women worldwide [1]. Due to the lack of effective methods for early diagnosis, in which 15–20% of patients with CRC were diagnosed with liver metastasis at the first time of diagnosis, and the remaining 60% would have recurrence or metastasis during subsequent treatment [2]. These poor outcomes are associated with the fact that the majority of patients are diagnosed at advanced stage (III/IV stage), with distant metastasis, lymphatic dissemination, and recurrence [3]. Although tremendous efforts at diagnosis and treatment have been made for advanced CRC patients, several patients benefit from chemotherapy to some extent. Overall survival (OS) is currently approaching 30 months for the patients treated with the combination of cytotoxic chemotherapy and biologic agents, targeting angiogenesis and the epidermal growth factor receptor (EGFR), which inhibit signal transduction pathways [4,5,6,7]. However, some patients who did not respond to these systemic treatments still have a dismal outcome. Indeed, approximately 28–44% of patients are ineffective to the first-line treatment with doublet chemotherapy plus either cetuximab or bevacizumab, and about 50% of these patients have postoperative recurrence or distant metastasis [8]. In addition, excessive chemotherapy leads to various side effects that seriously decrease the life quality of patients [9]. Therefore, there is of great importance to develop a more accurate method to identify patients with poor prognosis or with rapid disease progression, in which identification of more reliable predictive biomarkers to chemotherapy make them to be directed towards the most effective treatment for clinical precise management of CRC [10].
Circulating tumor cells (CTCs) are heterogeneous tumor cells that have escaped from the primary or metastatic tumor site and gained access to the vasculature through intravasation [11]. In recent years, several retrospective and prospective studies have indicated CTCs counts could be used as a strong and independent prognostic or predictive biomarker for efficient chemotherapy in breast, prostate, and CRC patients [12,13,14,15]. Romiti et al. detected CTCs of CRC patients 1 month after the first cycle of chemotherapy, and reported that CTCs can predict the prognosis [16]. Another clinical trial demonstrated that CTCs could be as a feasible and non-invasive approach to assess the current molecular characteristics of prostate cancer. Similar data were reported, and also demonstrated that CTCs could be used as predictive biomarkers for designing individually tailored therapy against CRC [17]. In general, CTCs have been widely taken as a non-invasive “liquid biopsy” of cancer into account. The counts and characteristic analysis of CTCs have shown their great application potential in both prognostication and treatment of CRC patients.
Materials and methods
Patients and data collection
From January 2016 to September 2017, 121 patients with advanced CRC were recruited in this retrospective study from the Shanghai Ninth People’s Hospital affiliated to Shanghai Jiao Tong University School of Medicine (Shanghai, China).
The inclusion criteria were as follows: (1) age > 18 years old; (2) ALL patients obtained confirmed pathological diagnosis and complete clinicopathological variables, including gender, age, tumor location, tumor de-differentiation, depth of invasion, lymphatic invasion, distant metastasis, TNM stage, CTCs counts, and CEA level during the same period; (3) The peripheral blood samples for detection of CTCs from patients were collected during two–six cycles of chemotherapy; (4) patients received 5-fluorouracil (5-FU) or capecitabine-based chemotherapy (with or without targeted therapy); and (5) patients voluntarily joined the study and signed the informed consent form, with a good compliance and follow-up.
The exclusion criteria were as follows: (1) evidence of the second primary tumor; (2) previous radiotherapy and biological immunotherapy; and (3) with other serious diseases which may affect the prognosis.
The TNM stage of CRC was classified according to American Joint Committee on Cancer (AJCC, the eighth edition, 2017). All patients signed the informed consent form. The study was approved by the Ethics Committee of the Shanghai Ninth People’s Hospital affiliated to Shanghai Jiao Tong University School of Medicine.
OS is defined as the time from blood collection for detection of CTCs to death, and PFS is defined as the period from blood collection for detection of CTCs until disease progression during or after chemotherapy course. Tumor response was evaluated by computed tomography (CT) scanning or magnetic resonance imaging (MRI) according to the response evaluation criteria in solid tumors (RECIST 1.1) every 8–12 weeks during or after chemotherapy course. All patients were followed up until death or the end of November 2018.
