Abstract
Objective
The laparoscopically-assisted anorectal pull-through (LAARP) for recto-bladderneck and recto-prostatic anorectal malformations (RB/RP-ARMs) is believed to improve patient outcomes. We performed a systematic review of the effect of LAARP on postoperative mucosal prolapse and defecation dysfunction.
Methods
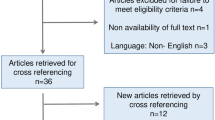
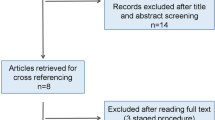
A comprehensive search of MEDLINE, EMBASE, CENTRAL, and grey literature was performed (2000–2014). Full-text screening, data abstraction and quality appraisal were conducted in duplicate. Included studies reported a primary diagnosis of RB/RP-ARM and compared LAARP versus open repair (OPEN).
Results
From 3681 retrieved articles, 7 studies enrolling 187 patients were analyzed. One was a randomized control trial, 6 were retrospective observational studies, and all were single-centre. The majority were of poor-moderate quality (MINORS scores: mean 16.42 (SD 2.225) out of 24). Mucosal prolapse was not significantly different after LAARP versus OPEN (p = 0.18). Defecation outcomes were inconsistently reported but were no different between LAARP and OPEN for either children >3 years old (p = 0.84), or all ages combined (p = 0.11).
Conclusion
We found no significant difference in rates of mucosal prolapse or defecation scores for LAARP compared to OPEN for children with RB/RP-ARMs. However, studies are small and of poor-moderate quality and results are heterogeneous. Comprehensive, standardized, reliable reporting is necessary to guide practice and inform postoperative guidelines.
Level of evidence
1c.







Similar content being viewed by others
References
Coran AG, Caldamone A, Adzick NS, Krummel TM, Laberge JM, Shamberger R (2012) Pediatric Surgery, 7th edn. Mosby, St. Louis
Brenner E (1915) Congenital defects of the anus and rectum. Surg Gynecol Obstet 220:579–598
Stephens FD, Smith ED, Paoul NW (1998) Anorectal malformations in children: update 1988. March of Dimes Birth Defect Foundation Original series, Vol. 24 (4). New York, NY: Alan R. Liss Inc
Holschneider A, Hutson J, Pena A et al (2005) Preliminary report on the International Conference for the Development of Standards for the Treatment of Anorectal Malformations. J Pediatr Surg 40:1521–1526
Levitt MA, Pena A (2007) Anorectal malformations. Orphanet J Rare Dis 2:33–45
Bischoff A, Tovilla M (2010) A practical approach to the management of pediatric fecal incontinence. Semin Pediatr Surg 19:154–159
deVries PA, Pena A (1982) Posterior sagittal anorectoplasty. J Pediatr Surg 17:638–643
Okada A, Kamata S, Fukuzawa M et al (1992) Anterior sagittal anorectoplasty for rectovestibular and anovestibular fistula. J Pediatr Surg 27:85–88
Willital GH (1998) Endosurgical intrapuborectal reconstruction of high anorectal anomalies. Pediatr Endosurg Innov Tech 2:5–11
Georgeson KE, Inge TH, Albanese CT (2000) Laparoscopically assisted anorectal pull-through for high imperforate anus—a new technique. J Pediatr Surg 35:927–930
Attard JP, MacLean AR (2007) Adhesive small bowel obstruction: epidemiology, biology and prevention. Can J Surg 504:291–300
Ponsky TA, Rothenberg SS (2008) Minimally invasive surgery in infants less than 5 kg: experience of 649 cases. Surg Endosc 22:2214–2219
Walsh PC, Schlegel PN (1998) Radical pelvic surgery with preservation of sexual function. Ann Surg 208:391–400
Bischoff A, Levitt MA, Peña A (2011) Laparoscopy and its use in the repair of anorectal malformations. J Pediatr Surg 46:1609–1617
Li X, Zhang J, Sang L et al (2011) Laparoscopic versus conventional appendectomy- a meta-analysis of randomized controlled trials. BMC Gastroenterol 10:129–136
Lin CL, Wong KKY, Lan LC et al (2003) Earlier appearance and higher incidence of the rectoanal relaxation reflex in patients with imperforate anus repaired with laparoscopically assisted anorectoplasty. Surg Endosc 17:1646–1649
