Abstract
Purpose
In general, patients with anorectal malformation (ARM) undergo surgical treatment at around 6 months of age in Japan. We aimed to clarify whether the timing of a definitive operation affects the long-term bowel function.
Methods
Patient data were collected from 1984 to 2007. Fifty-two male patients with high- and intermediate-type ARM were enrolled. Patients were classified into two groups based on their operative period: the early group (EG) underwent anorectoplasty at < 5 months of age (n = 22); the late group (LG) underwent anorectoplasty at ≥ 5 months (n = 30). The bowel function was evaluated at 3, 5, 7, 9, and 11 years of age using the evacuation score (ES) of the Japan Society of Anorectal Malformation Study Group.
Results
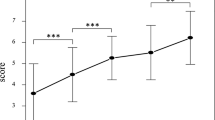
The total score and four functional outcomes improved chronologically with age. The constipation score in the EG showed significantly better improvement in comparison to the LG. The total score and the incontinence score in the EG were significantly higher than those in the LG at 11 years of age.
Conclusion
The long-term bowel function in the EG was better than that in the LG. Anorectoplasty at an early age was important for achieving a better postoperative bowel function in ARM patients.


Similar content being viewed by others

References
Pena A, Hong A (2000) Advances in the management of anorectal malformations. Am J Surg 180(5):370–376
Stephens FD (1953) Imperforate rectum; a new surgical technique. Med J Aust 1(6):202–203
Harumatsu T, Murakami M, Yano K, Onishi S, Yamada K, Yamada W, Masuya R, Kawano T, Machigashira S, Nakame K, Mukai M, Kaji T, Ieiri S (2019) The change over time in the postoperative bowel function in male anorectal malformation patients who underwent sacroperineal anorectoplasty and sacroabdominoperineal anorectoplasty. Pediatr Surg Int 35(10):1109–1114
Onishi S, Nakame K, Yamada K, Yamada W, Kawano T, Mukai M, Kaji T, Ieiri S (2016) Long-term outcome of bowel function for 110 consecutive cases of Hirschsprung’s disease: comparison of the abdominal approach with transanal approach more than 30years in a single institution—is the transanal approach truly beneficial for bowel function? J Pediatr Surg 51(12):2010–2014
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48(3):452–458
Albanese CT, Jennings RW, Lopoo JB, Bratton BJ, Harrison MR (1999) One-stage correction of high imperforate anus in the male neonate. J Pediatr Surg 34(5):834–836
Liu G, Yuan J, Geng J, Wang C, Li T (2004) The treatment of high and intermediate anorectal malformations: one stage or three procedures? J Pediatr Surg 39(10):1466–1471
Moore TC (1990) Advantages of performing the sagittal anoplasty operation for imperforate anus at birth. J Pediatr Surg 25(2):276–277
Pena A, Devries PA (1982) Posterior sagittal anorectoplasty: important technical considerations and new applications. J Pediatr Surg 17(6):796–811
Pena A, Migotto-Krieger M, Levitt MA (2006) Colostomy in anorectal malformations: a procedure with serious but preventable complications. J Pediatr Surg 41(4):748–756 (discussion 748-756)
Pena A (1993) Management of anorectal malformations during the newborn period. World J Surg 17(3):385–392
Japanese multicenter study group on male high imperforate anus (2013) Multicenter retrospective comparative study of laparoscopically assisted and conventional anorectoplasty for male infants with rectoprostatic urethral fistula. J Pediatr Surg 48(12):2383–2388
Rintala RJ, Lindahl HG (1999) Posterior sagittal anorectoplasty is superior to sacroperineal–sacroabdominoperineal pull-through: a long-term follow-up study in boys with high anorectal anomalies. J Pediatr Surg 34(2):334–337
Rintala R, Lindahl H, Marttinen E, Sariola H (1993) Constipation is a major functional complication after internal sphincter-saving posterior sagittal anorectoplasty for high and intermediate anorectal malformations. J Pediatr Surg 28(8):1054–1058
Langemeijer RA, Molenaar JC (1991) Continence after posterior sagittal anorectoplasty. J Pediatr Surg 26(5):587–590
Kyrklund K, Pakarinen MP, Koivusalo A, Rintala RJ (2014) Long-term bowel functional outcomes in rectourethral fistula treated with PSARP: controlled results after 4–29 years of follow-up: a single-institution, cross-sectional study. J Pediatr Surg 49(11):1635–1642
Rintala RJ, Lindahl HG (2001) Fecal continence in patients having undergone posterior sagittal anorectoplasty procedure for a high anorectal malformation improves at adolescence, as constipation disappears. J Pediatr Surg 36(8):1218–1221
Borg H, Holmdahl G, Doroszkievicz M, Sillen U (2014) Longitudinal study of lower urinary tract function in children with anorectal malformation. Eur J Pediatr Surg 24(6):492–499
Pena A (1995) Anorectal malformations. Semin Pediatr Surg 4(1):35–47
Pena A, Guardino K, Tovilla JM, Levitt MA, Rodriguez G, Torres R (1998) Bowel management for fecal incontinence in patients with anorectal malformations. J Pediatr Surg 33(1):133–137
Bliss DP Jr, Tapper D, Anderson JM, Schaller RT Jr, Hatch EI, Morgan A, Hall DG, Sawin RS (1996) Does posterior sagittal anorectoplasty in patients with high imperforate anus provide superior fecal continence? J Pediatr Surg 31(1):26–30 (discussion 30-22)
Nixon HH, Puri P (1977) The results of treatment of anorectal anomalies: a thirteen to twenty year follow-up. J Pediatr Surg 12(1):27–37
Hassink EA, Rieu PN, Severijnen RS, vd Staak FH, Festen C (1993) Are adults content or continent after repair for high anal atresia? A long-term follow-up study in patients 18 years of age and older. Ann Surg 218(2):196–200
Rintala R, Mildh L, Lindahl H (1994) Fecal continence and quality of life for adult patients with an operated high or intermediate anorectal malformation. J Pediatr Surg 29(6):777–780
Acknowledgements
We thank Mr. Brain Quinn for his comments and help with the manuscript. This study was supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JSPS: 20K08934, 20K17558, 20K10403, 20K08933, 19K10485, 19K09150, 19K09078, 19K03084, 19K18061, 19K17304, 19K18032, 18K08578, 18K16262 17K10555, 17K11514, 17K10183, 17K11515, 16K10466, 16K10094, 16K10095, 16K10434, 16H07090), research grant from The Mother and Child Health Foundation and research grant from the Kawano Masanori Memorial Public Interest Incorporated Foundation for Promotion of Pediatrics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Ethical approval
This study was performed in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects by the Ministry of Health, Labour, and Welfare of Japan in 2014. The study complied with the 1964 Declaration of Helsinki (revised in 2013) and was approved by the local ethics committee of our institution (registration number: 27-119). All participants or their parents provided their informed consent for involvement in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harumatsu, T., Kaji, T., Nagano, A. et al. Early definitive operation for patients with anorectal malformation was associated with a better long-term postoperative bowel function. Pediatr Surg Int 37, 445–450 (2021). https://doi.org/10.1007/s00383-020-04842-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04842-6