CTCs detection
Here, 5 ml peripheral blood sample of advanced CRC patients was collected during treatment. The CTCs detection was performed by the Cyttel method, and immunomagnetic bead-negative enrichment technique combined with immunofluorescence in situ hybridization technologies (imFISH) method was adopted to find out CTCs counts. The protocol of CTCs detection was as follows: First, leukocytes were specifically removed by lysing red blood cells and immunomagnetic beads, and the rarest cells in peripheral blood samples were retained. Secondly, the procedure was performed by using CD45-negative and chromosome polyploidy characteristics in tumor cells, in addition to CD45 staining of the remaining rare cells and imFISH of chromosomes 8 and 17 H1 fluorescent probes, combined with DAPI staining. It can avoid the epithelial-mesenchymal transition on epithelial cell adhesion molecules and effectively improve the detection rate of CTCs. In this study, all 121 patients underwent CTC test. Besides, CTCs ≥ 3 were considered to be CTC-positive, and correspondingly CTC < 3 were considered to be CTC-negative. According to the criteria for CTC interpretation, among 121 CRC patients, 71 cases were classified as CTC-positive group, while 50 cases were classified as CTC-negative group. The positive detection rate was 58.7% (71/121) as well.
Statistical analysis
All the statistical analyses were performed using SPSS 22.0 software (IBM, Armonk, NY, USA). Pearson’s chi-square test was used to analyze the differences in the CTC-positive and CTC-negative groups. The Mann–Whitney U test or Kruskal–Wallis H test was used to compare the CTCs counts among different groups, as appropriate. OS and PFS among different prognostic categories were calculated using the Kaplan–Meier method, and significant differences between the survival curves were compared by using the log-rank test. Based on the univariate analyses of all variables, only variables with a P value < 0.05 were included for analysis in the multivariate Cox regression model to investigate the influence of independent factors on OS and PFS. All statistical analyses were 2-sided, and a P value < 0.05 was statistically considered significant. Graphical plots were generated using GraphPad prism 7.0 software (GraphPad Software, La Jolla, CA, USA).
Data availability
The datasets used during the present study are available from the corresponding author upon reasonable request.
Results
Patients’ characteristics
The clinical characteristics of 121 advanced CRC patients is shown in Table 1. Of all the cases, the median age was 65 years (range 34–89 years), 78 (64.5%) were males, and 43 (35.5%) were females. The primary tumors were found from colon and rectum in 76 and 45 patients, respectively. In terms of histological differentiation subtypes, 58 patients were poorly differentiated adenocarcinoma, followed by 63 patients with moderately and well-differentiated subtypes. According to the TNM stage, there were 13 cases with stage IIIa, 29 cases with stage IIIb, 29 cases with stage IIIc, 26 cases with stage IVa, and 24 cases with stage IVb. All the patients received 5-FU or capecitabine-based chemotherapy (with or without targeted therapy). None of the patients with TNM stage IV underwent metastases resection before chemotherapy.
The relationship between CTCs and clinicopathological variables in advanced CRC patients with treatment
The association of CTC-positive rate with the clinicopathological variables is shown in Table 2. CTC-positive rate was positively correlated with depth of invasion, lymphatic invasion, distant metastasis, TNM stage, and serum CEA level (P < 0.05 for all). By contrast, no significant association was found between CTC-positive rate and other clinicopathological variables (P > 0.05 for all), such as gender, age, tumor location, and tumor de-differentiation.
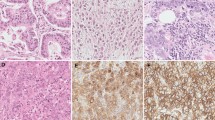
Furthermore, CTC counts for all 121 advanced CRC patients ranged from 0 to 30 (mean ± standard error (SE) 5.19 ± 5.50). In addition, there was a significant increase in CTCs counts with the decrease of tumor de-differentiation, high serum CEA level, depth of invasion, lymphatic invasion, distant metastasis, and TNM stage (Fig. 1a–f).
