Abstract
Purpose
In a preliminary study, we found that lancemaside A, which is a main constituent of Codonopsis lanceolata used as an herbal medicine for inflammatory diseases, potently inhibits lipopolysaccharide (LPS)-stimulated, TLR-4-linked NF-κB activation of NF-κB luciferase reporter gene-transfected 293-hTLR4-hemagglutinin (HA) cells. Therefore, we investigated its inhibitory effect in 2,4,6-trinitrobenzenesulfonic acid (TNBS)-induced colitis in mice.
Methods
We measured the ability of lancemaside A to inhibit LPS-stimulated, TLR-4-linked NF-κB activation in human embryonic kidney (HEK) cells, as well as to inhibit colitis outcomes in TNBS-induced colitis in mice. We also measured levels of the inflammatory markers, interleukin (IL)-1β, tumor necrosis factor (TNF)-α, and IL-6, and their transcription factor, NF-κB, in intestinal mucosa by enzyme-linked immunosorbent assay and immunoblotting.
Result
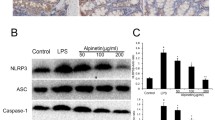
Intrarectal treatment of TNBS in mice caused colon shortening and also increased colonic expression of IL-1β, IL-6, and TNF-α expression. Oral administration of lancemaside A (10 and 20 mg/kg), inhibited colon shortening and myeloperoxidase activity in TNBS-induced colitic mice and also decreased colonic expression of IL-1β, IL-6, and TNF-α. Lancemaside A inhibited NF-κB activation induced by TNBS, as well as the expression of cyclooxygenase 2 and TLR-4. Lancemaside A also reduced the activity of intestinal bacterial β-glucuronidase that was induced by TNBS.
Conclusions
Lancemaside A ameliorates colitis via inhibition of TLR-4-linked NF-κB activation.





Similar content being viewed by others
Abbreviations
- IBD:
-
inflammatory bowel disease
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- ECL:
-
enhanced chemiluminescence
- ELISA:
-
enzyme-linked immunosorbent assay
- HA:
-
hemagglutinin
- HEK:
-
human embryonic kidney
- IL:
-
interleukin
- LPS:
-
lipopolysaccharide
- RIPA:
-
radio-immunoprecipitation assay
- TLR:
-
toll-like receptor
- TNBS:
-
2,4,6-trinitrobenzenesulfonic acid
- TNF:
-
tumor necrosis factor
References
Benno P, Leijonmarck CE, Monsen U, Uribe A (1993) Functional alteration of the microflora in patients with ulcerative colitis. Scand J Gastroenterol 28:839–844
Berrebi D, Languepin J, Ferkdadji L, Foussat A, De Lagausie P, Paris R, Emilie D, Mougenot JF, Cezard JP, Navarro J, Peuchmaur M (2003) Cytokines, chemokine receptors, and homing molecule distribution in the rectum and stomach of pediatric patients with ulcerative colitis. J Pediatr Gastroenterol Nutr 37:300–308
Gorbach SL, Nahas L (1968) Studies of intestinal microflora. V. Fecal microbial ecology in ulcerative colitis and regional enteritis, relationship to severity of disease and chemotherapy. Gastroenterology 54:575–587
Binder V (2004) Epidemiology of IBD during the twentieth century: an integrated view. Best Pract Res Clin Gastroenterol 18:463–479
Chandran P, Satthaporn Robins A, Eremin O (2003) Inflammatory bowel disease: dysfunction of GALT and gut bacterial flora (II). Surgeon 1:125–136
Hill MJ, Drasar BS (1975) The normal colonic bacterial flora. Gut 16:318–323
Simon GL, Gorbach SL (1984) Intestinal flora in health and disease. Gastroenterology 86:174–193
Chung KT, Fulk GE, Slein MW (1975) Tryptophanase of fecal flora as a possible factor in the etiology of colon cancer. J Natl Cancer Inst 54:1073–1078
Ganguly NK, Kingham JG, Lloyd B, Lloyd RS, Price CP, Triger DR, Wright R (1978) Acid hydrolases in monocytes from patients with inflammatory bowel disease, chronic liver disease, and rheumatoid arthritis. Lancet 1(8073):1073–1075
Rhodes JM, Gallimore R, Elias E, Allan RN, Kennedy JF (1985) Fecal mucus degrading glycosidase in ulcerative colitis and Crohn’s disease. Gut 26:761–765