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Braga LH, Mijovic H, Farrokhyar F et al (2013) Antibiotic prophylaxis for urinary tract infections in antenatal hydronephrosis. Pediatrics 131:e251–e261
Holschneider AM, Hutson JM (2006) Anorectal Malformations in Children. Springer, Heidelberg
Kelly JH (1972) The clinical and radiological assessment of anal continence in childhood. Aust NZ J Surg 42:62–63
Rintala RJ, Lindahl H (1995) Is normal bowel function possible after repair of intermediate and high anorectal malformations? J Pediatr Surg 30:491–494
Bai Y, Yuan Z, Wang W et al (2000) Quality of life for children with fecal incontinence after surgically corrected anorectal malformation. J Pediatr Surg 35:462–464
Hassnick EA, Rieu PN, Brugman AT et al (1994) Quality of life after operatively corrected high anorectal malformation: a long-term follow-up study of patients aged 18 years and older. J Pediatr Surg 29:773–776
Higgens JP (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 15:1539–1558
Steward DJ (1982) Preterm infants are more prone to complications following minor surgery than are term infants. Anesthesiology 56:304–306
Sun L (2010) Early childhood general anaesthesia exposure and neurocognitive development. Brit J Anaesth 105:i61–i68
Boemers T, Beek F, van Gool J et al (1996) Urologic problems in anorectal malformations. Part 1: urodynamic findings and significance of sacral anomalies. J Pediatr Surg 31:407–410
Boemers T, de Jong T, van Gool J et al (1996) Urologic problems in anorectal malformations. Part 2: functional urologic sequelae. J Pediatr Surg 31:634–637
Higgins JPT, Green S (2009) Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2009. Available from www.cochrane-handbook.org; Accessed August 25, 1014
Grade Working Group (2004) Grading quality of evidence and strength of recommendations. BMJ 328:1490–1494
GRADEpro (2008) [Computer program]. Version 3.2 for Windows. Jan Brozek, Andrew Oxman, Holger Schünemann
Fleiss JL (1981) Statistical methods for rates and proportions, 2nd edn. John Wiley, New York
IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp
Review Manager (RevMan) (2008) [Computer program]. Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration
Bailez MM, Cuenca ES, Mauri V et al (2011) Outcome of males with high anorectal malformations. J Pediatr Surg 46:473–477
England RJ, Warren SL, Bezuidenhout L et al (2012) Laparoscopic repair of anorectal malformations at the Red Cross War Memorial Children’s Hospital: taking stock. J Pediatr Surg 47:565–570
Kimura O, Iwai N, Sasaki Y et al (2010) Laparoscopic versus open abdominoperineal rectoplasty for infants with high-type anorectal malformation. J Pediatr Surg 45:2390–2393
Koga H, Miyano G, Takahashi T et al (2010) Comparison of anorectal angle and continence after Georgeson and Peña procedures for high/intermediate imperforate anus. J Pediatr Surg 45:2394–2397
Tong Q, Tang S, Pu J et al (2011) Laparoscopically assisted anorectal pull-through for high imperforate anus in infants: intermediate results. J Pediatr Surg 46:1578–1586
Yang J, Zhang W, Feng J et al (2009) Comparison of clinical outcomes and anorectal manometry in patients with congenital anorectal malformations treated with posterior sagittal anorectoplasty and laparoscopically assisted anorectal pull through. J Pediatr Surg 44:2380–2383
Wood AH (1993) Pulmonary surfactant therapy. NEJM 328:861–868
Veyrac C, Couture A, Saguintaah M et al (2004) MRI of fetal GI tract abnormalities. Abdom Imaging 29:411–420
Al-Hozaim O, Al-Maary J, AlQahtani A et al (2010) Laparoscopic-assisted anorectal pull-through for anorectal malformations: a systematic review and the need for standardization of outcome reporting. J Pediatr Surg 45:1500–1504
Beck CA (2009) Selection bias in observational studies: out of control? Neurology 72:108–109
Stoll C, Alembik Y, Dott B et al (2007) Associated malformations in patients with anorectal anomalies. Eur J Med Genet 50:281–290