The relationship between CTCs counts and clinicopathological characteristics in advanced CRC patients. a The correlation of CTCs counts with tumor de-differentiation (poor vs. well to moderate, P = 0.011). b The correlation of CTCs counts with serum CEA level (P = 0.001). c The correlation of CTCs counts with depth of invasion (T1 vs. T4b, P = 0.053; T2 vs. T4b, P < 0.001; T3 vs. T4b, P = 0.013; T4a vs. T4b, P = 0.026). d The correlation of CTCs counts with lymphatic invasion (N1 vs. N2a, P = 0.395; N1 vs. N2b, P = 0.010). e The correlation of CTCs counts with distant metastasis (M0 vs. M1a, P = 0.242; M0 vs. M1b, P = 0.014). f The correlation of CTCs counts with TNM stage (IIIa vs. IVb, P < 0.001; IIIb vs. IVb, P = 0.005; IIIc vs. IVb, P = 0.225; IVa vs. IVb, P = 0.319)
Univariate and multivariate analyses
During the follow-up period, 40 (33.1%) patients were evaluated for disease progression, 28 (23.1%) patients died, and all died of colorectal cancer. The median follow-up time was 14 months (range 8–27 months).
The results of the univariate analysis for OS and PFS that were associated with the clinical variables are presented in Table 3. Based on the univariate analysis, 6 of the 11 preselected variables, including high serum CEA level, tumor de-differentiation, lymphatic invasion, distant metastasis, TNM stage, and CTC-positive were closely associated with unfavorable PFS (Table 3). However, the multivariate Cox regression analysis further revealed that the CTC-positive, lymphatic invasion, and distant metastasis were independent prognostic factors for unfavorable PFS (Table 4). Besides, the Kaplan–Meier survival curves showed that advanced CRC patients with CTC-positive had a significantly unfavorable PFS (14 vs. 23 months, P = 0.001) (Fig. 2a).
Regarding the OS of all the patients, 7 of the 11 preselected variables, including high serum CEA level, lymphatic invasion, distant metastasis, TNM stage, tumor de-differentiation, tumor location, and CTC-positive were significant variables in the univariate analysis (Table 3). However, the multivariate Cox regression analysis further revealed that CTCs, lymphatic invasion, and distant metastasis were independent prognostic factors for unfavorable OS (Table 4). Additionally, the Kaplan–Meier survival curves showed that advanced CRC patients with CTC-positive had a significantly unfavorable OS (18 vs. 25 months, P = 0.003) (Fig. 2b).
Discussion
CRC is one of the most common malignant tumors. Recurrence and metastasis are important reasons, affecting the prognosis of CRC. Micrometastasis is an early event of distant metastasis of the tumor. How to detect the recurrence and metastasis of CRC earlier, how to quickly assess the need for adjuvant chemotherapy and chemotherapeutic drug sensitivity for CRC patients, and how to improve the treatment plan in time before the disease progression have become the main challenges during CRC treatment. In recent years, CTCs have been considered as a liquid biopsy for all solid tumors. The technique of isolation and analyzation of CTCs has been shown to be a highly repeatable, and minimally invasive technique for diagnosis, prognosis, and real-time monitoring of drug resistance for cancer treatment [18, 19]. Previous studies have indicated that CTCs are closely associated with the biological behavior of tumor. The existence of CTCs may be a basis for distant metastasis [20, 21]. Besides, there is growing evidence that CTCs might become as a reliable clinical marker for diagnosis and prognosis [22,23,24].
Since CTCs are derived from tumor tissue, the CTCs counts can reflect the tumor burden in patients to some extent. A number of studies have indicated that CTCs can indicate clinical features, such as tumor invasion and lymph node metastasis in patients with CRC. Our study revealed the relationship between CTCs and the clinicopathological characteristics of CRC. It was disclosed that CTC-positive rate was positively and dependently correlated with the pathological stage of tumor. Further refinement of the TNM stage revealed that CTCs were also associated with primary tumor depth of invasion, lymphatic invasion, and distant metastasis. In addition, CTC counts increased along with tumor pathological stage, primary tumor depth of invasion, lymphatic invasion, and distant metastasis. These results suggest that both CTC-positive rates and CTCs counts have positively correlated with lymphatic invasion and the appearance of distant metastases, which make the use of CTCs feasible to evaluate lymphatic invasion and distant metastasis. CTCs are the root cause of tumor metastasis, and their relationship with lymphatic invasion may be similar to tumor angiogenesis and lymphangiogenesis, and are associated with the regulation of vascular endothelial growth factor (VEGF) and its receptors [25, 26]. Moreover, serum CEA values were higher in CTC-positive patients than those in CTC-negative patients. To our knowledge, serum CEA level was used as a specific marker of intestinal tumors in several prognostic scoring systems. A positive correlation between CTC-positive rate and serum CEA level indicates that CTCs could be associated with a higher risk of tumor progression. In addition, the study found determination of CTCs is more significant than post-chemotherapy CEA level in predicting survival outcome. The above-mentioned results are consistent with the results of previous studies [27, 28]. In brief, CTCs could play an important role in predicting the processes of tumor progression and metastasis development, which could be universally applied in cancer screening.
