Abstract
Purpose
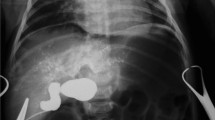
This study aimed to evaluate the effect of prenatal diagnosis at different gestational times on the clinical features of patients with choledochal cysts (CDCs).
Methods
Medical records of patients with prenatally diagnosed CDCs admitted to our hospital (April 2013–April 2018) were retrospectively reviewed. The clinical characteristics and pathological CDC features were analyzed.
Results
Two hundred eighteen cases were included. Patients were divided into two groups. Group 1 and group 2 had a prenatal diagnosis at ≤ 27 weeks of gestation (second trimester of gestation, n = 157) and > 27 weeks (third trimester of gestation, n = 61), respectively. The incidence of jaundice and the TBIL, IBIL and GGT levels were higher in Group 1 (P = 0.021, P = 0.029, P = 0.042, P = 0.007, respectively). The maximum cyst diameter at the time of surgery was larger in Group 1 (P = 0.015). An association study showed that the time of prenatal diagnosis was negatively correlated with the maximum cyst diameter both postnatally (r = − 0.223, P = 0.001) and at the time of surgery (r = − 0.268, P < 0.001).
Conclusion
Unlike patients diagnosed at a late prenatal age, patients diagnosed at an early prenatal age tend to present clinical symptoms (jaundice, manifested as high indirect bilirubin), hepatic function damage, and large cysts at the time of surgery.

Similar content being viewed by others
Abbreviations
- CDC:
-
Choledochal cyst
References
Sanna E, Loukogeorgakis S, Prior T et al (2019) Fetal abdominal cysts: antenatal course and postnatal outcomes. J Perinat Med 47(4):418–421
Friedmacher F, Ford KE, Davenport M (2019) Choledochal malformations: global research, scientific advances and key controversies. Pediatr Surg Int 35(3):273–282
Urushihara N, Fukumoto K, Yamoto M et al (2018) Characteristics, management, and outcomes of congenital biliary dilatation in neonates and early infants: a 20-year, single-institution study. J Hepatobiliary Pancreat Sci 25(12):544–549
Diao M, Li L, Cheng W (2011) Congenital biliary dilatation may consist of 2 disease entities. J Pediatr Surg 46(8):1503–1509
Todani T, Watanabe Y, Toki A et al (2003) Classification of congenital biliary cystic disease: special reference to type Ic and IVA cysts with primary ductal stricture. J Hepatobiliary Pancreat Surg 10(5):340–344
Diao M, Li L, Cheng W (2020) Timing of choledochal cyst perforation. Hepatology 71(2):753–756
Diao M, Li L, Cheng W (2012) Timing of surgery for prenatally diagnosed asymptomatic choledochal cysts: a prospective randomized study. J Pediatr Surg 47(3):506–512
Marchitelli G, Stirnemann J, Acanfora MM et al (2015) Prenatal diagnosis of intra-abdominal cystic lesions by fetal ultrasonography: diagnostic agreement between prenatal and postnatal diagnosis. Prenat Diagn 35(9):848–852
Yu P, Dong N, Pan YK et al (2022) Comparison between cystic biliary atresia and choledochal cyst: a clinical controlled study. Pediatr Surg Int 38(1):109–114
Ando K, Miyano T, Kohno S et al (1998) Spontaneous perforation of choledochal cyst: a study of 13 cases. Eur J Pediatr Surg 8(1):23–25
Chiang L, Chui CH, Low Y et al (2011) Perforation: a rare complication of choledochal cysts in children. Pediatr Surg Int 27(8):823–827
Khalil A, Cooke PC, Mantovani E et al (2014) Outcome of first-trimester fetal abdominal cysts: cohort study and review of the literature. Ultrasound Obstet Gynecol 43(4):413–419
Weng R, Hu W, Cai S et al (2016) Prenatal diagnosis and prognosis assessment of congenital choledochal cyst in 21 cases. J Obstet Gynaecol 36(3):324–327
Cochran ED, Lazow SP, Kim AG et al (2022) The in-utero diagnosis of choledochal cyst: can postnatal imaging predict benefit from early surgical intervention? J Matern Fetal Neonatal Med 35(6):1070–1074
Guan X, Li J, Wang Z et al (2022) Timing of operation in children with a prenatal diagnosis of choledochal cyst: a single-center retrospective study. J Hepatobiliary Pancreat Sci 29(12):1308–1315
Nambirajan L, Taneja P, Singh MK et al (2000) The liver in choledochal cyst. Trop Gastroenterol 21(3):135–139
Cass DL (2021) Fetal abdominal tumors and cysts. Transl Pediatr 10(5):1530–1541
Sugandhi N, Agarwala S, Bhatnagar V et al (2014) Liver histology in choledochal cyst- pathological changes and response to surgery: the overlooked aspect? Pediatr Surg Int 30(2):205–211
Gong ZH, Xiao X, Chen L (2007) Hepatic fibrosis with choledochal cyst in infants and children - an immunohistochemical assessment. Eur J Pediatr Surg 17(1):12–16
Fumino S, Higuchi K, Aoi S et al (2013) Clinical analysis of liver fibrosis in choledochal cyst. Pediatr Surg Int 29(11):1097–1102
Madadi-Sanjani O, Wirth TC, Kuebler JF et al (2019) Choledochal cyst and malignancy: a plea for lifelong follow-up. Eur J Pediatr Surg 29(2):143–149
Funding
The project is supported by Research Unit of Minimally Invasive Pediatric Surgery on Diagnosis and Treatment, Chinese Academy of Medical Sciences 2021RU015. No. 2021-I2M-5-016.
Author information
Authors and Affiliations
Contributions
Conception and design: Long Li, Mei Diao, Anxiao Ming, Dan Yang; Analysis and interpretation of data: Yu Tian, Ruyue Gao, Dan Yang; Drafting of the manuscript: Dan Yang; Critical revision of the manuscript for important intellectual content: Long Li, Mei Diao, Xianghui Xie; All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, D., Li, L., Diao, M. et al. Prenatal diagnosis at different gestational times and clinical features of choledochal cysts: a single tertiary center report. Pediatr Surg Int 39, 105 (2023). https://doi.org/10.1007/s00383-023-05374-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05374-5