Jung HC, Eckmann I, Yang SK, Panja A, Fierer J, Morzycka-Worblewska E, Kagnoff MF (1995) A distinct array of proinflammatory cytokine is expressed in human colon epithelia cells in response to bacterial invasion. J Clin Invest 95:55–65
Chow JC, Young DW, Golenbock DT, Christ WJ, Gusovsky F (1999) Toll-like receptor-4 mediates lipolysaccharide-induced signal transduction. J Biol Chem 274:10689–10692
Ingalls RR, Heine H, Lien E, Yoshimura A, Glenbock D (1999) Lipopolysaccharide recognition, CD14, and lipopolysaccharide receptors. Infect Dis Clin North Am 13:341–353
Cario E, Pldolsky DK (2000) Differential alteration in intestinal epithelial cell expression of toll-like receptor 3 (TLR3) and TLR4 in inflammatory bowel disease. Infect Immun 68:7010–7017
Poltorak A, He X, Smirnova I, Liu M, Huffel CV, Du X, Birdwell D, Alejos E, Silva M, Galanos C, Freudenberg M, Ricciardi-Castagnoli P, Layton B, Beutler B (1998) Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 282:2085–2088
Mizoguchi A, Mizoguchi E (2008) Inflammatory bowel disease, past, present and future: lessons from animal models. J Gastroenterol 43:1–17
Ushijima M, Komoto N, Sugizono Y, Mizuno I, Sumihiro M, Ichikawa M, Hayama M, Kawahara N, Nakane T, Shirota O, Sekita S, Kuroyanagi M (2008) Triterpene glycosides from the roots of Codonopsis lanceolata. Chem Pharm Bull (Tokyo) 56:308–314
Lee KT, Choi J, Jung WT, Nam JH, Jung HJ, Park HJ (2002) Structure of a new echinocystic acid bisdesmoside isolated from Codonopsis lanceolata roots and the cytotoxic activity of prosapogenins. J Agric Food Chem 50:4190–4193
Xu LP, Wang H, Yuan Z (2008) Triterpenoid saponins with anti-inflammatory activity from Codonopsis lanceolata. Planta Med 74:1412–1415
Fukata M, Chen A, Klepper A, Krishnareddy S, Vamadevan AS, Thomas LS, Xu R, Inoue H, Arditi M, Dannenberg AJ, Abreu MT (2006) Cox-2 is regulated by toll-like receptor-4 (TLR4) signaling: role in proliferation and apoptosis in the intestine. Gastroenterology 131:862–877
Hollenbach E, ViethM RA, Neumann M, Malfertheiner P, Naumann M (2005) Inhibition of RICK/Nuclear factor-kB and p38 signalling attenuates the inflammatory response in a murine model of Crohn’s disease. J Biol Chem 280:14981–14988
Mullane KM, Kraemer R, Smith B (1985) Myeloperoxidase activity as a quantitative assessment of neutrophil infiltration into ischemic myocardium. J Pharmacol Methods 14:157–167
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254
Shin YW, Bae EA, Kim SS, Lee YC, Kim DH (2005) Effect of ginsenoside Rb1 and compound K in chronic oxazolone-induced mouse dermatitis. Int Immunopharmacol 5:1183–1191
Harris F, Phoenix DA (1997) An investigation into the ability of C-terminal homologues of Escherichia coli low molecular mass penicillin-binding proteins 4, 5 and 6 to undergo membrane interaction. Biochimie 79:171–174
Duchmann R, Kaiser I, Hermann E, Mayet W, Ewe K, Meyer zum Büschenfelde KH (1995) Tolerance exists towards resident intestinal flora but is broken in active inflammatory bowel disease. Clin Exp Immunol 102:448–455
Bukovská A, Cikos S, Juhás S, Il'ková G, Rehák P, Koppel J (2007) Effects of a combination of thyme and oregano essential oils on TNBS-induced colitis in mice. Mediators Inflamm 2007:23296
Bai A, Lu N, Guo Y, Fan X (2008) Tanshinone IIA ameliorates trinitrobenzene sulfonic acid (TNBS)-induced murine colitis. Dig Dis Sci 53:421–428
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Joh, EH., Lee, IA., Han, SJ. et al. Lancemaside A ameliorates colitis by inhibiting NF-κB activation in TNBS-induced colitis mice. Int J Colorectal Dis 25, 545–551 (2010). https://doi.org/10.1007/s00384-009-0858-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-009-0858-0