Recurrence and metastasis are important factors, affecting the prognosis of CRC patients. In addition to reflecting the aggressiveness of the disease, CTC counts represent as a potential complementary method to predict the outcome of CRC patients. The study also found that the presence of CTCs was associated with poor survival in advanced CRC patients during chemotherapy course, and the multivariate Cox regression analysis further identified that CTCs was an independent prognostic factor for OS and PFS, which was consistent with previous studies [29,30,31]. Galizia et al. recently reported that 75% of 69 CRC patients undergoing radical surgery with more postoperative CTCs counts experienced tumor recurrence. Thus, postoperative CTCs counts could be used as an early indicator for undetectable metastasis [32].
According to previous studies, the relationship between CTCs detection and prognosis during treatment was more significant and convincing compared with the CTCs at baseline [13, 14, 33]. That was the reason why we recruited CTCs counts of advanced CRC patients with two–six cycles of chemotherapy course to predict outcomes in the present study. In addition, CTCs were divided into three phenotypes based on differences in cell-surface biomarker expression levels: epithelial tumor cells, tumor cells undergoing epithelial-to-mesenchymal transition (EMT), and tumor stem cells. The current standard method is on the basis of CellSearch System approved by the United States Food and Drug Administration (FDA), utilizing ferrofluids loaded with an EpCAM antibody to capture the epithelial CTCs, but not CTCs that have undergone EMT [34, 35]. Notably, it was suggested that not only epithelial, but also mesenchymal markers in cell-surface of CTCs could offer valuable assistance for metastasis evaluation and tumor staging in CRC patients. In this study, phenotype of CTCs was measured by immunomagnetic bead-negative enrichment technique combined with imFISH. It avoids the EMT through the epithelial cell adhesion molecules and effectively improves the detection rate of CTCs.
To the best of our knowledge, this is a much larger retrospective study using a negative selection method for CTCs isolation to evaluate its prognostic value in advanced CRC patients. Based on our results, CTCs might be widely available to be used as a prognostic and predictive factor in advanced CRC patients who underwent chemotherapy. However, there are still several inherent limitations. First of all, as our results are based on a single-center retrospective study, with a relatively small sample size, the statistical impact of clinical variables on survival might be the modest. More samples with large size are required for stratified analyses to improve the treatment, in addition to provide more accurate information for evidence-based medicine. Another limitation is the lack of dynamic enumeration of CTCs. The dynamic enumeration of CTCs could better reflect the aggressiveness and prognosis of the disease than the isolated enumeration of CTCs [36]. However, it was difficult for us to compare the baseline (pretreatment) level of CTCs with the level at follow-up. Cause treatment interventions (including surgery and chemotherapy), as we know, can reduce CTCs counts, even to negative.
In conclusion, CTCs may serve as an independent prognostic factor in terms of PFS and OS in advanced CRC patients during chemotherapy course. Therefore, including the detection of CTCs in the blood in the future treatment guidelines is highly recommended. However, the significant role of CTCs for CRC patients should be further validated in large-scale prospective trials.