Levitt MA, Patel M, Rodriguez G et al (1997) The tethered spinal cord in patients with anorectal malformations. J Pediatr Surg 32:462–468
Belizon A, Levitt M, Shoshany G et al (2005) Rectal prolapse following posterior sagittal anorectoplasty for anorectal malformations. J Pediatr Surg 40:192–196
Laberge JM (1997) The anterior sagittal approach to the treatment of anorectal malformations: evolution of the Mollard approach. Semin Pediatr Surg 6:196–203
Hartman EE, Oort FJ, Aronson DC et al (2011) Quality of life and disease-specific functioning of patients with anorectal malformations or Hirschsprung’s disease: a review. Arch Dis Child 96:398–406
Diseth TH, Egeland T, Emblem R (1998) Effects of anal invasive treatment and incontinence on mental health and psychosocial functioning of adolescents with Hirschsprung’s disease and low anorectal anomalies. J Pediatr Surg 33:468–475
Langemeijer RA, Molenaar JC (1991) Continence after posterior sagittal anorectoplasty. J Pediatr Surg 26:587–590
deVries PA, Cox KL (1985) Surgery of anorectal anomalies. Surg Clin North Am 65:1139–1169
Rintala R, Lindahl H, Louhimo I (1991) Anorectal malformations - results of treatment and long-term follow-up in 208 patients. Peditri Surg Int 6:36–41
Levitt MA, Pena A (2005) Outcomes from the correction of anorectal malformation. Curr Opin Pediatr 17:394–401
Hassett S, Snell S, Hughes-Thomas A et al (2009) 10-Year outcome of children born with anorectal malformation, treated by posterior sagittal anorectoplasty, assessed according to the Krickenbeck classification. J Pediatr Surg 44:399–403
Rintala RJ, Pakarinen MP (2008) Imperforate anus: long- and short-term outcome. Semin Pediatr Surg 17:79–89
Duepree HJ, Senagore AJ, Delaney CP et al (2003) Does means of access affect the incidence of small bowel obstruction and ventral hernia after bowel resection? Laparoscopy versus laparotomy. J Am Coll Surgeons 197:177–181
Pena A, Hong A (2000) Advances in the management of anorectal malformations. Am J Surg 80:370–376
Vinnicombe SJ, Good CD, Hall CM (1996) Posterior urethral diverticula: a complication of surgery for high anorectal malformations. Pediatr Radiol 26:120–126
Lopez PJ, Guelfand M, Angel L et al (2010) Urethral diverticulum after laparoscopically-assisted anorectal pull-through (LAARP) for anorectal malformation: is resection of the diverticulum always necessary? Arch Esp Urol 63:297–301
Koga H, Okazaki T, Yamataka A et al (2005) Posterior urethral diverticulum after laparoscopic-assisted repair of high-type anorectal malformation in a male patient: surgical treatment and prevention. Pediatr Surg Int 21:58–60
Alam S, Lawal TA, Pena A et al (2011) Acquired posterior urethral diverticulum following surgery for anorectal malformations. J Pediatr Surg 46:1231–1235
Sheldon CA, Gilbert A, Lewis AG et al (1994) Surgical implications of genitourinary anomalies in patients with imperforate anus. J Urol 152:196–199
Choby BA, George S (2008) Toilet Training. Am Fam Physician 8:1059–1064
Witvliet MJ, Slaar A, Heij HA et al (2013) Qualitative analysis of studies concerning quality of life in children and adults with anorectal malformations. J Pediatr Surg 48:372–379
Grano C, Aminoff A, Lucidi F et al (2011) Long-term disease-specific quality of life in adult anorectal malformation patients. J Pediatr Surg 46:691–698
Acknowledgments
The authors would like to thank Neera Bhatnagar for her assistance with the search strategy, and Molly Barber for her assistance with editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shawyer, A.C., Livingston, M.H., Cook, D.J. et al. Laparoscopic versus open repair of recto-bladderneck and recto-prostatic anorectal malformations: a systematic review and meta-analysis. Pediatr Surg Int 31, 17–30 (2015). https://doi.org/10.1007/s00383-014-3626-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-014-3626-3