References
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Kemeny N (2010) The management of resectable and unresectable liver metastases from colorectal cancer. Curr Opin Oncol 22(4):364–373. https://doi.org/10.1097/CCO.0b013e32833a6c8a
Tzeng CW, Aloia TA (2013) Colorectal liver metastases. J Gastrointest Surg 17(1):195–201; quiz p 201–192. https://doi.org/10.1007/s11605-012-2022-3
Liu Y, Luan L, Wang X (2015) A randomized phase II clinical study of combining panitumumab and bevacizumab, plus irinotecan, 5-fluorouracil, and leucovorin (FOLFIRI) compared with FOLFIRI alone as second-line treatment for patients with metastatic colorectal cancer and KRAS mutation. OncoTargets Therapy 8:1061–1068. https://doi.org/10.2147/OTT.S81442
Cao R, Zhang S, Ma D, Hu L (2015) A multi-center randomized phase II clinical study of bevacizumab plus irinotecan, 5-fluorouracil, and leucovorin (FOLFIRI) compared with FOLFIRI alone as second-line treatment for Chinese patients with metastatic colorectal cancer. Med Oncol 32(1):325. https://doi.org/10.1007/s12032-014-0325-9
Nakayama G, Ishigure K, Yokoyama H, Uehara K, Kojima H, Ishiyama A, Hayashi N, Takano N, Hattori N, Kobayashi D, Tanaka C, Hayashi M, Kanda M, Yamada S, Sugimoto H, Koike M, Fujiwara M, Fujii T, Murotani K, Ando Y, Kodera Y (2017) The efficacy and safety of CapeOX plus bevacizumab therapy followed by capecitabine plus bevacizumab maintenance therapy in patients with metastatic colorectal cancer: a multi-center, single-arm, phase II study (CCOG-0902). BMC Cancer 17(1):243. https://doi.org/10.1186/s12885-017-3245-1
Takata K, Fujita KI, Kubota Y, Ishida H, Ichikawa W, Shimada K, Sekikawa T, Taki-Takemoto I, Kamei D, Iwai S, Sasaki Y (2016) Cost-minimization analysis of adjuvant chemotherapy regimens given to patients with colorectal cancer in Japan. J Pharm Health Care Sci 2:30. https://doi.org/10.1186/s40780-016-0064-5
Heinemann V, von Weikersthal LF, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran S-E, Heintges T, Lerchenmüller C, Kahl C, Seipelt G, Kullmann F, Stauch M, Scheithauer W, Hielscher J, Scholz M, Müller S, Link H, Niederle N, Rost A, Höffkes H-G, Moehler M, Lindig RU, Modest DP, Rossius L, Kirchner T, Jung A, Stintzing S (2014) FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol 15(10):1065–1075. https://doi.org/10.1016/s1470-2045(14)70330-4
Hazama S, Nakamura Y, Tanaka H, Hirakawa K, Tahara K, Shimizu R, Ozasa H, Etoh R, Sugiura F, Okuno K, Furuya T, Nishimura T, Sakata K, Yoshimatsu K, Takenouchi H, Tsunedomi R, Inoue Y, Kanekiyo S, Shindo Y, Suzuki N, Yoshino S, Shinozaki H, Kamiya A, Furukawa H, Yamanaka T, Fujita T, Kawakami Y, Oka M (2014) A phase IotaI study of five peptides combination with oxaliplatin-based chemotherapy as a first-line therapy for advanced colorectal cancer (FXV study). J Transl Med 12:108. https://doi.org/10.1186/1479-5876-12-108
Stein A, Atanackovic D, Bokemeyer C (2011) Current standards and new trends in the primary treatment of colorectal cancer. Eur J Cancer 47:S312–S314. https://doi.org/10.1016/s0959-8049(11)70183-6
Liberko M, Kolostova K, Bobek V (2013) Essentials of circulating tumor cells for clinical research and practice. Crit Rev Oncol Hematol 88(2):338–356. https://doi.org/10.1016/j.critrevonc.2013.05.002
Masuda T, Hayashi N, Iguchi T, Ito S, Eguchi H, Mimori K (2016) Clinical and biological significance of circulating tumor cells in cancer. Mol Oncol 10(3):408–417. https://doi.org/10.1016/j.molonc.2016.01.010
de Albuquerque A, Kubisch I, Stolzel U, Ernst D, Boese-Landgraf J, Breier G, Stamminger G, Fersis N, Kaul S (2012) Prognostic and predictive value of circulating tumor cell analysis in colorectal cancer patients. J Transl Med 10:222. https://doi.org/10.1186/1479-5876-10-222
Wallwiener M, Riethdorf S, Hartkopf AD, Modugno C, Nees J, Madhavan D, Sprick MR, Schott S, Domschke C, Baccelli I, Schonfisch B, Burwinkel B, Marme F, Heil J, Sohn C, Pantel K, Trumpp A, Schneeweiss A (2014) Serial enumeration of circulating tumor cells predicts treatment response and prognosis in metastatic breast cancer: a prospective study in 393 patients. BMC Cancer 14:512. https://doi.org/10.1186/1471-2407-14-512
Lack J, Gillard M, Cam M, Paner GP, VanderWeele DJ (2017) Circulating tumor cells capture disease evolution in advanced prostate cancer. J Transl Med 15(1):44. https://doi.org/10.1186/s12967-017-1138-3
Romiti A, Raffa S, Di Rocco R, Roberto M, Milano A, Zullo A, Leone L, Ranieri D, Mazzetta F, Medda E, Sarcina I, Barucca V, D'Antonio C, Durante V, Ferri M, Torrisi MR, Marchetti P (2014) Circulating tumor cells count predicts survival in colorectal cancer patients. J Gastrointest Liver Dis: JGLD 23(3):279–284. https://doi.org/10.15403/jgld.2014.1121.233.arom1
Huang MY, Tsai HL, Huang JJ, Wang JY (2016) Clinical implications and future perspectives of circulating tumor cells and biomarkers in clinical outcomes of colorectal Cancer. Transl Oncol 9(4):340–347. https://doi.org/10.1016/j.tranon.2016.06.006
Hinz S, Hendricks A, Wittig A, Schafmayer C, Tepel J, Kalthoff H, Becker T, Roder C (2017) Detection of circulating tumor cells with CK20 RT-PCR is an independent negative prognostic marker in colon cancer patients - a prospective study. BMC Cancer 17(1):53. https://doi.org/10.1186/s12885-016-3035-1
Di Meo A, Bartlett J, Cheng Y, Pasic MD, Yousef GM (2017) Liquid biopsy: a step forward towards precision medicine in urologic malignancies. Mol Cancer 16(1):80. https://doi.org/10.1186/s12943-017-0644-5
Lianidou ES, Mavroudis D, Pantel K (2013) Advances in circulating tumor cells (ACTC): from basic research to clinical practice. Breast Cancer Res: BCR 15(6):319. https://doi.org/10.1186/bcr3582
Huang X, Gao P, Song Y, Sun J, Chen X, Zhao J, Xu H, Wang Z (2015) Meta-analysis of the prognostic value of circulating tumor cells detected with the CellSearch System in colorectal cancer. BMC Cancer 15:202. https://doi.org/10.1186/s12885-015-1218-9
Pesta M, Kulda V, Narsanska A, Fichtl J, Topolcan O (2015) May CTC technologies promote better cancer management? EPMA J 6(1):1. https://doi.org/10.1186/s13167-014-0023-x
Gorges TM, Pantel K (2013) Circulating tumor cells as therapy-related biomarkers in cancer patients. Cancer Immunol Immunother: CII 62(5):931–939. https://doi.org/10.1007/s00262-012-1387-1
Yap TA, Lorente D, Omlin A, Olmos D, de Bono JS (2014) Circulating tumor cells: a multifunctional biomarker. Clin Cancer Res 20(10):2553–2568. https://doi.org/10.1158/1078-0432.CCR-13-2664
Borowski DW, Banky B, Banerjee AK, Agarwal AK, Tabaqchali MA, Garg DK, Hobday C, Hegab M, Gill TS (2014) Intra-arterial methylene blue injection into ex vivo colorectal cancer specimens improves lymph node staging accuracy: a randomized controlled trial. Color Dis 16(9):681–689. https://doi.org/10.1111/codi.12681
Patenaude A, Parker J, Karsan A (2010) Involvement of endothelial progenitor cells in tumor vascularization. Microvasc Res 79(3):217–223. https://doi.org/10.1016/j.mvr.2010.01.007
Tsai WS, Chen JS, Shao HJ, Wu JC, Lai JM, Lu SH, Hung TF, Chiu YC, You JF, Hsieh PS, Yeh CY, Hung HY, Chiang SF, Lin GP, Tang R, Chang YC (2016) Circulating tumor cell count correlates with colorectal neoplasm progression and is a prognostic marker for distant metastasis in non-metastatic patients. Sci Rep 6:24517. https://doi.org/10.1038/srep24517
Das A, Kunkel M, Joudeh J, Dicker DT, Scicchitano A, Allen JE, Sarwani N, Yang Z, Kaifi J, Zhu J, Liao J, El-Deiry WS (2015) Clinico-pathological correlation of serial measurement of circulating tumor cells in 24 metastatic colorectal cancer patients receiving chemotherapy reveals interpatient heterogeneity correlated with CEA levels but independent of KRAS and BRAF mutation. Cancer Biol Ther 16(5):709–713. https://doi.org/10.1080/15384047.2015.1030555
Yalcin S, Kilickap S, Portakal O, Arslan C, Hascelik G, Kutluk T (2010) Determination of circulating tumor cells for detection of colorectal cancer progression or recurrence. Hepato-Gastroenterology 57(104):1395–1398
Lu CY, Uen YH, Tsai HL, Chuang SC, Hou MF, Wu DC, Juo SH, Lin SR, Wang JY (2011) Molecular detection of persistent postoperative circulating tumour cells in stages II and III colon cancer patients via multiple blood sampling: prognostic significance of detection for early relapse. Br J Cancer 104(7):1178–1184. https://doi.org/10.1038/bjc.2011.40
Uen YH, Lu CY, Tsai HL, Yu FJ, Huang MY, Cheng TL, Lin SR, Wang JY (2008) Persistent presence of postoperative circulating tumor cells is a poor prognostic factor for patients with stage I-III colorectal cancer after curative resection. Ann Surg Oncol 15(8):2120–2128. https://doi.org/10.1245/s10434-008-9961-7
Galizia G, Gemei M, Orditura M, Romano C, Zamboli A, Castellano P, Mabilia A, Auricchio A, De Vita F, Del Vecchio L, Lieto E (2013) Postoperative detection of circulating tumor cells predicts tumor recurrence in colorectal cancer patients. J Gastrointest Surg 17 (10):1809–1818. https://doi.org/10.1007/s11605-013-2258-6
Huang XZ, Gao P, Song YX, Sun JX, Chen XW, Zhao JH, Liu J, Xu HM, Wang ZN (2014) Relationship between circulating tumor cells and tumor response in colorectal cancer patients treated with chemotherapy: a meta-analysis. BMC cancer 14. doi: Artn 976. https://doi.org/10.1186/1471-2407-14-976
Hardingham JE, Grover P, Winter M, Hewett PJ, Price TJ, Thierry B (2015) Detection and clinical significance of circulating tumor cells in colorectal cancer-20 years of progress. Mol Med 21:S25–S31. https://doi.org/10.2119/molmed.2015.00149
Liu H, Zhang X, Li J, Sun B, Qian H, Yin Z (2015) The biological and clinical importance of epithelial-mesenchymal transition in circulating tumor cells. J Cancer Res Clin Oncol 141(2):189–201. https://doi.org/10.1007/s00432-014-1752-x
Silva VSE, Chinen LTD, Abdallah EA, Damascena A, Paludo J, Chojniak R, Dettino ALA, de Mello CAL, Alves VS, Fanelli MF (2016) Early detection of poor outcome in patients with metastatic colorectal cancer: tumor kinetics evaluated by circulating tumor cells. OncoTargets Therapy 9:7503–7513. https://doi.org/10.2147/Ott.S115268
Funding
The present study was supported by the Seed Founding of the Shanghai Ninth People’s Hospital affiliated to Shanghai Jiao Tong University School of Medicine (Grant No. JYZZ008), Shanghai Shen-Kang Hospital Development Foundation (16CR4030A to B.J) and Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant (Grant No. 20172017).
Author information
Authors and Affiliations
Contributions
Bin Jiang and Yanjie Zhang designed the study. Haihua Yuan, Lili Wang, and Feng Liu collected the samples. Wenying Zhang, Jiongyi Wang, Meiling Wang, and Xiaohua Hu followed up the OS and PFS of the patients. Haihua Yuan and Lili Wang analyzed the data, and Lili Wang performed the statistical analyses. Lili Wang wrote the manuscript with Haihua Yuan’s assistance, and final version of the manuscript was approved by all the authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Shanghai Ninth People’s Hospital affiliated to Shanghai Jiao Tong University School of Medicine.
Patient consent for publication
The authors declare that the patients have provided written informed consent for the purpose of publication.
Competing interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wang, L., Zhou, S., Zhang, W. et al. Circulating tumor cells as an independent prognostic factor in advanced colorectal cancer: a retrospective study in 121 patients. Int J Colorectal Dis 34, 589–597 (2019). https://doi.org/10.1007/s00384-018-03223-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-03223-9